Cover Story | Hypertrophic Cardiomyopathy in 2021: New Insights, New Strategies and (Possibly) a New Treatment
Sixty years ago, hypertrophic cardiomyopathy (HCM) was considered a rare condition with an uncertain prognosis and limited treatment options. Today, it is understood to occur in 1 in 500 people in the general population and its reputation has been transformed by treatment innovations in sudden death prevention and the treatment of heart failure (HF) that have served to substantially reduce disease-related morbidity and mortality.
Currently, HCM is having a moment in the sun, with many of the management advances underscored in the recent HCM guideline, and, barring a rejection from regulators, the first new medical therapy in decades (see mavacamten sidebar).
"With a number of advances in contemporary cardiovascular therapies applied to HCM over the last couple of decades, we've made enormous improvements in both longevity and quality of life (QOL) of patients, such that nearly all patients diagnosed with HCM today can expect to achieve a normal life expectancy with a good QOL," says Martin S. Maron, MD, director of the HCM Center at Tufts Medical Center in Boston, MA, in an interview with Cardiology.
History of Medicine or Netflix Drama?
Advancing HCM Management
While being one of the most common cardiovascular genetic diseases, hypertrophic cardiomyopathy (HCM) is often undiagnosed, especially in women and underrepresented populations, with patients suffering substantial disease burden. With advances in treatment options and new therapies on the horizon, the ACC held its first Heart House Roundtable focused on HCM last month to identify and address opportunities and challenges in the delivery of guideline-directed care, as well as define forward-looking patient-focused innovations.
Topics tackled by the group included current standards and frontiers in diagnosis and treatment, including multimodality diagnostics, thresholds and interplay of therapies and the overlap of nonobstructive HCM and heart failure with preserved ejection fraction; population health, including access to specialty care, opportunities for value-based models in HCM, and the intersection of sex and race in HCM.
"HCM crosses many medical fields, from primary care to cardiology and in particular heart failure, to imaging, and also requires the full health care team, including pharmacists, nurse practitioners and others," noted a roundtable participant. Indeed, the roles of interdisciplinary and intersystem treatment was also addressed.
Specifically, participants noted a clear need for more awareness of HCM and clinician education, and improving accurate recognition and diagnosis of HCM, in part through better imaging quality and greater use of artificial intelligence, as well as improving the yield on family screening.
Acknowledging that access to specialty care is unequal and changes patient outcomes, goals and associated metrics are needed to improve access for all, increase inclusion of underrepresented patients in clinical trials and outcome studies, and increase clinician education including the next generation.
The HCM Patient Forum, held in conjunction with the roundtable, was an important opportunity to learn directly from patients about how HCM affects their quality of life and brought to light their concerns about the significant delay in access to an HCM expert, the desire for more shared decision-making, the need for patient education and support for the affect on their mental health.
The Roundtable and the Patient Forum were held as part of the College's new Accelerating Innovation for Medical Excellence in Hypertrophic Cardiomyopathy (AIME HCM) initiative. "Our goal with this initiative is to increase the awareness and understanding of HCM, activate clinicians, and optimize disease management to improve outcomes," said ACC President Dipti Itchhaporia, MD, FACC, in kicking off the Roundtable.
Visit ACC.org/HCM for the AIME HCM Hub and learn more about the roundtable and forum, as well as access CardioSmart patient resources and helpful clinician education and tools.
Although first documented in the second half of the 19th century, HCM went largely unrecognized as a clinical entity until the second half of the 20th century.
After the first patient report in 1868, there were a handful of seminal observations leading to HCM's breakthrough moment in the 1960s, according to an historical account written by Eugene Braunwald, MD, MACC, the main player in this story and widely considered the father of HCM.1,2
In 1929, a previously healthy 20-year-old student died suddenly while bike riding. On autopsy he was found to have an "enormous heart" with excessive hypertrophy, particularly of the left ventricle.3
Then, in 1949, William Evans, a London cardiologist, reported on five patients with idiopathic left ventricular hypertrophy (LVH) who came from three families.4 He dubbed the condition "familial cardiomegaly."
This was followed by an autopsy study in 1957, considered to be the first seminal series describing the morphologic findings of HCM in eight young adults with "asymmetrical hypertrophy" of the heart, seven of whom died suddenly,5 and a 1961 paper that reported a French-Canadian family from Quebec in whom 30 members across five generations were found to have HCM inherited in an autosomal dominant manner.6 (It was not until 1990 that the first causal gene for HCM was discovered.)
