New in Clinical Guidance | New ACC Guidance Addresses Obesity Treatment Strategies Across the CV Spectrum; More
As obesity continues to drive cardiovascular risk, the ACC has released two new guidance documents to support clinicians: Concise Clinical Guidance (CCG) on the medical management of obesity and a Scientific Statement focused on treating obesity in adults with heart failure. Both underscore the need for individualized, evidence-informed strategies that leverage emerging therapies and evolving clinical insights to reduce weight and improve cardiovascular outcomes.
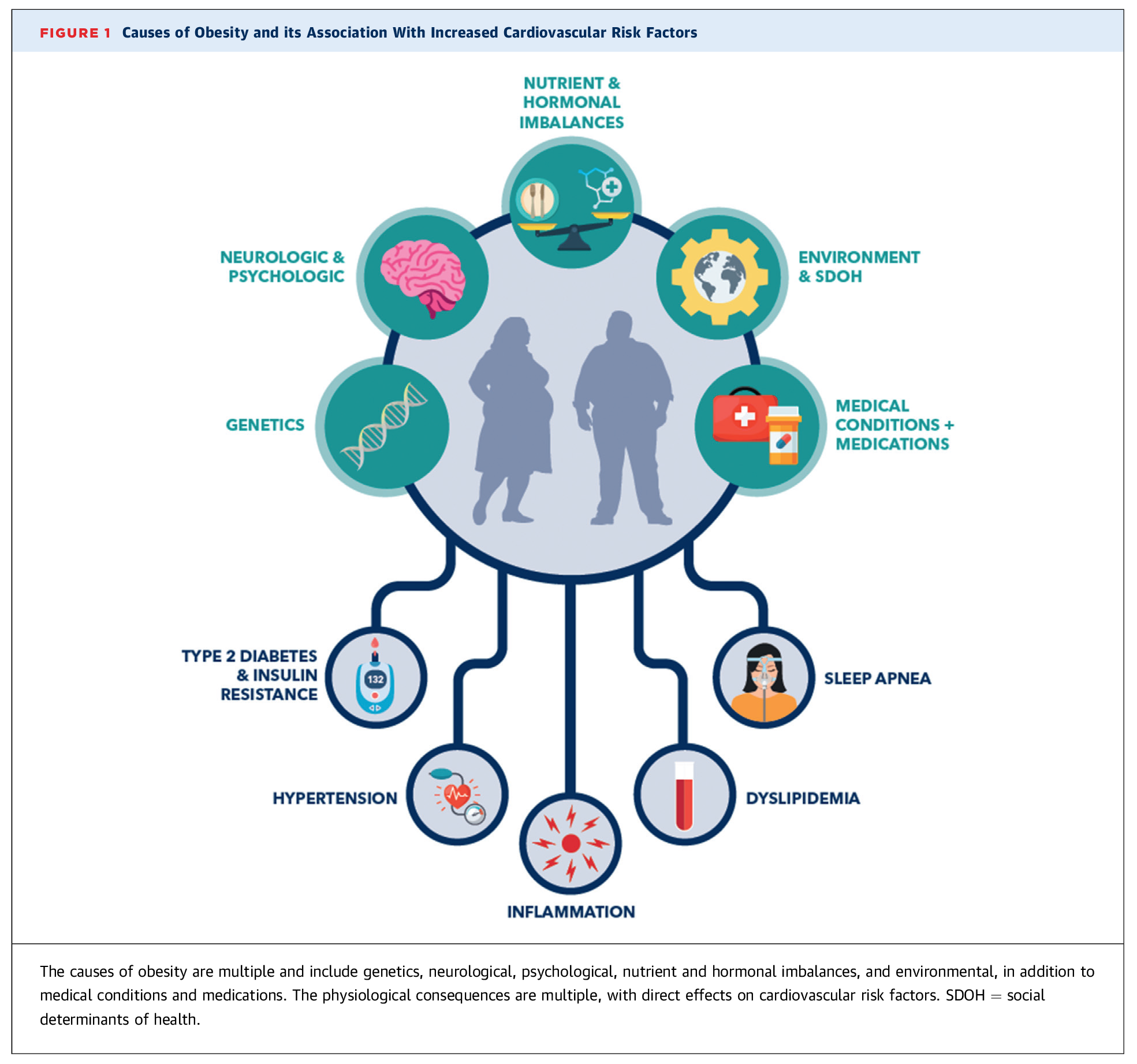
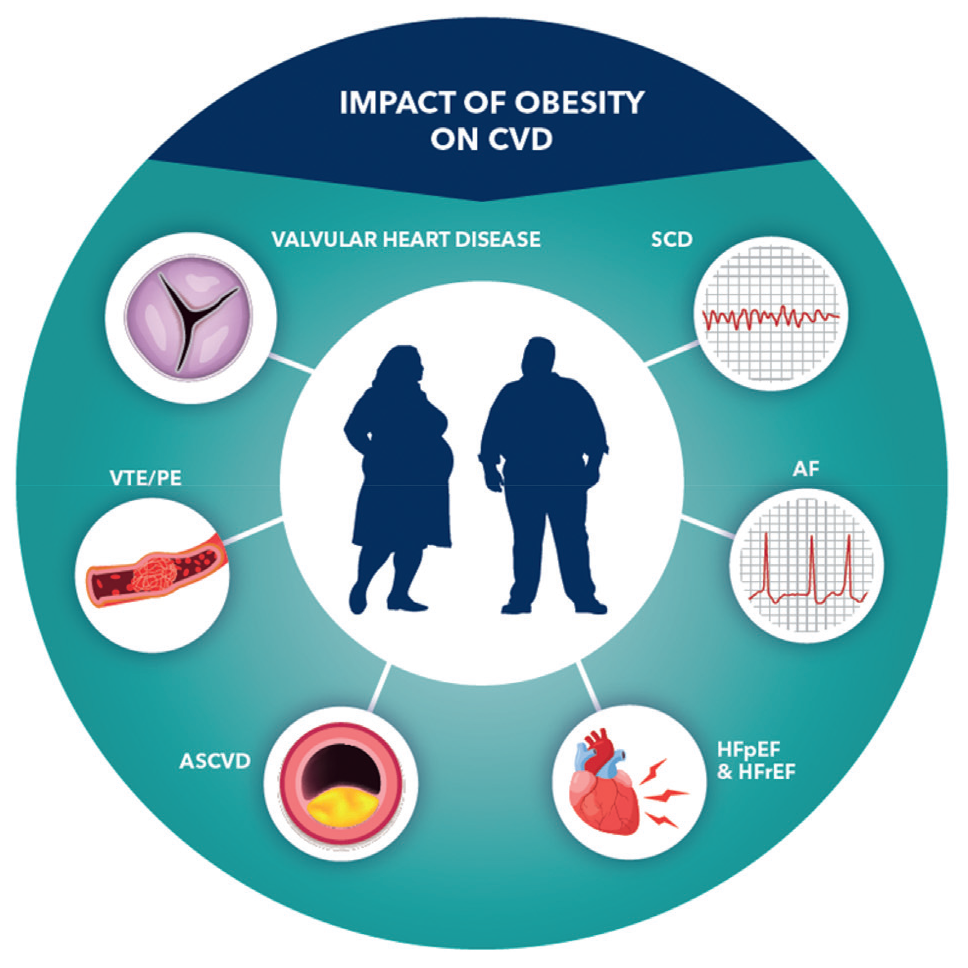
The CCG, led by Chair Olivia Gilbert, MD, MSc, FACC, and Vice Chair Martha Gulati, MD, MS, FACC, highlights the multiple causes of obesity, including genetic, neurological and psychological factors, as well as nutrient and hormonal imbalances, environmental and social determinants of health, and medical conditions and medications. It also discusses obesity-related cardiovascular disease risks like sleep apnea, dyslipidemia, inflammation, hypertension and type 2 diabetes, which can increasingly be addressed with modern obesity medications with fewer risks than procedure-based interventions.
Unhealthy weight has been linked to 60+ conditions, including heart risk factors, #CVD, #cvMI and #Stroke. Download the latest CardioSmart infographic supporting the ACC's new Concise Clinical Guidance on medical weight management.
