Introduction to Cardio-Oncology

Cardio-oncology is neither the science nor the practice of treating heart tumors, rather an emerging multidisciplinary field that focuses on the cardiovascular management (prevention, diagnosis and treatment) of patients with cancer.
The core objective of the cardio-oncology discipline is to ensure that "the cancer patient of today does not become the heart patient of tomorrow."
What are the historic roots of cardio-oncology and how did it become an established niche in cardiovascular medicine?
In 1929, Thibauduau first reported marked pathological changes in the myocardium of 10 patients who underwent wide-field thoracic radiation.
These abnormalities ranged from mild interstitial fibrosis to muscle fiber degeneration and frank necrosis. Over the ensuing decades, investigators have shown that the culprit mechanisms underlying radiation-induced cardiac disease were endothelial cell damage, microvascular dysfunction and macrovascular injury.
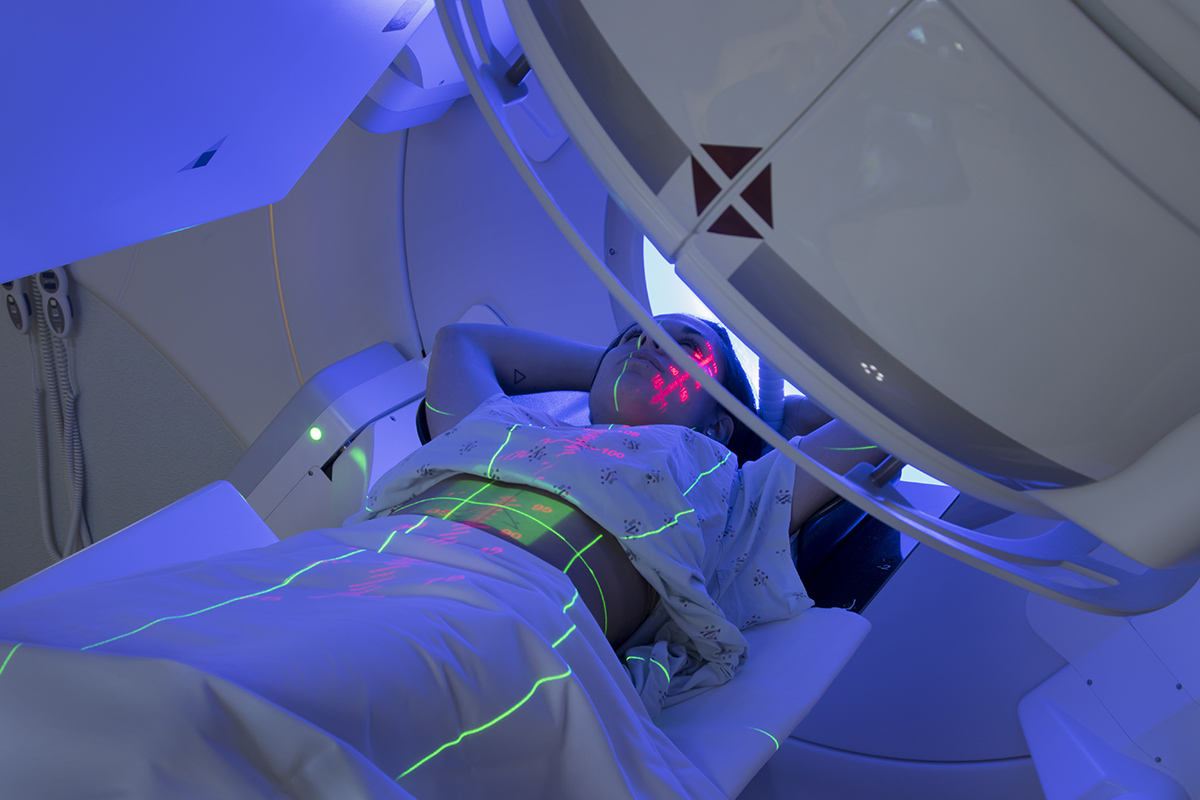
It was later found that thoracic radiation can grossly affect any level of the cardiovascular system, and may result in premature atherosclerosis, valvular heart disease, pericarditis, cardiomyopathy and arrhythmias.
Subsequent decades have also revealed a rise in heart failure cases among breast cancer patients who received anthracycline chemotherapies. An epidemiological link between the use of anthracycline drugs and cardiomyopathy was recognized and its biologic mediators were later determined to be oxidative stress, mitochondrial injury and topoisomerase 2-ß inhibition.
These historical anecdotes served as the impetus for the systematic study of cardiotoxicity in oncology.
While cardiologists were working hard to acquire a basic understanding of chemotherapy- and radiation-induced cardiac dysfunction, oncologists continued to make substantial strides in the treatment of cancer patients.
Utilizing novel monoclonal antibody-based therapies, targeted biologic inhibitors and immune-based compounds, they were successful in significantly boosting patient response and cure rates as well as extending survival.
As patients' cancer outcomes have improved, and while interest in the cardiovascular sequel of anti-cancer therapies increased, cardiotoxicities have emerged with a variety of anti-cancer drugs.
These signals-turned-cardiotoxic phenomena were quickly found to be a highly-varied cluster of manifestations that result from pathologic activation or suppression of fundamental biologic pathways.
Some were characterized by the reversibility of the cardiac derangement while others were permanent. Some resulted in toxicity when used alone, others when administered in combination with other cardio-injurious interventions.
The landscape of therapy-induced cardiotoxicity has thus expanded over time, reaching the point where it now demands expertise in both the cancer process and its therapies, as well as the spectrum of cardiovascular manifestations.

With cardio-oncology reflecting the integration of two subspecialties comes its nature of a team-based multi-collaborative enterprise. Oncologists define the cancer treatment goal (definitive/curative intent; palliative) based on a myriad of patient- and tumor-related factors yet generally lack expertise in cardiovascular risk assessment.
Cardiovascular clinicians, on the other hand, may well understand a targeted drug's potential implications on the myocardium, the vasculature, or heart valves, but are deficient in the comprehension of the overall cancer prognosis as well as the long-term outcomes of alternative anti-cancer treatment options.
It was obvious, then, that a unique breed of a cardiovascular clinician, one mastering both the cardiovascular profile of a host, the basic principles of the care of a cancer patient, and the acute and late consequences of anti-cancer therapies, was needed.
Therefore, cardio-oncology has emerged as a high-level equilibrium exercise whose premise is the evidence-based optimization of both cardiovascular well-being and cancer treatment.