In 1958, Morrow and Braunwald identified two young men with intraventricular pressure gradients who they thought had an unusual congenital anomaly, membranous subaortic stenosis, but at the time of surgery during which cardiac contraction was halted, were found to have no outflow tract obstruction but did show LVH.7
Braunwald described in detail the clinical characteristics, natural history, and hemodynamics of the condition, especially the dynamic nature of the obstruction, the frequency of sudden death, autosomal transmission, and tested newly developed beta-blockers as medical treatment. During the same period, Morrow developed myectomy, a surgical procedure to relieve the subaortic obstruction that bears his name (the Morrow procedure).
Their combined efforts culminated in the seminal Circulation monograph published in 1964 that provided the initial description of HCM as a unique clinical entity, including its pathophysiology, and medical and surgical treatment.8 The monograph clocked in at 213 pages with 176 figures, 18 tables and 191 references. The NIH team called this new disease idiopathic hypertrophic subaortic stenosis.
"These men were like Lewis and Clark – they had no idea what was around the next corner, without any cardiovascular imaging to guide them, and they were able to put all the pieces together about this complex disease in a way that still stands true today," says Maron.
The myectomy procedure described by Morrow, while it has been further developed and advanced, is still the most widely used surgical intervention for HCM. Beta-blockers, developed in the 1960s and reported by Braunwald and colleagues to offer hemodynamic and clinical benefits, remain a mainstay of medical therapy.
"The history of HCM is just fascinating, with echocardiographic advances as one example," says Michelle M. Kittleson, MD, PhD, FACC, director of postgraduate education in heart failure and transplantation and director of heart failure research at the Smidt Heart Institute at Cedars-Sinai in Los Angeles, CA. "These giants of cardiology didn't have echocardiography. They did their physical exam and then determined the hemodynamic correlates on invasive cardiac catheterization, and with that information, they pioneered medical treatments and surgical myectomy."
"Just imagine taking a patient to the operating room for a surgical myectomy based just on clinical parameters, not actually being able to look at the heart and see how thick it is," she adds.
Martin S. Maron, MD
In a twist suitable to a Netflix series, Morrow himself developed obstructive HCM at the age of 40.8 His diagnosis was made solely by precordial auscultation and consideration of his symptoms by his close friend and collaborator, Braunwald.
Morrow's disease was particularly aggressive – he suffered from severe symptoms and ultimately died at 63 after a series of strokes.9 One of his two daughters and his only son also developed progressive forms of the disease involving arrhythmias, recurrent syncope, heart transplant (the daughter, at age 51), and subaortic obstruction causing severe HF symptoms (the son), reversed by a Morrow procedure. A 21-year-old granddaughter has HCM, completing a three-generation disease transmission.
The Evolution of Contemporary HCM Management
HCM Guideline Hub: Practice Support
The ACC's HCM Guideline Hub provides a central repository of clinician tools and resources needed under the new ACC/AHA HCM guideline.
Among the hub highlights: an HCM Guidelines Made Simple document available in English, Spanish, Portuguese and Chinese, outlining the top 10 take-home messages from the guideline; focused HCM guideline slide sets; expert commentary and sample case studies; CME and MOC education opportunities; and more. Also find a CardioSmart patient summary and infographic to help increase patient knowledge and engagement in shared decision-making. Click here to visit and bookmark the Hub.
Test your knowledge and earn credit with two HCM Guideline-focused case reports in JACC: Case Reports. Click here for the case on shared decision-making for sports participation.
Visit the HCM Guideline section on JACC.org to access the second case, as well as additional JACC Journals resources.
As a complement to the ACC/AHA Guideline Optimization effort, a new tool on ACC.org was launched to help users more easily search within guidelines. The new search tool can be found at ACC.org/Guidelines. Click here for a tutorial video on optimizing your use of this new tool.
The 2020 ACC/AHA Guideline for the Diagnosis and Treatment of Patients With Hypertrophic Cardiomyopathy offers a full revision of the previous 2011 guideline.10 And while the treatments for HCM, medical and interventional, have not changed substantially in decades (mavacamten is not covered in the new guideline because it is not yet approved), the management strategies have evolved in important ways.
"We're getting better and better at managing this disease – the risk of sudden cardiac death (SCD), arrhythmias, stroke prevention and reversal of refractory HF symptoms – and the new guideline explains all this," says Maron, who was on the writing committee.
