Focus on EP | ACC.23/WCC: Five Practice Takeaways For Electrophysiologists

The scientific program at ACC.23/WCC was packed from the late-breaking clinical trials (three related to electrophysiology [EP]) and featured clinical research to the Learning Pathways, including EP, providing the opportunity to expand our general and specialty specific knowledge. As always, though, it's not possible to attend every presentation or attend every day.
Fortunately, using ACC Anywhere, I was able to retrieve and review all the relevant EP content and more from the meeting. I highly recommend everyone access use this online video library. Here are five I learned that can affect EP practice.

Pulse field ablation is the future for PVI in AFib ablation.
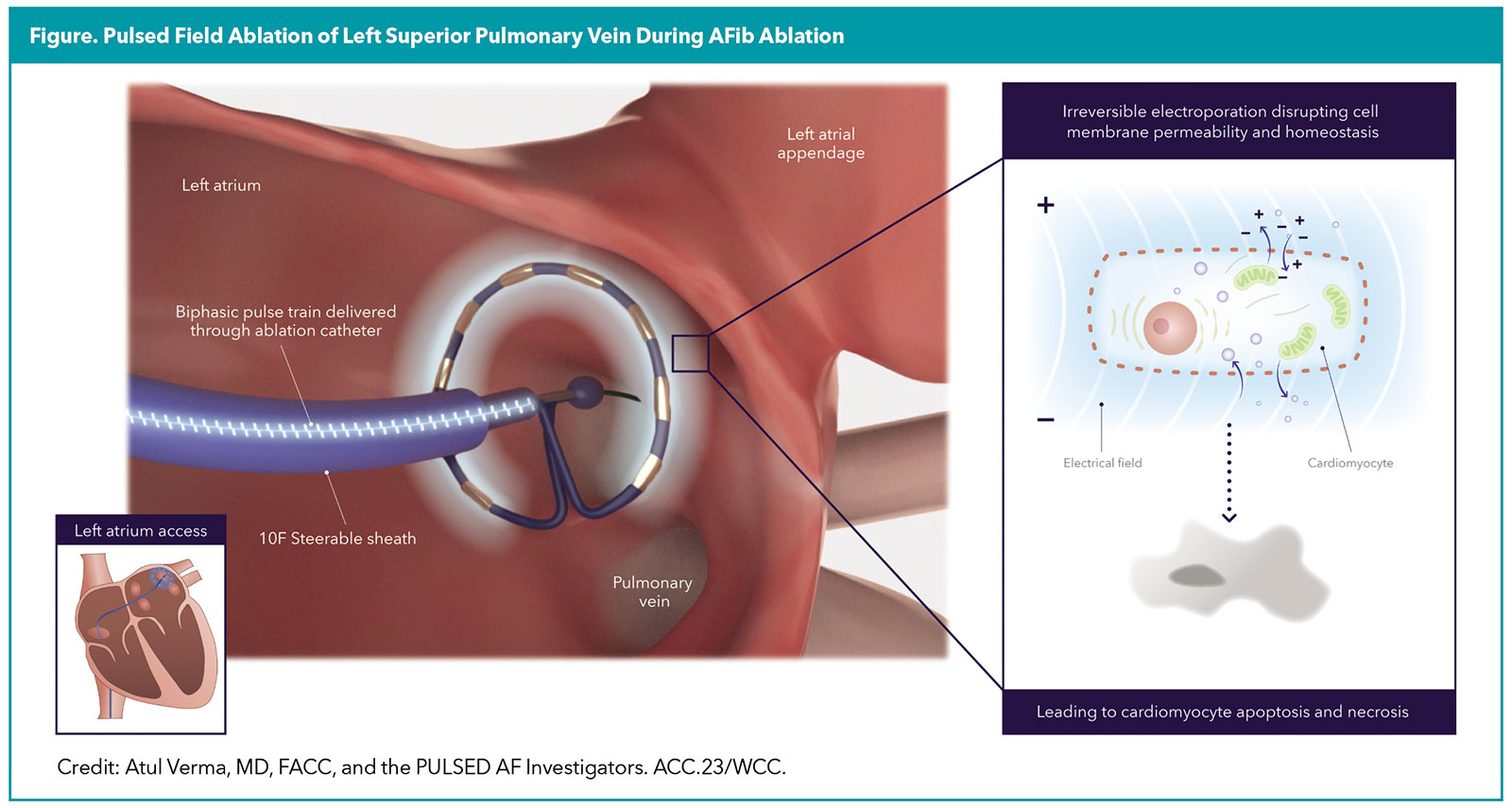
Undoubtedly the most exciting EP update was the long-awaited, late-breaking clinical trial presentation for the PULSED AF Pivotal trial.1 This is the first clinical trial to report outcomes related to the use of the Medtronic PulseSelect pulsed field ablation (PFA) system for pulmonary vein isolation (PVI) in patients with symptomatic, drug-refractory atrial fibrillation (AFib). Of note, this was a multicenter but nonrandomized single-arm study.
One-hundred and fifty patients with paroxysmal AFib and 150 patients with persistent AFib underwent PFA (Figure). At one year, the primary composite effectiveness endpoint of freedom from acute procedural failure, arrhythmia recurrence or antiarrhythmic escalation (excluding a three-month blanking period) was 66.2% in the paroxysmal group (95% CI, 57.9-73.2%) and 55.1% in the persistent group (95% CI, 46.7-62.7%).
The primary composite safety endpoint of serious procedure- and device-related adverse events occurred in one patient in the paroxysmal group who developed a stroke and one patient in the persistent group who developed cardiac tamponade (0.7%; 95% CI, 0.1-4.6).
While these safety and efficacy outcomes of PFA were consistent with modern day radiofrequency and cryoablation outcomes, the procedural workflow was substantially faster. The mean time between the first and last PFA application was approximately one hour (58 ± 28 minutes vs. 64 ± 28 minutes in the paroxysmal and persistent groups, respectively).
However, the time measurement included a mandatory 20-minute waiting period and postablation mapping time. The actual time spent delivering PFA energy was <30 seconds per patient in each group (25 ± 8 seconds vs. 29 ± 10 seconds, respectively). General anesthesia was used in 89% and 84% of patients in the respective groups, but the expected real-world use of PFA is likely to require no more than deep sedation.

