Innovation at ACC | Virtual Strides in Blood Pressure Control
In a year that has stunted growth in many arenas, the health technology space has experienced the opposite effect. Recently, at least 68 companies are in the remote monitoring space.1 Further, there are at least 128,000 health coaches and health educators, promising dramatic results and changed lives.2 This number is likely underreported. In 2017, the U.S. Health Coaching market was worth $6.14 billion, up 15% from 2014, expected to grow to $7.85 billion by 2022.3
Despite a ballooning health technology industry, improved outcomes remain undelivered. Cardiovascular disease is still the #1 killer worldwide, amplified during a pandemic that discouraged patients from seeking care for both chronic and high acuity problems, even acute myocardial infarction.4
The elephant in the room is clear: how do we bridge the bells and whistles of technology with usable, practical and meaningful change?
It comes down to a simple hypothesis: pair quality clinical care with reliable data and engaged patients to see results. There is to date no substitute for the master clinician, able to reliably diagnose and effectively treat patients to reach targets outlined in clinical guidelines and drive down cardiovascular events. Thus, for health technology to achieve the promise of reducing adverse health events, we must arm clinicians with the right tools, connect them with patients and keep both sides engaged.
Over the past 12 months, Heartbeat Health has directly managed 10,459 patients with a model of virtual cardiovascular care that utilizes telemedicine, remote patient monitoring and clinical disease management that includes patient engagement. Many patient phenotypes have benefited from this model of care. Here we describe the use case of a group of patients with hypertension at moderate risk of cardiovascular disease.