Importantly, the CCG also outlines the clinical decision-making process for clinicians to incorporate these and future pharmacologic weight management strategies into cardiovascular care, highlighting the following key areas:
- Rationale and Eligibility – Pharmacotherapy strikes the balance between effectiveness and invasiveness. Eligibility may be determined by BMI thresholds or other risk indicators. These therapies can be adjusted to minimize adverse effects and personalize care.
- Pharmacological Options – Among U.S. Food and Drug Administration-approved medications, the GLP-1 receptor agonist semaglutide and the GLP-1/GIP receptor agonist tirzepatide have demonstrated the highest efficacy. Clinical trial and real-world observational data support slightly greater weight loss with tirzepatide. Insurance coverage, availability and affordability are likely to dictate agent selection.
- Impact on Cardiovascular Risk – Clinical evidence supports medications leading to a reduction in major adverse cardiovascular events – including cardiovascular death, myocardial infarction and stroke – particularly in individuals with type 2 diabetes and elevated cardiovascular risk.
- Multidisciplinary Care Approaches – Team-based approaches are critical for effective weight management, helping to assess modifiable risk factors, identify comorbidities and tailor treatment strategies.
- Reducing Bias and Improving Experience – Clinicians should make every effort to validate the lifelong journey that patients experience with this chronic disease, placing emphasis on person-first language, creating welcoming clinical environments and addressing weight stigmas.
- Access Considerations – Lack of insurance coverage remains a major barrier for patients. Initial strategies to improve access to therapies include identifying individuals most likely to benefit, close monitoring of treatment outcomes and price negotiations.
"Patients should not be required to 'try and fail' lifestyle changes prior to initiating pharmacotherapy; nonetheless, lifestyle interventions should always be offered in conjunction with obesity medications," said Gilbert. "Weight management by the cardiovascular community needs to be embraced, given both the prevalence of obesity and the impact it has on many forms of [cardiovascular disease]."
In the new ACC Scientific Statement, the College addresses the management of obesity in adults with heart failure (HF), with a specific focus on those with stage 2 HF with preserved ejection fraction (HFpEF). The statement is the first in a new series of clinical guidance from the College aimed at informing clinicians about areas where evidence is new and evolving or where sufficient data are more limited.
