Wearable Technology in 2021: Five Burning Questions Cardiologists Are Asking

Cardiology has long been a specialty with a rich spirit of innovation and early adoption of medical advances after rigorous research. The interest in exploring digital devices and wearable technology for chronic cardiovascular diseases, such as congestive heart failure (HF), coronary artery disease and vascular disease, is no surprise.
Newly developed high-tech digital devices, including wearables and sensors, are capable of transmitting reams of individual physiologic data to sophisticated computer platforms armed with complex algorithms. Rich computational science capabilities, including artificial intelligence and prediction analysis technology, can place individual data in the context of data from thousands or even millions of patients.
This creation of a big data predictive model allows for the use of precision medicine and population health risk stratification. New approaches such as eHealth, which uses information and communications technology to support health and health-related fields, and mHealth, a subcategory of eHealth using mobile and wireless technology, are accelerating the shift to digital health for cardiovascular diseases.
Disease management appeared to be the primary focus of digital health companies from 2011 to 2018. More recently, the focus has shifted to earlier prediction of disease, including detection and prevention.
1. Why now? What's the big deal?
Any large shift in a field begins with interest from various stakeholders long before adoption occurs at the cardiology practice or physician level. When innovators, investors, regulators and payers are all paying attention, physicians should sit up and take note.
Over the past decade, the explosion of interest in digital health has been widely felt across the spectrum of health care stakeholders.
Since the new expedited pathways for digital device approval was rolled out by the U.S. Food and Drug Administration (FDA), venture capital funds have invested billions of dollars, launching thousands of new digital health startups focused on every aspect of the patient and provider health journey.
The Centers for Medicare and Medicaid Services (CMS) started paying for remote physiologic monitoring (RPM) in 2019 and expanded that decision in 2020, building the economic justification of digital health ventures, which will no doubt be of much interest in 2021 and beyond.
COVID-19 changed everything about health care delivery in 2020. Innovative care solutions were sparked by the desire of patients to avoid unnecessary exposure to the novel coronavirus, along with interest in reducing the cost of travel and avoiding long waiting times while increasing communication with clinicians.
Most importantly, the need for fewer face-to-face doctor-patient interactions has accelerated the adoption of remote services and telemedicine. Conservative estimates for telemedicine adoption from 2019 to 2020 suggest an increase of 50- to 175-fold compared with January 2019 levels.
The increase has been significantly enhanced by CMS waivers for certain telehealth regulations.
This newly accepted form of doctor-patient communication creates the immediate need to improve and facilitate vital signs and other physiologic measurements that are difficult to obtain in remote interactions.
Enter the need for wearable technology and platform solutions for distance medical care.
2. What devices should I consider?
The number of wearable devices has exploded in the past five years. Generally, cardiology-related wearables include fitness trackers to digital blood pressure cuffs, weight scales to arrhythmia monitoring systems. Some are connected to a proprietary mobile application, and others are part of a digital solution with a platform that facilitates communication between patients and providers.
Many devices are available directly to consumers and are not FDA-approved. Since many are not considered medical grade (but are vastly popular), the focus here is on reliable devices with accurate data confirmed through rigorous FDA approval.
From a clinician's standpoint, there are several basic parameters that should be present when considering adoption of physiologic monitoring devices. Is the monitoring device part of a platform? Does it include disease-based physiologic measurements for disease monitoring like blood pressure cuffs, weight scales or oxygen sensors for congestive heart failure?
Does the digital device measure a single parameter that requires a proprietary application (app) without integration into a wider electronic health record (EHR) system or other device?
Current wearable devices and systems include:
- EKG monitoring and arrhythmia detection patches, such as ZioPatch from iRhythm Technologies; CAM patch from Bardy Diagnostics; Bioflux monitor from Biotricity, etc.
- Arrhythmia detection, including atrial fibrillation (AFib, with wristwatch devices, such as Apple Watch, Livmor Halo+ System and Garmin FitBit, and smartphone apps, such as Pulse-Smart, Kardia Mobile, ECG Check, etc.
- Physiologic monitoring via a variety of sensors available to measure heart rate, respiratory rate, SpO2, accelerometers (walk speed), heart rate variability, skin temperature, stress and sleep disorder assessment.
- Remote monitoring systems for cardiovascular-focused conditions like those from intelliH, Biofourmis, CareMindr, Current Health, Hello Heart, Livongo, Medical Innovations, Myia, Orma Health, among others, provide actionable data to stratify patient information and inform clinicians in real time.
- Digital stethoscopes like Coala and EKO can assist clinicians in performing a remote physical examination, enhancing the quality of a telemedicine visit. Additionally, for patients with vascular disease, Siren Care has developed smart socks to check temperature changes and alert clinicians of impending lower extremity ulcerations before they become clinically apparent.
All these devices and their platforms or apps must be customized for your patients and practice workflow.
The challenge for today's practicing clinician is which device for which patient? A tailored approach to disease state monitoring is recommended, such as congestive HF monitoring using a blood pressure cuff, weight scale and O2 sensor on platforms from IntelliH or Vivify Health.
