Cutting Edge Structural Interventions | TEER: New Hope For Patients With Mitral Regurgitation

I love my job as an interventional and structural cardiologist, especially because of the variety of procedures I perform. However, if I was pressed to choose only one procedure to do for the rest of my life, I would choose mitral valve transcatheter edge-to-edge repair (TEER).
TEER technologies have transformed many lives since their inception in the late 1990s. A 55-year-old woman from Caracas, Venezuela, was the first patient to undergo a TEER procedure with the MitraClip device. Since then, more than 115,000 patients across the globe with mitral regurgitation (MR) have been successfully treated.
Two recent developments could lead to more patients benefiting from TEER: a change in national society guideline recommendations and inclusion of TEER for secondary MR in the National Coverage Determination (NCD) released by the Centers for Medicare and Medicaid Services (CMS) in January 2021. This opens the door to insurance coverage for patients meeting the criteria outlined in the NCD.
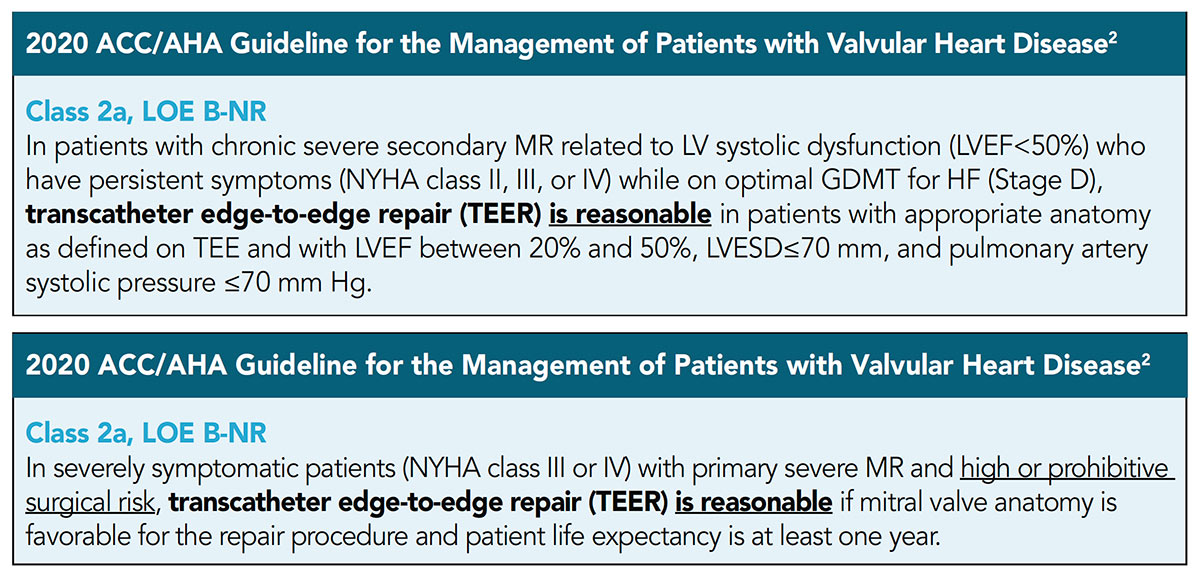
The ACC and American Heart Association (AHA) guideline on valvular heart disease, released in December 2020, included an upgrade in the recommendations for TEER in patients with primary and secondary MR.
For patients with chronic severe primary (also known as degenerative) MR, TEER now has a Class 2a recommendation stating it is reasonable if mitral valve anatomy is favorable for the repair procedure and patient life expectancy is at least one year.1 Previously only patients who were considered prohibitive risk were eligible for therapy with TEER and in those patients it was a Class 2b recommendation.2
In chronic severe secondary (also known as functional) MR, TEER is now considered a Class 2a recommendation in selected patients after they are optimized on guideline-directed medical therapy (GDMT).1 The COAPT inclusion criteria guides patient selection in this setting and includes appropriate anatomy as defined on transesophageal echocardiography and with a left ventricular ejection fraction (LVEF) of 20% to 50%, LV end systolic diameter ≤70 mm and a pulmonary artery systolic pressure ≤70 mm Hg.
