Feature | Returning to Play After Coronavirus Infection: A Perspective From Pediatric Cardiologists

Typically, during the summer months, pediatricians and family physicians are inundated with requests for sports clearance physicals. This year, as schools and sports reopen, a new question will need to be addressed at these appointments: is it safe for my child to resume physical activity and sports after a COVID-19 infection?
There have been eloquent editorials written on the return-to-play topic from an adult cardiologist's perspective,1-3 but no statements or articles addressing return-to-play from the perspective of pediatric cardiologists.
For four reasons, we believe it would be wrong to universally apply the "adult return-to-play" criteria to the pediatric population.
One, fortunately, COVID-19 infections in pediatric patients are more likely to be asymptomatic or mild compared with adult patients.4,5
This means pediatric providers will frequently be presented with the return-to-play question for patients who had asymptomatic or very mild disease.

Two, there is a significant amount of variation in intensity of youth and school-based sports. Providers should not treat the 7-year-old recreational soccer player the same as the 18-year-old varsity basketball player.
Three, the pediatric population is less reliant on electrocardiograms (ECGs), echocardiograms, stress testing and troponins for general screening and for clearing patients for exercise and sports.
Four, in the pediatric population, it may be inappropriate to follow the recommendation to consider using the COVID-19-positive pathway algorithm for a patient who develops symptoms concerning for COVID-19 and testing is negative or not obtained.1
Respiratory infections in the pediatric population are highly prevalent and in the presence of reliable negative COVID-19 testing should not result in a presumptive diagnosis in the pediatric population.
The question of returning to sports is significant because of the propensity for COVID-19 to cause cardiac damage and myocarditis.6
While the incidence of myocarditis is lower in the pediatric population compared with the adult population, myocarditis is known to be a cause of sudden death during exercise in the young athletic populations.
Similar to other forms of myocarditis, providers caring for patients who have had a COVID-19 infection should be confident there is no myocardial injury prior to clearing athletes to participate.7
When considering the question of return-to-play, we believe there are three variables:
- How recent was the COVID-19 infection?
- How severe was the infection?
- What is the physical activity or sport being considered?
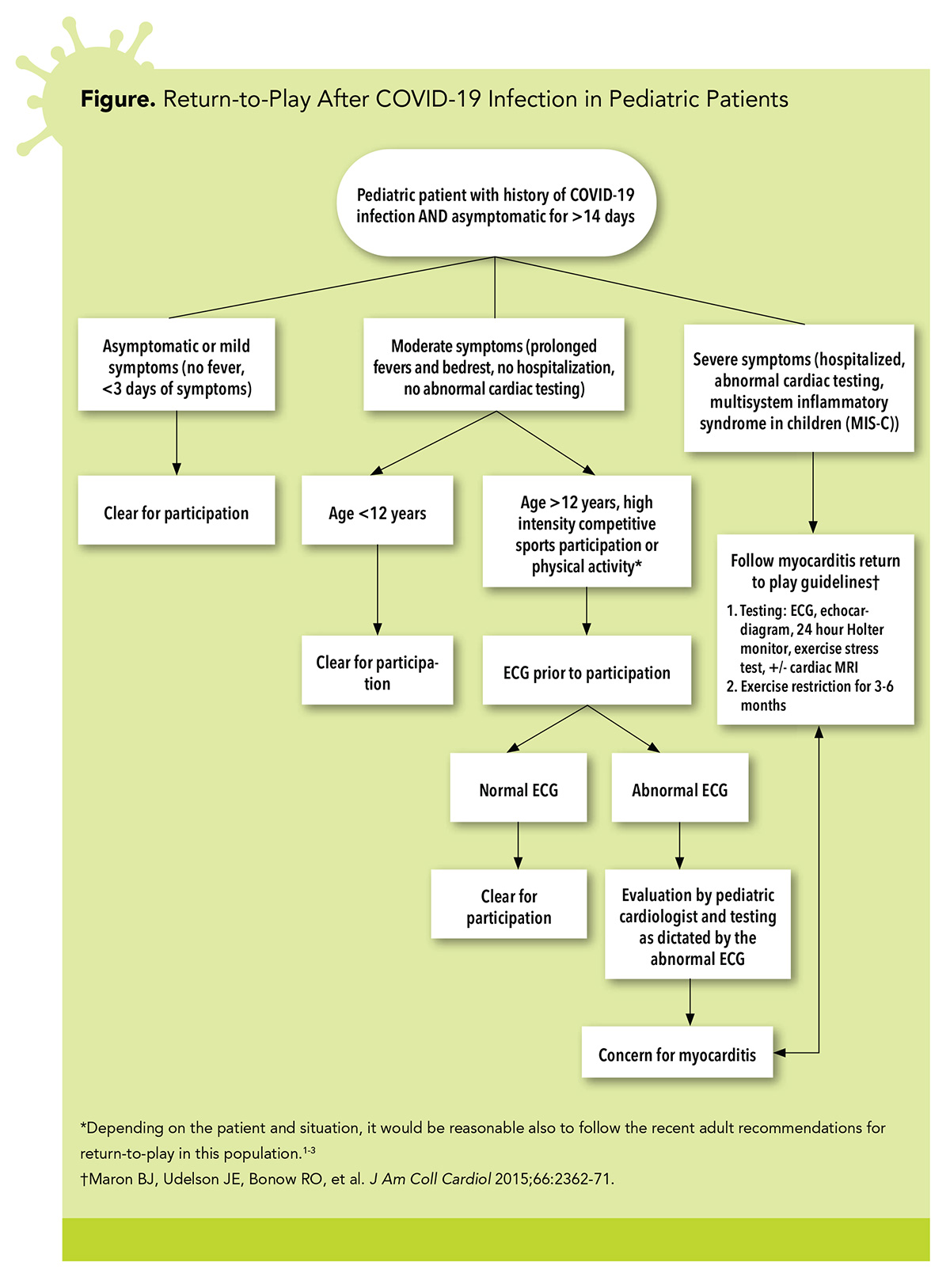
Assuming there were no clinical or laboratory findings suggesting myocardial involvement during the acute infection, before considering return-to-play patients should be asymptomatic for at least two weeks (Figure).
This two-week period will allow for the full clinical manifestations of COVID-19 to present themselves and, perhaps most importantly, decrease the risk of transmitting the infection to teammates or opponents.
Regarding the severity of the illness, we believe that asymptomatic or mild illnesses in the pediatric population should be treated similarly to other viral illnesses in the pediatric population.
This typically means that children refrain from physical activity and sports while actively sick or febrile and gradually return to activities as they feel able. These patients likely did not require cardiac testing during their acute infection, so we do not believe cardiac testing is needed to clear them for participation.
While most pediatric patients will be asymptomatic, there certainly are severe presentations. Severe disease would be defined as somebody who required hospitalization, had abnormal cardiac testing during the acute infection, and/or had the recently described multisystem inflammatory syndrome in children (MIS-C).

