Business of Medicine | It's Time to Think Differently About Access: Success Requires More than Operational Change

Year after year, access is one of the top concerns from cardiovascular programs and practices across the country. How do we get new patients in the door when we don't have enough appointment slots? How do we expand capacity when we can't recruit enough cardiologists? Where are we supposed to put all the follow-ups?
True, access is a complex problem. Its scope is broad and there are numerous factors at play: clinically complicated patients, provider capacity, multifaceted scheduling protocols, lack of clinical standardization, Relative Value Unit targets, lean staffing and antiquated phone systems, to name a few.
Many organizations have tried for years to improve access incrementally, by modifying scheduling templates and protocols and bringing advanced practice providers (APPs) on board. When third-party payers offered reimbursement, some programs dipped their toe into the water of telehealth visits.
Then came the COVID-19 crisis. Within two weeks, scheduling protocols completely shifted. Nonemergent visits and procedures were canceled. Patients were given telehealth visit options.
By late March 2020, results of MedAxiom's Impact of COVID-19 on Cardiovascular Organizations Survey showed that more than half of the groups (52.3%) were performing less than a quarter of their patient visits face-to-face. In other words, 75% of encounters were by some form of remote or telehealth means.1
The pandemic proved that cardiovascular programs and practices can make enormous shifts in their access protocols, at lightning speed. It was amazing to watch MedAxiom members pivot so quickly. They admirably focused on what was right for patients and health care providers first, and on the financial implications of those actions second. They did this because it was the right thing to do.
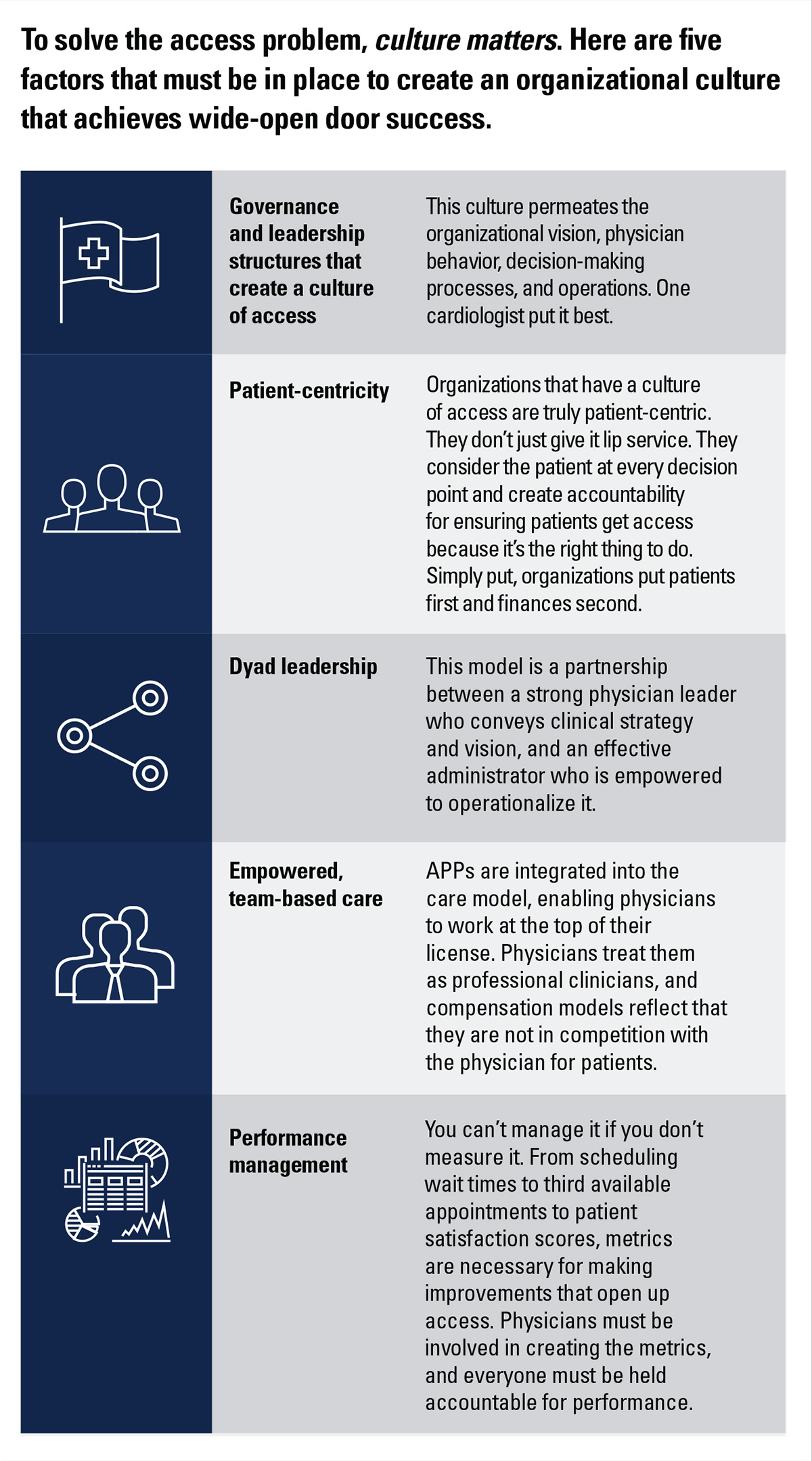
These same principles apply to creating wide-open door access for patients. The foundation for truly solving the access problem is to create governance and leadership structures that support a culture of access.
One that permeates the organization and creates an environment in which everyone recognizes that access is a priority that's integrated into standard operations and care protocols.
Not back door access, with physician-only phone lines or giving out personal cell phone numbers, but open access through normal channels, that is sanctioned by physicians and believed and upheld by all staff.
As Peter Drucker famously said: Culture eats strategy. If your organization tolerates individual provider scheduling preferences, hasn't updated care protocols for follow-ups and ongoing patient management, or has no clear plan for the role and development of APPs, you have a culture and leadership opportunity, not an access problem. Despite how well planned or managed they are, well-intentioned operational or structural improvement efforts won't be enough.
Note: This is an excerpt from a new MedAxiom White Paper on building a culture of access. The full white paper is available at MedAxiom.com/Publications.
References
- Survey: Impact of COVID-19 on CV Organizations, April 3, 2020, MedAxiom, an ACC Company.
Clinical Topics: COVID-19 Hub
Keywords: ACC Publications, Cardiology Magazine, COVID-19, Pandemics, Insurance, Health, Reimbursement, Leadership, Access to Information, severe acute respiratory syndrome coronavirus 2, Telemedicine, Names, Appointments and Schedules, Telephone
< Back to Listings