AFib detection should use a highly sensitive and specific FDA-approved solution platform to reduce false alarms, which can create confusion for patients.
Available systems like the Livmor Halo system, which provides continuous monitoring for asymptomatic patients, or a short-term monitor patch like iRhythm or spot-check monitors such as AliveCor all detect arrhythmias but require an individualized approach determined by clinicians as best for each patient condition.
3. What am I supposed to do with all the data?

As the population ages, the prevalence of chronic disease continues to rise. Simultaneously, tech-savvy generations continue to look to mobile and remote devices to interact with the health care system, just as they have for other business sectors like banking and commerce.
In addition, improved wireless connections and the introduction of 5G technology for cellular connections enable patients and providers to share large amounts of data almost instantaneously.
This real-time exchange of information reduces episodic care costs by proactively identifying at-risk patients through more frequent physiologic monitoring devices, including wearables and other devices.
With appropriate escalation alerts for data, including high/low parameters for blood pressure, weight, oxygen, heart rate, etc., a portal with clearly identified red, green or yellow color-coded alerts (like many systems have adopted) are the best way to create a workflow escalation from medical assistants to nurse practitioners to physicians.
With this set up, the experience at my center has proven a large amount of data to be very manageable for large panels of patients followed by RPM.
4. Does digital health reduce cost and improve outcomes?
Many different methods have been used to determine the impact of digital health on reducing the cost of treatment in cardiology, including direct and indirect methods. One accepted model is the decision analytic-based health technology approach.
Cost-effectiveness and incremental cost per additional quality-adjusted life year (QALY) are frequently cited to derive the impact of an intervention. Fields such as HF and stroke are commonly studied in this space.
Telehealth and telemedicine services have been the most frequently delivered digital intervention, which includes message services, telephone support, mobile apps, video conferencing, wearable medical devices and remote physiologic monitoring.
The TEMA-HF 1 (TElemonitoring in the MAnagement of Heart Failure) study in patients with severe HF provides some data on the effect on mortality and rehospitalization rates of a telemonitoring-facilitated collaboration between general practitioners and a HF clinic.
In the telemonitoring group vs. the usual care group, all-cause mortality was significantly lower (5% vs. 17.5%; p=0.01); follow-up days lost to hospitalization, dialysis or death were significantly lower (13 vs. 30 days; p=0.02); and the number of HF hospitalizations was lower (0.24 vs. 0.42 hospitalizations/patient, p=0.06).
In recent years, more outcomes trials continue to add support to the value of remote monitoring for chronic disease as a means to provide better care and reduce health care costs.
5. Who will pay for all these wearable devices?
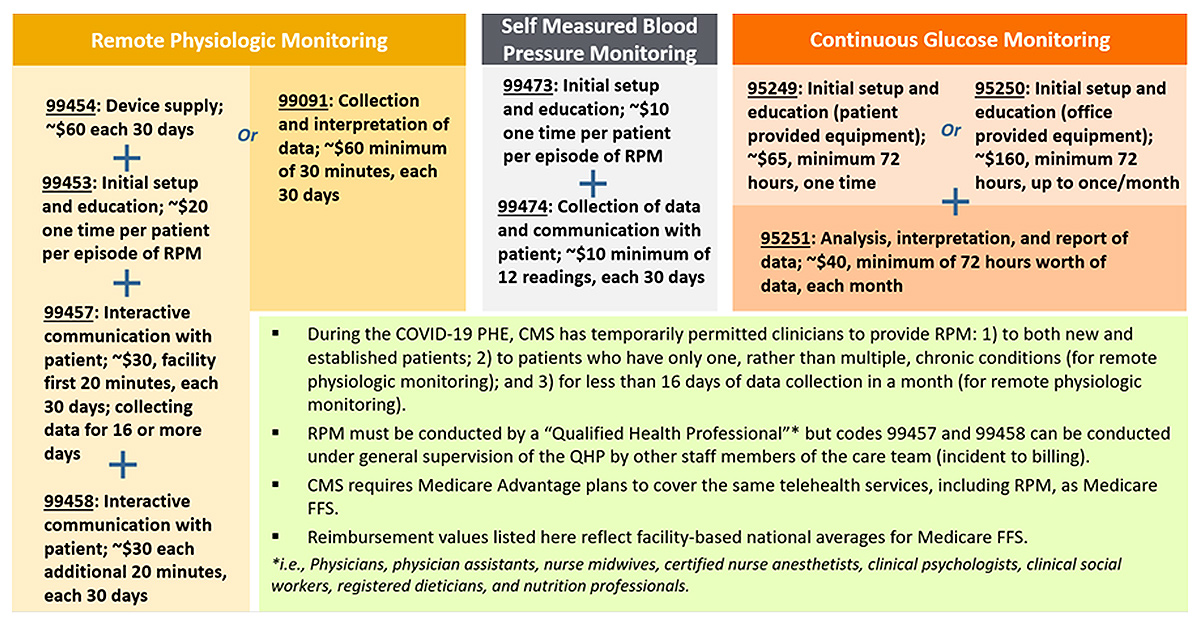 Used with permission from Manatt, and available here. Click the image above for a larger view.