In AFib, maintaining sinus rhythm has additional benefits.
After the EAST-AFNET4 trial demonstrated the superiority of rhythm control over usual care (rate control) in AFib for reducing cardiovascular death and stroke, subsequent studies have suggested additional cognitive and cardiac function protection with maintaining sinus rhythm.
Cognitive Function
A 2022 report from the AF-SCREEN international collaboration on AFib and dementia surmised that inflammation and hypoperfusion from AFib may result in cognitive impairment independent of thromboembolic stroke.2
A 10-year evaluation of 194,928 patients with AFib treated with ablation or medical therapy revealed that patients who underwent AFib ablation had a significantly lower risk of developing dementia, even after correcting for stroke events (4.7 vs. 5.9 cases per 1000 person-years; hazard ratio [HR], 0.76; p=0.015).3
Not surprisingly, the subset of patients who experienced a successful AFib ablation (defined as freedom from subsequent cardioversion, antiarrhythmic medication use or repeat ablation) had a significantly decreased risk of dementia compared with those who had a failed AFib ablation (HR, 0.56; 95% CI, 0.44-0.71; p<0.05).
This hypothesis was further supported by a more recent study that compared brain MRIs in 57 patients with AFib who underwent AFib ablation and 11 patients with AFib who underwent medical management only.4 Freedom from atrial tachyarrhythmias was achieved in 84.2% of patients who underwent AFib ablation. Repeat brain MRI at six months demonstrated significantly increased cerebral blood flow in patients who underwent AFib ablation vs. medical management (39.26 vs. –34.86 mL; p=0.01).
Cardiac Function
An echocardiographic study of cardiac remodeling and functional regurgitation at the one-year follow-up of 47 AFib patients with active restoration of sinus rhythm (cardioversion and/or ablation), 31 AFib patients with spontaneous restoration of sinus rhythm and 39 AFib patients who remained in AFib revealed that active restoration was associated with a significant improvement in cardiac chamber size (indexed volume), cardiac chamber function (ejection fraction), and severity of tricuspid and mitral valve regurgitation (vena contracta diameter).5
Interestingly, spontaneous restoration of sinus rhythm was also associated with improvements in valvular regurgitation severity but not in cardiac chamber size and function.

Left atrial appendage closure is associated with additional benefits too.
In 2015, percutaneous left atrial appendage closure (LAAC) was approved as an alternative to long-term oral anticoagulation (OAC) therapy in patients with AFib. Recent studies indicate there may be additional benefits related to a reduction in stroke severity along with improvements in cognitive decline.
Stroke Severity
A large multicenter investigation (publication pending) led by Vivek Reddy, MD, compared ischemic stroke severity in 98 patients who had undergone prior LAAC and in 89 patients who were on novel OACs. Disabling or fatal strokes (modified Rankin score ≥3) were significantly lower in the LAAC group compared with the OAC group, both at the time of hospital discharge (33% vs. 60%; p<0.001) and at the three-month follow-up (27% vs. 51%; p=0.001). Potential explanations for this observation include smaller emboli in patients with LAAC and superimposed bleeding in patients taking OACs.
Cognitive Function
Cognitive function was assessed with the Montreal Cognitive Assessment (MoCA) in 50 patients who had undergone AFib ablation and LAAC (not on OAC) and in 48 patients who had undergone AFib ablation only (remained on OAC).6 Compared with baseline measurements, at the one-year follow-up, patients in the OAC group experienced a significant decline in cognitive function (mean –2.74 points on MoCA; 95% CI, –3.61 to –1.87; p<0.0001) whereas there was no significant change in the LAAC group (mean +0.79 points on MoCA; 95% CI, –0.06 to 1.64; p=0.07).