The CMS NCD coverage became effective for all hospital discharges on January 19, 2021 and onwards, TEER is now covered for the treatment of symptomatic moderate-to-severe or severe functional MR. Maximally tolerated guideline-directed medical therapy (GDMT) plus cardiac resynchronization therapy, if appropriate, must have already been tried and shown to have failed for the patient.
The landscape has changed quickly because of these developments and potentially thousands of new patients could be treated with this therapy. TEER is a unique procedure requiring a dedicated structural cardiology imager as well as an operator to manipulate the clip device – it is truly a team effort.
Here I share a conversation with my imaging partner, Oscar Peñate, MD, and another with a leader in structural heart disease, Mark Reisman, MD, FACC, who shares his perspective on the past and future of TEER.
A key member of the team is the patient. What does the TEER option mean for them? A pretty quick improvement in quality of life and a return to feeling well and pursuing their usual activities. My patient, Ronald Grimm, is a great example of this improvement. He has lived with heart failure for many years and then MR was diagnosed two years ago, what he called leaky valves. He became sluggish and lost his energy, and as he said, it was like he had lost his drive and he had to push hard to get little things done. Mr. Grimm shared that not only was he happy to be able to go home the day after the procedure, but that as soon as he woke from anesthesia, he could feel a difference: the constant gurgling and spasm-like feeling was gone and his chest was quiet and his heart was smooth. From there, it was a steady and speedy return to his old self.
Reisman on TEER
Mark Reisman, MD, is the new director of Structural Heart Disease at New York Presbyterian/Weill Cornell Medicine. A leader in cardiac innovations for over three decades, he continues to dedicate his career to furthering the field of cardiology and valvular heart disease. He strives to ensure every patient benefits from the dizzying array of options available to treat structural heart disease. He is also my mentor and I recently had the opportunity for a Zoom visit to talk about TEER. Here's an excerpt from our conversation.
Krishnan: How did you get interested in the MitraClip device?
Reisman: I've always been interested in emerging therapies and new technologies. I became aware of the MitraClip device early in its infancy and humbly realized how much I did not know about the mitral valve and how this type of device delivered transeptally interacts with the mitral valve. I was blessed to run the health care innovation program at the Swedish Medical Center and then at the University of Washington. I used the cadaver lab to conduct studies to better understand the relational anatomy and pathology of the mitral valve and the MitraClip so I could help train physicians in this space.
I discovered that trying to understand and internalize these concepts helped me become a better physician and teacher.
What do you think are the biggest challenges for TEER technologies moving forwards?
Despite the exponential growth of our knowledge base regarding the mitral valve, there is still much to be discovered. Patient selection remains challenging. I think the story goes beyond MITRA-FR and COAPT. Those randomized trials put the battleship in the correct direction, but the truth may be in the middle. There is something to be said about the significant learning curve of the device and the interplay between the imager and the operator.
Furthermore, we have yet to understand the value of an annuloplasty ring in such patients. Should TEER be performed simultaneously with transcatheter annuloplasty rings? Although no such device is currently approved by the U.S. Food and Drug Administration (FDA), several are in development and require us to re-examine our thought process as we approach patients with severe mitral regurgitation as this is usually the basis for most surgical mitral valve repairs.
Mark, would you please expand on your comments about the interplay between the clip operator and the imager?
This is probably one of the most underappreciated aspects of this technology. TEER requires both the operator(s) and the imager to be truly be in sync with one another and appreciate the other's expertise. The improvement in imaging is what took MitraClip as a technology to the next level – not that we developed an epiphany about the mitral valve or the patient.
You have to allow your imager to learn and make mistakes, just like the operators do, in order to find the intentional movements necessary to get the right image at the right time. I am proud of the relationships I have built with my imaging partner, most recently, Burkhard Mackenson, MD. I always wait to make sure that the imaging physician speaks to the patient's family with me after the case.
What most excites you about the future of TEER?