Another of the guideline writers, Kittleson, provided an engaging and comprehensive summary of the changes during a session devoted to HCM at ACC.21. (Click here to view the on-demand session on the Guidelines Channel.)
The guideline, she notes, runs to 74 pages and 133 recommendations, but comes with "Top 10 Take-Home Messages" to help clinicians absorb the most important details (available in the ACC.org Guideline Hub). Provided here are a few of the take-home messages particularly relevant to the general cardiologist.
HCM Centers: When to Refer?
General cardiologists should feel comfortable making the diagnosis of HCM looking at symptoms, the physical exam, initial EKG, echocardiogram, and family history, according to the guideline. They can also make initial treatment recommendations and do a rapid assessment for changes in the disease course.
"General cardiologists might feel more comfortable referring patients for confirmation of the diagnosis and for genetic testing and counseling, or for advanced treatment decisions like whether to consider septal reduction therapies or defibrillators in some cases for primary prevention of SCD," says Kittleson.
Michelle M. Kittleson, MD, PhD, FACC
While there were no explicit recommendations in the 2011 guideline for when to refer, the new guideline says a referral should be made for Class 2b ICD decision-making, septal reduction therapies, advanced HF management, and decision-making surrounding high-intensity or competitive sports, pregnancy and pediatric HCM.
SCD Risk Assessment
HCM Management Pearls of Wisdom
Kittleson, known for her #kittlesonrules on Twitter, shared some management pearls for Cardiology readers.
- In obstructive HCM, target therapy to the patient's symptoms, not the gradient seen on echo "because the gradient is dynamic. What you really want to know is whether their symptoms improve on treatment."
- If a patient has any element of obstructive HCM, advanced therapies like heart transplantation and LVADs are never indicated because, by definition, obstructive HCM is treatable either with medications or invasive septal reduction therapies.
- Traditionally, in HF with reduced EF, the LVEF cutoff is <40%. But for HCM, an EF <50% is considered HF and should trigger discussions around ICDs, cardiac resynchronization therapy, and guideline-directed medical therapy because an EF <50% connotes significantly impaired systolic function and identifies individuals with a poor prognosis.
- Don't be fooled by a "normal" EF. There are some patients who develop restrictive physiology and severe symptoms with no fall in EF. These patients can still be sick enough to need a transplant. So, don't use EF alone to guide you.
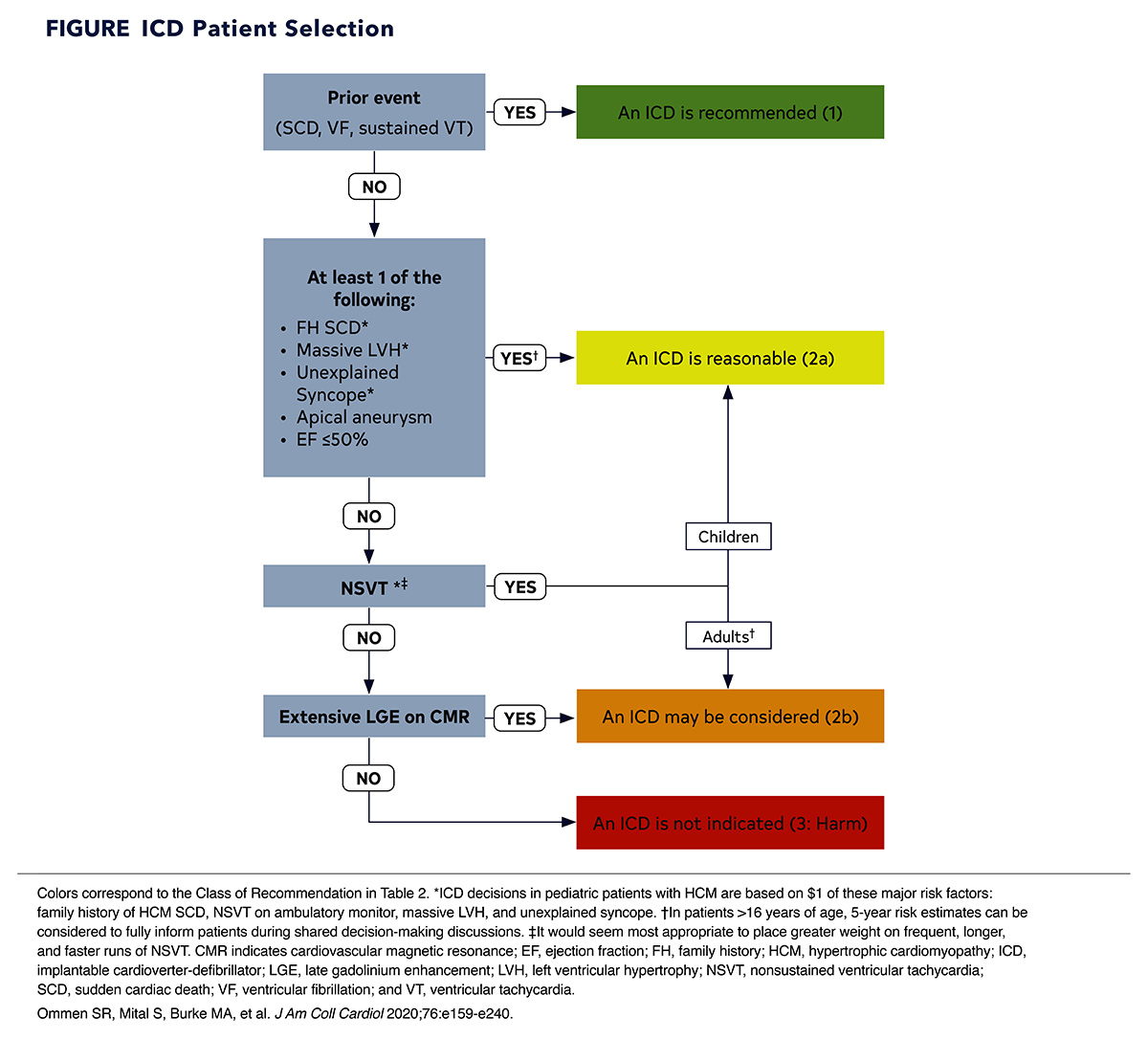
SCD remains a devastating consequence of HCM, making risk stratification and patient selection for ICD device therapy important (Figure). But the story is very different from what it was even a few years ago.