The statement, led by Writing Committee Chair Michelle M. Kittleson, MD, PHD, FACC, provides an overview of the latest evidence and current challenges in HF management and reviews the existing processes for diagnosis, evaluation and risk assessment of obesity in HF. It also includes a series of consensus recommendations regarding the epidemiology of obesity in HF and the diagnosis of obesity, risk assessment, and evaluation of obesity and HF.
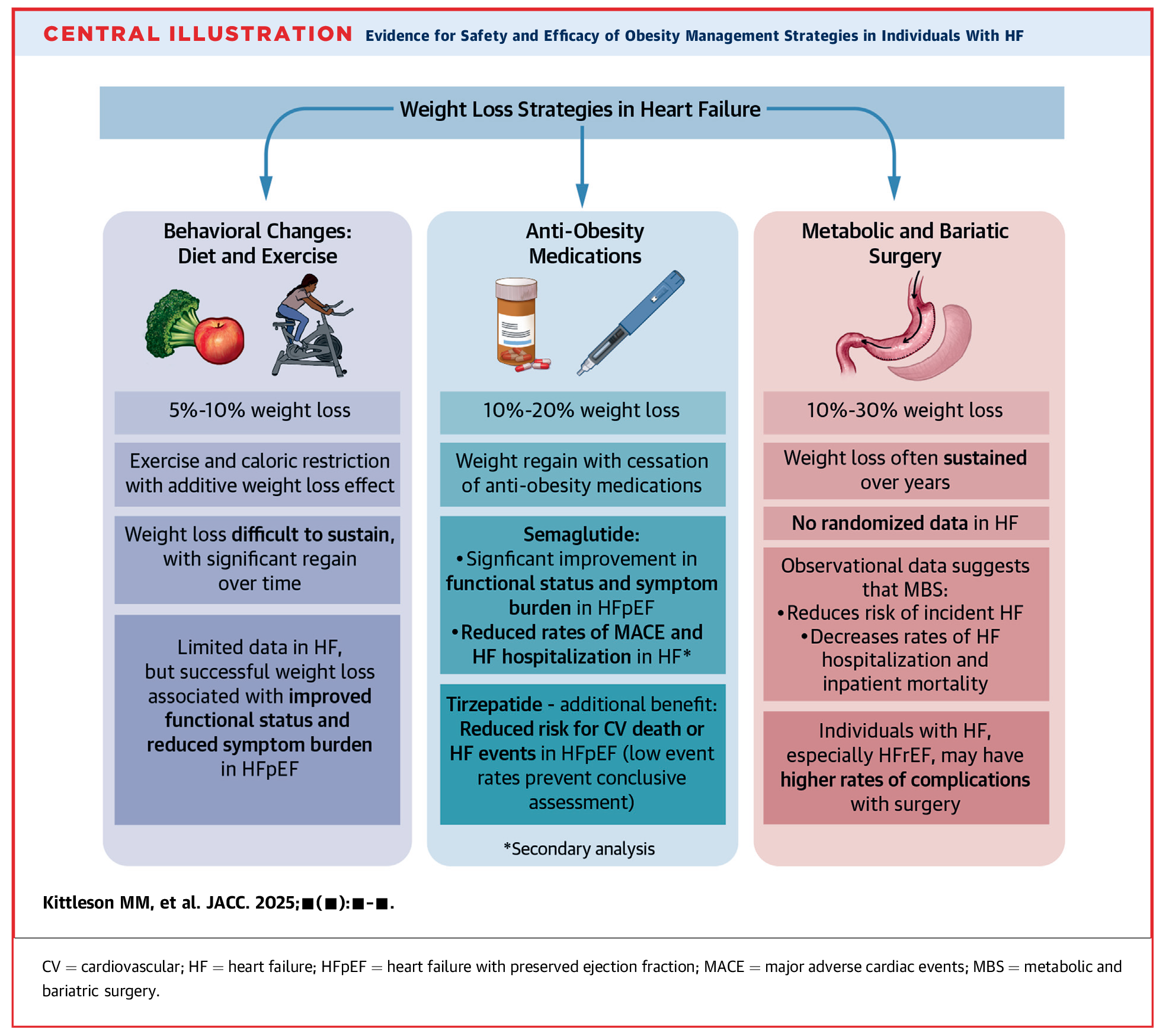
Recommendations for specific lifestyle, behavioral, pharmacological and invasive interventions for the management of obesity in HF are also included. Of note, the Central Illustration summarizes current evidence surrounding the safety and efficacy of weight loss strategies including behavioral changes like diet and exercise, anti-obesity medications (AOM) like semaglutide and tirzepatide, and metabolic and bariatric surgery.
In addition to clinical guidance, the statement also includes a closer look at evidence gaps and opportunities for further research, including a closer look at what intentional weight loss strategy offers the greatest HF benefit, the role of cardiometabolic health clinics in HF care, and whether AOMs may improve outcomes in individuals with HF with reduced ejection fraction (HFrEF).
Read the Scientific Statement in JACC.
Cardiac CT Imaging to Assess Prosthetic Heart Valves
A new multisociety expert consensus document co-authored by the ACC, the Society of Cardiovascular Computed Tomography, the European Society of Cardiovascular Radiology, the North American Society of Cardiovascular Imaging, the Radiological Society of North America, the Society for Cardiovascular Angiography & Interventions and Society of Thoracic Surgeons (STS) addresses the evolving use of cardiac CT imaging and how to best use it to assess different types of prosthetic heart valve (PHV) dysfunction.
The document, led by Writing Group Chair Ricardo P. J. Budde, MD, PhD, provides an overview of heart valve repairment techniques and summarizes the available imaging modalities for PHV, including transthoracic and transesophageal echocardiography, CT imaging, cine fluoroscopy and nuclear imaging. It then dives deeper into CT acquisition protocols for PHV imaging; CT findings in normal functioning PHV; types of PHV dysfunction; (para)valvular leakage; patient prosthesis mismatch; endocarditis; structural valve deterioration/dysfunction; and hypo-attenuated leaflet thickening – providing consensus statements based on the latest data available and expert opinion.
Keywords: Cardiology Magazine, ACC Publications, Glucagon-Like Peptide 1, Weight Loss, Semaglutide, Obesity