Engaging Patients, Reaching Targets
We retrospectively evaluated data from a subset of 96 ambulatory patients who had scheduled a virtual consultation with a cardiovascular professional (MD or physician assistant) on the Heartbeat Health software platform.
After this enrollment into virtual cardiovascular care, patients with hypertension were invited to enroll in Heartbeat Measure, a manual-entry remote monitoring component of the Heartbeat Health app or to use Bluetooth-connected blood pressure (BP) devices. Follow-up consultation was based on patients' clinical status and need for medication adjustment.

A retrospective chart review at six months included an evaluation of the number of virtual visits, medication adjustments, and BP level at enrollment and six months. Some patients had completed care with Heartbeat Health by the time this analysis was finished.
The average age of the patients was 52 years, ranging from 26 to 93 years. Most had hypertension (98%), and 19% had type 2 diabetes, 15% coronary artery disease, 22% heart failure, 10% chronic kidney disease and 34% had hyperlipidemia.
The use of Heartbeat Measure was high, with 90% of those invited to use this component of the app logging their BP measurements at least once weekly. The average number of virtual visits was 5.1, with an average of 1.6 medication changes.
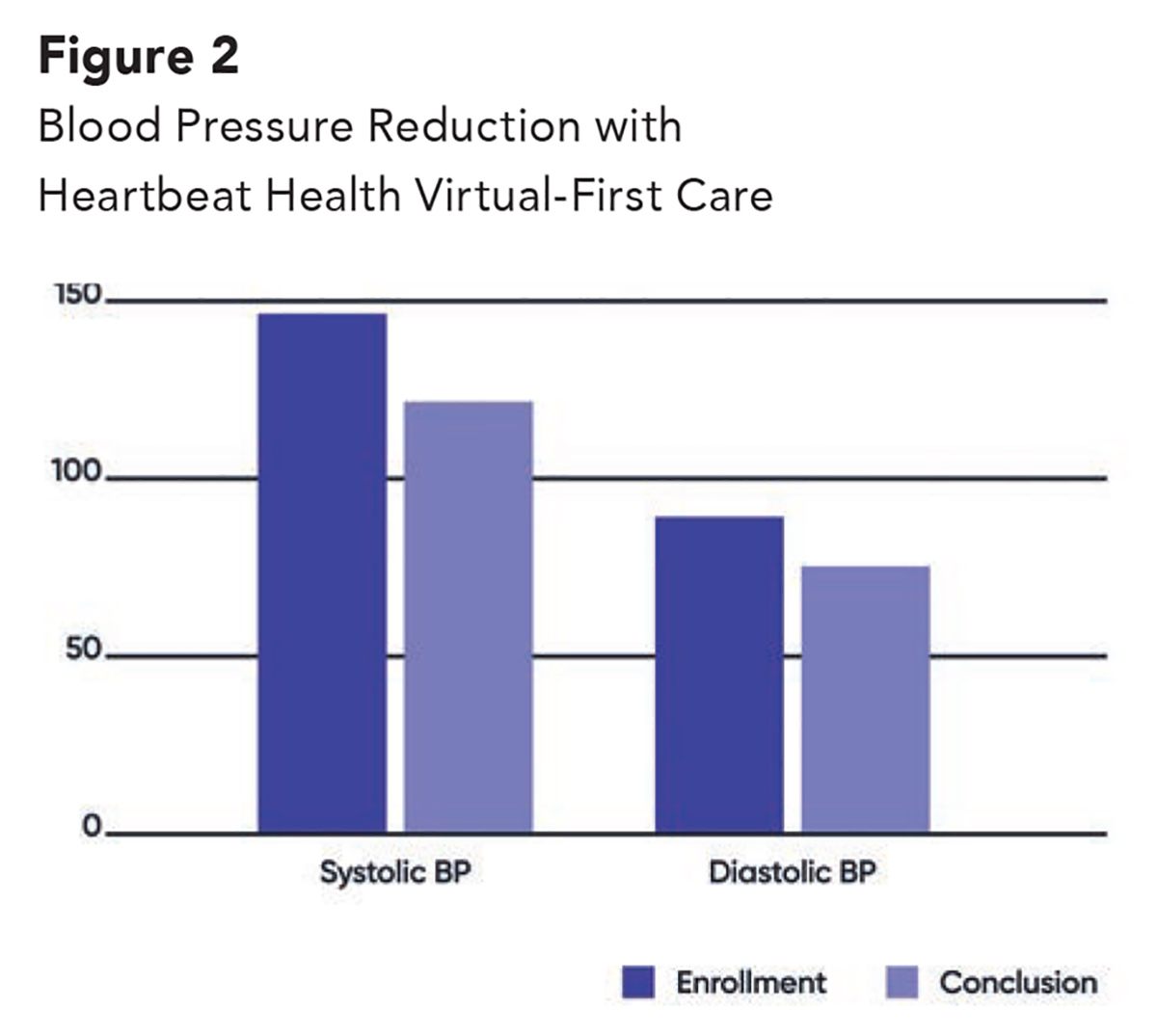
At enrollment, the average BP was 146/89 mm Hg, consistent with stage 2 hypertension, according to the ACC/AHA guideline.5
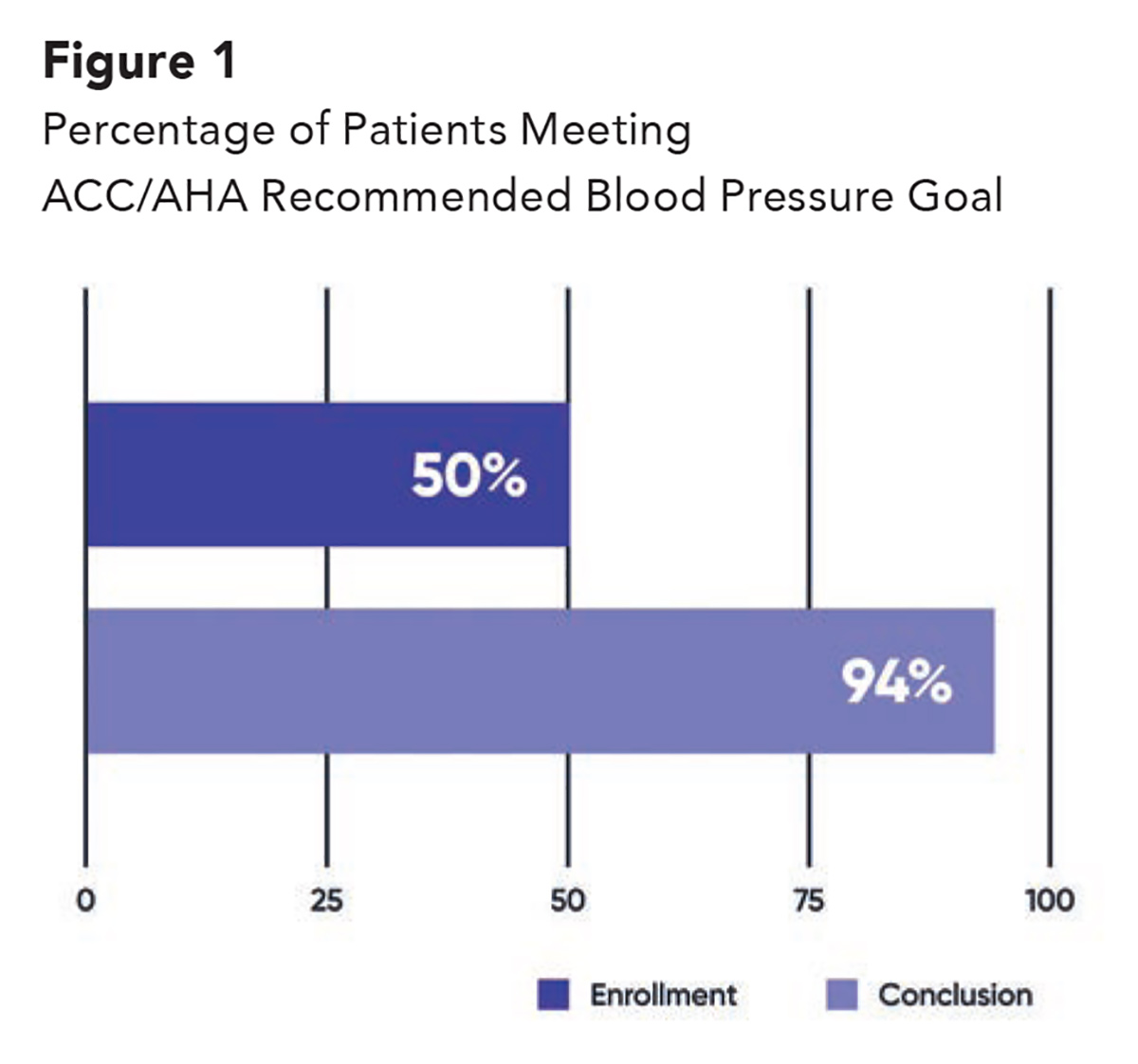
Only 50% of participants met the recommended BP target at enrollment, and this was increased to 94% at six months, with an average BP of 122/75 mm Hg (Figure 1). The average reductions in systolic and diastolic BP were 24.1 mm Hg and 12.5 mm Hg, respectively (Figure 2).