"Risk stratification in HCM has matured to the extent that we can identify almost all patients today who are at risk of SCD and provide them with protection in the form of an ICD. This is a remarkable statement to make and light years different from a time not that long ago when you gave a patient a beta-blocker and hoped you didn't get a phone call that they had died," says Maron.
"Back in the olden days we used to put everyone with HCM on a treadmill to see if their blood pressure dropped during exercise because that was a finding that signaled the need for a defibrillator," says Kittleson.
Now, studies have shown this is not an independent risk factor for SCD, nor is the degree of LV outflow tract obstruction and the presence of genetic mutations, she says.
"What has been bumped up in importance is an ejection fraction (EF) less than 50%, the presence of an LV apical aneurysm, and the presence of extensive gadolinium enhancement," says Kittleson, which also emphasizes the increased importance given to the role of MRI in risk stratification.
Sports and Exercise
Another important change in the new guideline pertains to sports and activity. In the old guideline, low-intensity aerobic exercise was 'reasonable,' and "that was a generally proscriptive and narrow Class IIa recommendation with a Level of Evidence of C," says Kittleson.
The new guideline has incorporated research from the past decade showing that in patients with HCM, sudden death is generally rare in exercise and that a moderate-intensity recreational exercise program is not only safe, but encouraged for most patients with HCM, just like for the general population.
"Encouraging exercise may make some cardiologists feel nervous. But they should feel comfortable telling patients with HCM to play some doubles tennis or go on a hike. Patients should limit themselves based on their symptoms and go at a pace that feels comfortable," she says.
In terms of participation in competitive sports, that should "absolutely" be deferred to a comprehensive HCM center and an HCM specialist "because there is a lot of gray area and a lot of shared decision-making around this," Kittleson adds.
"It's really all about shared decision-making, which we've also spoken about in the guideline more explicitly and in more detail," she notes.
"The updated guideline is extremely important for us to put into context new therapies as they come along. There's a lot of expertise and new data since the last guideline about what works and what doesn't. This is important to consider as we think about how treatments like mavacamten fit into the picture," says Daniel Jacoby, MD, founder and director of the cardiomyopathy program at Yale Medical School and an investigator with the EXPLORER-HCM trial of mavacamten.