The tricuspid valve is one of the most satisfying opportunities that we have as interventional cardiologists. Open heart surgery for isolated tricuspid valve disease is sparingly performed due to challenges such as right ventricular failure. However, tricuspid valve disease causes extreme suffering for our patients and remains an area of significant unmet need. Translating our knowledge from the mitral valve to the tricuspid valve will certainly help to catalyze our ability to treat these patients; hopefully, the tricuspid valve will be more forgiving due to the lower pressure in the right side of the heart.
What advice do you have for Fellows in Training and Early Career professionals who are just beginning their journey into practice?
Here are two things I have learned during my journey: every device needs a champion and some of the best physicians practice in the smallest towns. Anyone can make a difference in any practice setting. You don't need to be in a large academic medical center to continue to innovate if that is your passion. There is nothing more powerful than a strong champion for a new technology.
Peñate on Imaging in TEER
Oscar Peñate, MD, a cardiac anesthesiologist for 10+ years at King's Daughters Medical Center, did not have any experience with the MitraClip before his first case in February 2020. Now Peñate is one of the most skilled MitraClip imagers in the country and I'm fortunate that he is my imaging partner for TEER cases.
Krishnan: What is your background and how did you get involved with TEER?
Peñate: As a cardiac anesthesiologist, I've been performing cardiac perioperative transesophageal echocardiography for about 10 years and I am boarded in adult echocardiography. I got involved with TEER last year because my hospital wanted to start a program. I was the only cardiac anesthesiologist on staff then, and this led me to becoming an integral part of the program.
What is the role of the imaging specialist during a TEER?
I see my role as part of the team, working concurrently with the implanting physician to provide adequate imaging to make the procedure a success.
Do you find it challenging to balance your duties as an anesthesiologist and an imager simultaneously?
Typically no, as I'm blessed to have a trusted team of skilled cardiac-focused CRNAs with whom I work. This makes my job a lot easier. In other institutions they have two anesthesiologists – one focused on imaging and another focused on the anesthesia. At our institution, we use a cardiac-focused CRNA and a cardiac anesthesiologist model to remain efficient.
What is the most rewarding aspect of your involvement with the TEER program?
The most rewarding aspect for me is to be an active participant in the decision-making process and to see an immediate result in the patient's quality of life as well as an immediate result on the patient's mitral regurgitation. There are very few things in medicine, I feel, where you can actually see an immediate result and TEER procedures are one of the few where you have this privilege.
Do you talk to the patient's families with the implanting physician after the procedure?
Here at King's Daughters Medical Center, I do have that opportunity. Usually in the anesthesia world, we rarely get involved with meeting with the family to discuss the procedure. I appreciate and enjoy this unique experience at my center and it helps to highlight the contribution we make to patient care.

This article was authored by Sandeep Krishnan, MD, RPVI, FACC, an interventional and structural cardiologist at King's Daughters Medical Center in Ashland, KY.
Clinical Topics: Arrhythmias and Clinical EP, Cardiac Surgery, Heart Failure and Cardiomyopathies, Noninvasive Imaging, Valvular Heart Disease, Implantable Devices, Cardiac Surgery and Arrhythmias, Cardiac Surgery and Heart Failure, Cardiac Surgery and VHD, Acute Heart Failure, Echocardiography/Ultrasound, Mitral Regurgitation
Keywords: ACC Publications, Cardiology Magazine, American Heart Association, Anesthesia, Blood Pressure, Cardiac Resynchronization Therapy, Centers for Medicare and Medicaid Services, U.S., Delivery of Health Care, Echocardiography, Transesophageal, Heart Failure, Heart Valve Diseases, Heart Valve Prosthesis, Hospitals, Insurance Coverage, Knowledge Bases, Learning Curve, Life Expectancy, Medicare, Medicine, Mentors, Middle Aged, Mitral Valve, Mitral Valve Insufficiency, Patient Discharge, Patient Selection, Pulmonary Artery, Quality of Life, RNA, Complementary, Stroke Volume, Spasm, Surgical Instruments, Technology, Tricuspid Valve, United States Food and Drug Administration, Ventricular Function, Left
< Back to Listings