The impact on the heart in MIS-C seems similar to the presentation of other acute viral myocarditis in pediatric patients,8 therefore it would be reasonable to treat pediatric patients who have had MIS-C as if they had myocarditis. These patients likely will have had cardiac testing during the acute phase (echocardiograms, ECGs, etc.).
Depending on the results of these tests, based on care of athletes with myocarditis, the patient should be restricted for three to six months and only resume activities when/if cardiac testing (ECG, echocardiogram, 24-hour Holter monitor, exercise stress test and possibly cardiac MRI) have normalized.7
We must emphasize that nothing is known about the long-term history of pediatric patients with MIS-C.
Although complete or near complete recovery of cardiac function is often seen in this population, even prior to hospital discharge, more frequent and longer monitoring of this population may be warranted.
In the absence of any data, a conservative approach for return-to-activity is probably indicated for this small subpopulation of COVID-19 patients.
For patients whose infection caused symptoms between mild and severe COVID-19 disease, there will be a variety of considerations. These patients with "moderate" symptoms may have had prolonged fevers and symptoms and could have had subclinical myocardial injury even if they did not have cardiac symptoms or have cardiac testing during the acute phase.

Since ECGs are typically abnormal in myocarditis,9 it would be reasonable to perform an ECG on an older pediatric patient who wants to return to high school or collegiate sports.
Depending on the patient and situation, it also would be reasonable to follow the recent adult recommendations for return-to-play in this population, which would include a high-sensitivity troponin and echocardiogram.1,2
For the younger patients (<12-year-olds), because their exertional level during sports is likely not significantly higher than their activities of daily living, we do not believe cardiac testing is required to clear them for physical activity or sports if their history and exam are reassuring.
We should also remember that even with extensive cardiac testing, we will never be able to completely rule out all cases of myocyte damage or predict with absolute certainty which patients with acute infections are at risk for cardiac involvement.
Therefore, we will never be able to guarantee every child is safe. For this reason, we encourage youth sports and high school sports to reevaluate their emergency action plans to ensure appropriate CPR, defibrillation and emergency medical care are provided if a sudden cardiac arrest occurs.
References
- Phelan D, Kim JH, Chung EH. A game plan for the resumption of sport and exercise after Coronavirus Disease 2019 (COVID-19) infection. JAMA Cardiol 2020;May 13:[Epub ahead of print].
- Baggish A, Drezner JA, Kim J, et al. Resurgence of sport in the wake of COVID-19: cardiac considerations in competitive athletes. Br J Sports Med 2020;Jun 13:[Epub ahead of print].
- Dores H, Cardim N. Return to play after COVID-19: a sport cardiologist's view. Br J Sports Med 2020;May 7:[Epub ahead of print].
- Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 2020;323:1775-6.
- Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA 2020;323:2052-9.
- Driggin E, Madhavan MV, Bikdeli B, et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol 2020;May 12:[Epub ahead of print].
- Maron BJ, Udelson JE, Bonow RO, et al. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: task force 3: hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy and other cardiomyopathies, and myocarditis. J Am Coll Cardiol 2015;66:2362-71.
- Belhadjer Z, Méot M, Bajolle F, et al. Acute heart failure in multisystem inflammatory syndrome in children (MIS-C) in the context of global SARS-CoV-2 pandemic. Circulation 2020;May 17:[Epub ahead of print].
- Canter CE, Simpson KP. Diagnosis and treatment of myocarditis in children in the current era. Circulation 2014;129:115-28.
Clinical Topics: Arrhythmias and Clinical EP, COVID-19 Hub, Diabetes and Cardiometabolic Disease, Heart Failure and Cardiomyopathies, Prevention, Sports and Exercise Cardiology, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Exercise, Sports and Exercise and ECG and Stress Testing
Keywords: ACC Publications, Cardiology Magazine, COVID-19, Myocarditis, Troponin, Incidence, Physicians, Family, severe acute respiratory syndrome coronavirus 2, Exercise Test, Electrocardiography, Athletes, Patient Discharge, Activities of Daily Living, Electrocardiography, Ambulatory, Death, Sudden, Cardiac, Sports, Exercise
< Back to Listings