The Promise That is Mavacamten
Mavacamten is big news in the HCM world. It's a first-in-class, cardiac-specific myosin inhibitor that reduces the number of available actin-myosin cross-bridges and thus decreases excessive myocardial contractility, improving symptoms and QOL in patients with obstructive HCM.1 In the phase 3 EXPLORER-HCM trial, mavacamten (vs. placebo) met its primary endpoint, a ≥1.5 mL/kg/min increase in peak oxygen consumption (pVO2) and at least one NYHA class reduction or a ≥3.0 mL/kg/min increase in pVO2 and no NYHA class worsening.1
In the study arm, 37% of patients reached the primary endpoint vs. 17% in the placebo arm (difference +19.4%; p=0.0005). More mavacamten patients experienced both complete relief of symptoms (class I) and outflow gradients to ≤30mm Hg (20.3% vs. 7.8% for placebo; p=0.0005).
Mavacamten-treated patients showed greater reductions in post-exercise left ventricular outflow tract (LVOT) gradient vs. placebo (—36 mm Hg; p<0.0001) and greater increase in pVO2 (+1.4 mL/kg/min; p=0.0006). About one-third more patients in the mavacamten group improved by at least one NYHA class (p<0.0001), with no safety or tolerability signals observed. However, it should be noted, as well, that two-thirds of mavacamten-treated patients did not achieve the study endpoint, and 50% of patients were still limited by class II-III symptoms with relatively modest improvements in functional capacity.

Daniel Jacoby, MD
The trial was conducted in 251 patients enrolled at 68 clinical centers in 13 countries. Participants had an LVOT obstruction gradient of ≥50 mm Hg and NYHA class II–III symptoms. Randomization was to mavacamten or placebo for 30 weeks.
In his virtual presentation of the main results at ESC Congress 2020, principal investigator Iacopo Olivotto, MD, called the findings a breakthrough that the community has been working towards for 60 years. "Nearly 75% of patients saw a reduction below guideline-defined thresholds for invasive septal reduction therapy and 56% showed complete relief of obstruction," he reported.
It's All About Symptoms
HCM is usually asymptomatic, but when symptoms appear – exercise intolerance, fatigue, angina, syncope – the effect on QOL can be profound and the primary goal of treatment is to alleviate symptoms.
In a Late-Breaking Clinical Trial session at ACC.21, John Spertus, MD, MPH, FACC, presented health status outcomes for the EXPLORER-HCM trial, with findings simultaneously published in the Lancet.2
At 30 weeks, the change in Kansas City Cardiomyopathy Questionnaire (KCCQ) score was greater with mavacamten than placebo (mean scores, 14.9 vs. 5.4, difference, +9.1; p<0.0001), with similar benefits across all subscales of the KCCQ.
About one in three patients treated with mavacamten (36%) had a ≥20-point change in their overall summary score, vs. 15% of the placebo arm, for an estimated absolute difference of 21% and number needed to treat of five. In a small subgroup with available data, these gains disappeared after treatment cessation.
"We have never in the 60-year history of this disease had a prospective, randomized, double-blind, placebo-controlled medication trial of this size showing this magnitude of benefit," says Jacoby. He expects the drug will likely be approved.
But with that, it's also important to be discerning about what the trial did and did not show. "EXPLORER-HCM was not a trial for people who were going to get or were interested in getting septal myectomy. Neither was this a trial that directly compared medical therapy and substrate reduction therapy,so we really should be careful about comparing these randomized data from EXPLORER-HCM with retrospective, observational data that we have on medical therapies and septal reduction," says Jacoby.
For his part, Maron is less bullish. "It decreases contractility of the heart, which decreases mitral valve-septal contact duration and as a result, can lower outflow tract gradients in many patients with obstruction. In principle, doing this can be expected to improve symptoms and it appears mavacamten does this in some patients, as we saw in EXPLORER-HCM," says Maron.
"But what EXPLORER-HCM did not show is a disease-modifying effect in terms of wall thickness, fibrosis, energetics, things like that," he adds. We also need longer-term data on the drug, he feels, to understand how residual gradients impact longer-term efficacy. Maron is the principal investigator for the REDWOOD-HCM trial, a phase 2 trial of a second-generation myosin inhibitor, CK-274 (Cytokinetics), which has a shorter half-life than mavacamten.3 The trial is still recruiting.
Cost is also an important consideration, says Maron. "If this drug is like tafamidis, and I expect it will be, costing upwards of $80,000 or more a year, and the alternative is a one-time low-risk septal reduction therapy, there will likely be backlash."