Used with permission from Manatt, and available here. Click the image above for a larger view.
The inevitable question is, of course, who is going to pay for it. Medicare and commercial payers have committed to RPM payments through CPT codes established since January 2019.
In 2020, CMS doubled down, saying the agency will pay for several new CPT codes that not only reimburse providers for various types of care they may already be providing, but would open new potential revenue streams to help ease the transition into value-based care.
Code 99453 covers the set-up of devices in an episode of care and patient education, while code 99454 covers the cost of device(s) with daily recording(s) or programmed alert(s) and can be billed every 30 days. These CPT codes offer reimbursement for providing the patient with a device as defined by the FDA.
While CMS may further define the device definition in 2021, it currently remains very broad. Code 99457 covers the first 20 minutes each calendar month of RPM treatment management services of clinical staff/physician/other qualified health care professional time requiring interactive communication with the patient/caregiver during the month.
CMS began paying for CPT code 99458 on Jan. 1, 2020. The new code covers each additional 20 minutes (each calendar month) spent on treatment management services. Also beginning Jan. 1, 2020, CPT codes 99457 and 99458 were designated as care management services by CMS, which means they can be furnished under general rather than direct supervision of the billing provider.
The net effect is that the physician or other qualified health care professional supervising the delivery of RPM services doesn't have to be located at the same site as the clinical staff delivering them.
Conclusion
Now, more than ever, the barriers to adoption of remote monitoring and digital health have been mostly overcome for cardiologists. There are now solutions for the concerns about increased amounts of data leading to increased workload and lack of workflow integration crippling cardiology practice efficiencies.
Establishment of viable payment options through CMS and other payers for RPM, mitigation of patient concerns over health information privacy using secure portals, greater patient and physician understanding of supporting research proving quality of care through data and science all support increased use of remote monitoring devices.
The future of cardiology and cardiovascular care will no doubt integrate wearable devices, remote monitoring, machine learning, artificial intelligence and algorithms to risk stratify patients as the health care system moves from fee-for-service to a more value-based approach. And 2021 is only the beginning of the digital revolution for cardiology.
Reading List
Rock Health, LLC. Digital Health Funding Database. Available here. Accessed Aug. 28, 2018.
Cohen AB, Dorsey ER, Mathews SC, et al. A digital health industry cohort across the health continuum. NPJ Digit Med 2020;3(1).
Jiang X, Ming WK, You JH. The cost-effectiveness of digital health interventions on the management of cardiovascular diseases: systematic review. J Med Internet Res 2019;21:e13166.
Chatterjee NA, Singh JP. Making sense of remote monitoring studies in heart failure. Eur Heart J 2017;38:2361-3.
Ajami S, Teimouri F. Features and application of wearable biosensors in medical care. J Res Med Sci 2015;20:1208.
Walsh JA, Topol EJ, Steinhubl SR. Novel wireless devices for cardiac monitoring. Circulation 2014;130:573-81.
Carpenter A, Frontera A. Smart-watches: a potential challenger to the implantable loop recorder? Europace 2016;18:791-3.
Widmer RJ, Collins NM, Collins CS, et al. Digital health interventions for the prevention of cardiovascular disease: a systematic review and meta-analysis. Mayo Clin Proc 2015;90:469-80.
Mobile Smith. How to reduce preventable readmissions with healthcare IT. Available here. Published Jan. 30, 2015. Accessed Feb. 12, 2021.
Kekade S, Hseieh CH, Islam MM, et al. The usefulness and actual use of wearable devices among the elderly population. Comput Methods Programs Biomed 2018;153:137-59.
Vegesna A, Tran M, Angelaccio M, Arcona S. Remote patient monitoring via non-invasive digital technologies: a systematic review. Telemed J E Health 2017;23:3-17.
Dendale P, De Keulenaer G, Troisfontaines P, et al. Effect of a telemonitoring-facilitated collaboration between general practitioner and heart failure clinic on mortality and rehospitalization rates in severe heart failure: the TEMA-HF 1 (TElemonitoring in the MAnagement of Heart Failure) study. Eur J Heart Fail 2012;14:333-40.
Reginal A, Stowe EC, Augenstein J. A quick reference guide to remote patient monitoring during the COVID-19 pandemic. Manatt. Available here. Published July 7, 2020. Accessed Feb. 12, 2021.
Clinical Topics: Arrhythmias and Clinical EP, COVID-19 Hub, Heart Failure and Cardiomyopathies, Atherosclerotic Disease (CAD/PAD), Atrial Fibrillation/Supraventricular Arrhythmias, Acute Heart Failure
Keywords: ACC Publications, Cardiology Magazine, Atrial Fibrillation, Centers for Medicare and Medicaid Services, U.S., Wireless Technology, Coronary Artery Disease, Artificial Intelligence, Mobile Applications, Electronic Health Records, Blood Pressure, COVID-19, United States Food and Drug Administration, Medicare, Telemedicine, Monitoring, Physiologic, Electrocardiography, Heart Failure, Delivery of Health Care, Risk Assessment
< Back to Listings