Conduction system pacing outperforms traditional CRT.
His-bundle pacing was approved as an alternative to traditional right ventricular apical pacing in 2018 by the U.S. Food and Drug Administration. In October 2022, this approval was expanded to include pacing from the left bundle branch (LBB) area.
A recent meta-analysis of patients with heart failure and LBB block compared 159 patients who underwent LBB area pacing with 230 patients who underwent conventional biventricular pacing for CRT.7 LBB area pacing was successful in 88.3% of cases.
Compared with CRT, those who underwent LBB area pacing experienced a significantly narrower QRS (mean difference –22.65 ms; p<0.00001), improved left ventricular ejection fraction (mean difference +6.73; p<0.0001), and improved NYHA classification (mean difference –0.47; p=0.0003). The investigators concluded that LBB area pacing was superior to CRT both in terms of electro-mechanical function and clinical outcomes.

Remote monitoring of CIEDs is eco-friendly and cost-effective.
I routinely recommend my patients with cardiac implantable electronic devices (CIEDs) to enroll in remote monitoring (RM) to reduce unnecessary patient visits and alleviate congestion in the clinic. Now there is additional data promoting the benefits of RM on a population level.
An observational study evaluated the environmental and economic impact of RM in 32,811 patients with CIEDs from 67 device clinics across 30 cities in the U.S.8 Remote interrogations occurred every month for patients with loop recorders and every three months for those with permanent pacemakers and implantable defibrillators.
Over a two-year period (July 2020 to June 2022), RM prevented 31.7 million miles of car travel, corresponding to a 12,518 metric ton reduction in carbon dioxide production from gasoline burned; and prevented printing of 14.2 million pieces of paper, corresponding to a 78 metric ton reduction in carbon dioxide production from paper making.
Economically, remote monitoring alleviated the need to purchase gasoline for car travel, calculated as a cost savings of $3.45 million dollars; the need to have as many cardiac device technicians available for in-person CIED interrogations, calculated as a cost savings of $3.7 million; and the need to print paper interrogation reports, calculated as a cost savings of $3 million. In total, RM of 32,811 patients over a two-year period led to a net reduction in 12,596 tons of greenhouse gas emissions and net savings of $10.15 million.

This article was authored by Edward Chu, MD, (@Ed_Chu_MD), an electrophysiology attending physician in Miami, FL.
References
- Verma A, Haines DE, Boersma LV; PULSED AF Investigators. Pulsed field ablation for the treatment of atrial fibrillation: PULSED AF pivotal trial. Circulation 2023;Mar 6:Epub ahead of print.
- Rivard L, Friberg L, Conen D, et al. Atrial fibrillation and dementia: A Report from the AF-SCREEN International Collaboration. Circulation 2022;145:392-409.
- Kim D, Yang PS, Sung JH, et al. Less dementia after catheter ablation for atrial fibrillation: A nationwide cohort study. Eur Heart J 2020;41:4483-93.
- Takahashi Y, Yamamoto T, Oyama J, et al. Increase in cerebral blood flow after catheter ablation of atrial fibrillation. JACC Clin Electrophysiol 2022;8:1369-77.
- Soulat-Dufour L, Lang S, Addetia K, et al. Restoring sinus rhythm reverses cardiac remodeling and reduces valvular regurgitation in patients with atrial fibrillation. J Am Coll Cardiol 2022;79:951-61.
- Mohanty S, Mohanty P, Trivedi C, et al. Impact of oral anticoagulation therapy versus left atrial appendage occlusion on cognitive function and quality of life in patients with atrial fibrillation. J Am Heart Assoc 2021;10:e019664.
- Aamir M, Yasmin F, Moeed A, et al. Left bundle branch biventricular pacing in hear failure patients with left bundle branch block: An updated systematic review and meta-analysis. J Am Coll Cardiol 2023;March 8(8_Supplement 59). Available here.
- Bawa D, Ahmed A, Darden D, et al. Impact of remote cardiac monitoring on green house gas emissions. JACC Adv 2023;Mrch 3. Available here.
Clinical Topics: Anticoagulation Management, Arrhythmias and Clinical EP, Cardiac Surgery, Heart Failure and Cardiomyopathies, Noninvasive Imaging, Anticoagulation Management and Atrial Fibrillation, Implantable Devices, EP Basic Science, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Cardiac Surgery and Arrhythmias, Cardiac Surgery and Heart Failure, Acute Heart Failure, Echocardiography/Ultrasound, Magnetic Resonance Imaging, Sleep Apnea
Keywords: ACC Publications, Cardiology Magazine, ACC Annual Scientific Session, ACC23, Atrial Fibrillation, Electric Countershock, Cryosurgery, Follow-Up Studies, Stroke Volume, Mitral Valve, Tachycardia, Anti-Arrhythmia Agents, Magnetic Resonance Imaging, Inflammation, Stroke, Echocardiography, Electrophysiology, Dementia, Heart Failure, Pacemaker, Artificial, Anticoagulants, Ischemic Stroke, Ventricular Function, Left, Defibrillators, Implantable
< Back to Listings