Kittleson is taking a cautious but hopeful approach. "Will it be a substitute for septal reduction therapy? Probably not. Will it be an adjunctive therapy to beta-blockers, calcium channel blockers, and disopyramide? Potentially. Will it be good for patients who need septal reduction therapy, but for whatever reason, anatomically or because of their frailty or comorbidities aren't candidates? Maybe," she says.
Meanwhile, currently mavacamten is not approved anywhere. In the fall of 2020, shortly after the initial EXPLORER-HCM results were presented, Bristol Myers Squibb bought MyoKardia, the developers of mavacamten and an application for approval has been made to the U.S. Food & Drug Administration with a Prescription Drug User Fee Act (PDUFA) goal date of January 28, 2022.
References
- Olivotto I, Oreziak A, Barriales-Villa R, et al. Mavacamten for treatment of symptomatic obstructive hypertrophic cardiomyopathy (EXPLORER-HCM): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2020;396:759-69.
- Spertus JA, Fine JT, Elliott P, et al. Mavacamten for treatment of symptomatic obstructive hypertrophic cardiomyopathy (EXPLORER-HCM): health status analysis of a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2021;May 14:[Epub ahead of print].
- Argirò A, Zampieri M, Berteotti M, et al. Emerging medical treatment for hypertrophic cardiomyopathy. J Clin Med 2021;10:951.
Fuster's Top Five Influencers (Papers, that is) on HCM
Cardiology asked JACC Editor-in-Chief Valentin Fuster, MD, PhD, MACC, to weigh in with his thoughts on the most important papers published in the Journal of the American College of Cardiology over the past five years that have helped to move the needle forward on our understanding and treatment of hypertrophic cardiomyopathy (HCM).
His top five picks are as follows:

Evaluation of Mavacamten in Symptomatic Patients With Nonobstructive Hypertrophic Cardiomyopathy
Ho CY, Mealiffe ME, Bach RG, et al.
Importance of paper? In nonobstructive HCM, which makes up approximately half of all HCM cases, available therapeutic options are currently very limited. This study offers some hope. Read the paper.

Distinct Subgroups in Hypertrophic Cardiomyopathy in the NHLBI HCM Registry
Neubauer S, Kolm P, Ho CY, et al.
Importance of paper? A description of MRI, genetic, and biomarker findings, with two groups evolving from these three variables: a sarcomere mutation-positive group more likely to have reverse septal curvature morphology, more fibrosis, but less resting obstruction; and a sarcomere mutation-negative group more likely to have isolated basal septal hypertrophy, obstruction, but less fibrosis. Only a long follow-up will tell us about the risk stratification and/or prognosis for these two groups. Read the paper.

Penetrance of Hypertrophic Cardiomyopathy in Sarcomere Protein Mutation Carriers
Lorenzini M, Norrish G, Field E, et al.
Importance of paper? The study, combined with other studies from other research groups worldwide over three decades, suggests that penetrance of HCM is likely determined by a number of environmental and genetic influences in addition to the primary disease-causing sarcomere variant. The take-home messages from this study are that 1) genetic testing should be performed in patients with HCM and, depending on results, in first-degree family members, and 2) because disease may present in early childhood, clinical screening should perhaps commence at an earlier age. Read the paper.

Survival After Alcohol Septal Ablation in Patients With Hypertrophic Obstructive Cardiomyopathy
Batzner A, Pfeiffer B, Neugebauer A, et al.
Importance of paper? For more than 50 years, surgical myectomy was the gold standard for treatment of symptomatic patients with high outflow tract gradients, but more than two decades ago alcohol septal ablation was introduced as another treatment option. This study provides long-term follow-up data for patients who had undergone percutaneous transluminal septal myocardial ablation, which proved to be a good and safe procedure, with ongoing symptomatic improvement and excellent long-term survival. Read the paper.

Late Gadolinium Enhancement in Patients With Hypertrophic Cardiomyopathy and Preserved Systolic Function
Mentias A, Raesi-Giglou P, Smedira NG, et al.
Importance of paper? This history of sudden cardiac death and risk stratification in patients with HCM has had a continuous evolution. This study adds an important variable for such risk stratification – late gadolinium enhancement (LGE) on cardiac MR. It is the first paper to extend the importance of LGE findings into both obstructive and nonobstructive subgroups, as well as in the context of patient. Read the paper.