Small Changes, Big Differences
Our cohort analysis illustrates that a program combining frequent virtual visits and BP self-monitoring that maintains patient engagement may lead to rapid improvements in reaching BP goals.
Furthermore, the level of BP reduction we achieved has been shown to directly improve outcomes. Every 10 mm Hg drop in systolic BP translates to a significant reduction in major cardiovascular disease events (relative risk, 0.80; 95% confidence interval, 0.77-0.83).6,7 In one-year follow-up alone, this translates to a 20% reduction in coronary heart disease events and 32% reduction in stroke.8
Although the small sample size and lack of randomization are among limitations of our analysis, data such as these hold the promise that a simple formula – strong clinical care with effective virtual touchpoints – may be the recipe for success.
Innovative Partners
The Heartbeat Health virtual cardiovascular care platform offers a set of tools that combine telemedicine, remote monitoring and disease-specific patient engagement that have demonstrated successful patient activation, engagement, program adherence and clinical outcomes.
Learn more about Heartbeat Health and opportunities for ACC members at ACC.org/HeartbeatHealth.
Learn more about ACC's Innovation Program at ACC.org/InnovationProgram.


This article was authored by Jana M. Goldberg, MD, FACC, a cardiologist and medical director, HeartBeat Health, and Jeffrey D. Wessler, MD, MPhil, FACC, a cardiologist and founder/CEO, Heartbeat Health.
References
- Remote Patient Monitoring Companies. Healthcare IT Today. Available here. Accessed May 3, 2021.
- United States Health Coaching Market Report 2021-2025 with Discussion of Effects of the COVID-19 Pandemic on Operations/Growth. Available here. Accessed May 3, 2021.
- U.S. Health Coaching Market Growing Among Consumers, Insurers and Employers. Available here. Accessed May 3, 2021.
- Wadhera R, Shen C, Gondi S, et al. Cardiovascular deaths during the COVID-19 pandemic in the United States. J Am Coll Cardiol 2021;77:159-69.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ ABC/ACPM/AGS/APhA /ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2018;71:e127-e248.
- D'Anci KE, Tipton K, Hedden-Gross A, et al. Effect of intensive blood pressure lowering on cardiovascular outcomes: A systematic review prepared for the 2020 US Department of Veterans Affairs/US Department of Defense Guidelines. Ann Intern Med 2020;173:895-903.
- Wang TJ, Vasan RS. Epidemiology of uncontrolled hypertension in the United States. Circulation 2005;112:1651-62.
- Law MR, Wald NR. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 2009;338:b1665.
- Bryant KB, Sheppard JP, Ruiz-Negron N, et al. Impact of self‐monitoring of blood pressure on processes of hypertension care and long‐term blood pressure control. J Am Heart Assoc 2020;9:e016174.
Clinical Topics: Cardiovascular Care Team, Dyslipidemia, Heart Failure and Cardiomyopathies, Prevention, Atherosclerotic Disease (CAD/PAD), Acute Heart Failure, Hypertension
Keywords: ACC Publications, Cardiology Magazine, Innovation, Retrospective Studies, Antihypertensive Agents, Blood Pressure, Heart Rate, Cardiovascular Diseases, Confidence Intervals, Hyperlipidemias, Health Educators, Patient Participation, Physician Executives, Sample Size, Risk, Pandemics, Diabetes Mellitus, Type 2, Follow-Up Studies, Coronary Artery Disease, Random Allocation, Heart Failure, Telemedicine, Hypertension, Stroke, Medicare, Monitoring, Physiologic, Referral and Consultation, Biomedical Technology, Technology, Physician Assistants, Software, Infarction, Phenotype, Mercury, Disease Management, Kidney
< Back to Listings