References
- Braunwald E. Hypertrophic cardiomyopathy: The first century 1869-1969. Glob Cardiol Sci Pract 2012;2012:5. doi:10.5339/gcsp.2012.5
- Naidu SS, ed. Hypertrophic Cardiomyopathy. Foreword by Bernard Gersh and Historical Context by Eugene Braunwald. Springer-Verlag, NY; 2015.
- Whittle CH. "Idiopathic" hypertrophy of the heart in a young man. Lancet 1929;213:1354-55.
- Evans W. Familial cardiomegaly. Br Heart J 1949;11:68-82.
- Teare D. Asymmetrical hypertrophy of the heart in young adults. Br Heart J 1958;20:1-8.
- Pare JA, Fraser RG, Pirozynski WJ, Shanks JA, Stubington D. Hereditary cardiovascular dysplasia. A form of familial cardiomyopathy. Am J Med 1961;31:37-62.
- Morrow AG, Braunwald E. Functional aortic stenosis; a malformation characterized by resistance to left ventricular outflow without anatomic obstruction. Circulation 1959;20:181-9.
- Braunwald E, Lambrew CT, Rockoff SD, Ross J, Morrow AG. Idiopathic hypertrophic subaortic stenosis. I. A description of the disease based upon an analysis of 64 patients. Circulation 1964;30:SUPPL 4:3-119.
- Maron BJ, Roberts WC. The father of septal myectomy for obstructive HCM, who also had HCM. J Am Coll Cardiol 2016;67:2900-3.
- Ommen SR, Mital S, Burke MA, et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2020;76:e159-e240.
Clinical Topics: Arrhythmias and Clinical EP, Cardiac Surgery, Cardiovascular Care Team, Congenital Heart Disease and Pediatric Cardiology, Diabetes and Cardiometabolic Disease, Geriatric Cardiology, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Prevention, Sports and Exercise Cardiology, Vascular Medicine, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Aortic Surgery, Cardiac Surgery and Arrhythmias, Cardiac Surgery and CHD and Pediatrics, Cardiac Surgery and Heart Failure, CHD and Pediatrics and Arrhythmias, CHD and Pediatrics and Imaging, CHD and Pediatrics and Interventions, CHD and Pediatrics and Prevention, CHD and Pediatrics and Quality Improvement, Statins, Acute Heart Failure, Heart Transplant, Interventions and Imaging, Interventions and Structural Heart Disease, Interventions and Vascular Medicine, Echocardiography/Ultrasound, Magnetic Resonance Imaging, Exercise, Sports and Exercise and Congenital Heart Disease and Pediatric Cardiology, Sports and Exercise and Imaging
Keywords: ACC Publications, Cardiology Magazine, Aneurysm, Arrhythmias, Cardiac, Auscultation, Autopsy, Benzylamines, Bicycling, Blood Pressure, Boston, Calcium Channel Blockers, Canada, Cardiac Catheterization, Cardiac Myosins, Cardiac Resynchronization Therapy, Cardiology, Cardiomyopathies, Cardiomyopathy, Hypertrophic, Constriction, Pathologic, Contrast Media, Counseling, Death, Sudden, Death, Sudden, Cardiac, Decision Making, Defibrillators, Disopyramide, Double-Blind Method, Echocardiography, Electrocardiography, Exercise, Exercise Therapy, Family Characteristics, Fatigue, Fibrosis, Frail Elderly, Friends, Gadolinium, Genetic Testing, Goals, Half-Life, Heart Failure, Heart Transplantation, Heart Ventricles, Hemodynamics, History of Medicine, Hypertrophy, Left Ventricular, Kansas, Life Expectancy, London, Longevity, Los Angeles, Magnetic Resonance Imaging, Mercury, Mitral Valve, Morbidity, Mutation, Myosins, Nuclear Family, Operating Rooms, Oxygen Consumption, Patient Selection, Physical Examination, Pregnancy, Prescription Drugs, Primary Prevention, Prognosis, Prospective Studies, Quality of Life, Quebec, Random Allocation, Referral and Consultation, Retrospective Studies, Risk Assessment, Risk Factors, Schools, Medical, Social Media, Stroke, Stroke Volume, Students, Syncope, Tennis, Uracil, Ursidae, Ventricular Pressure, Withholding Treatment, Writing, Young Adult, ACC21, ACC Annual Scientific Session
< Back to Listings