Navigating Consults as a Fellow

On the first day of my cardiology fellowship, I found myself in a new role on the consult service. No longer the primary doctor for my own group of patients in the hospital, I was now weighing in on cardiology questions for patients across the hospital and was at the ready for any cardiology problems that came up. The role of a consultant is one that we often find ourselves in as Fellows in Training (FITs) on dedicated consult rotations and on call, and it is new territory for many of us as we transition from residency.
This transition is an exciting one; we get to be accessible experts, using our growing body of knowledge in cardiology to help patients and teach our colleagues in the hospital. It is also a very challenging transition. This role carries a high cognitive load for FITs. We must address complex clinical questions (often for critically ill patients) while coping with the external cognitive load of work accumulating from prior consults and new pages to triage, all the while trying to learn to help take better care of our current and future patients. And providing an effective consultation goes beyond knowing the literature or having the technical skill to perform procedures. There are communication challenges unique to the consultant role that take time and thought to navigate well.
A framework for the cognitive load during consults
The consult service has a heavy workload, with complex cases and competing distractions. One study explored the fellow experience in this environment and developed a framework based on cognitive load theory.
In their qualitative analysis, they found four themes that encompassed the cognitive load on fellows during consults:
- The nature and scope of the consult (complex clinical questions)
- Leveraging resources to create a network (coordination, including arranging for procedures, communicating with primary team, the patient and family, and other consultants)
- Extraneous tasks (documentation from prior consults, triaging pages)
- Fellow learning
This language has helped me understand how I feel during consult rotations and manage my time more effectively. For example, I can put a finger on why I am feeling particularly drained after spending a lot of time coordinating input from multiple specialists and arranging an urgent procedure. Having acknowledged this, I can reset and redirect my focus on the next task. For example, if our attending wants to spend a few minutes teaching but I’ve just received multiple pages, I might ask to return some pages first or reschedule so that I can truly focus on learning.
In addition, this framework serves to remind me of all the different ways I am learning during this rotation. For each consult question, there is self-directed learning as I read or dig up guidelines to help direct next steps in care. In addition, I get to teach the primary team or junior members of my consult team about what I have learned, which helps me solidify knowledge. This process is iterative and learning from one consult makes the next less daunting.
How to make sure your consults are helpful to others
Learning how to consult is not something that is often taught in medical school or residency, and therefore the mechanics of this process are often overlooked or learned through trial and error. In 1983, Lee Goldman, MD, and colleagues published "Ten Commandments for Effective Consultation" to address this gap and provide a structure for consulting physicians to work within.
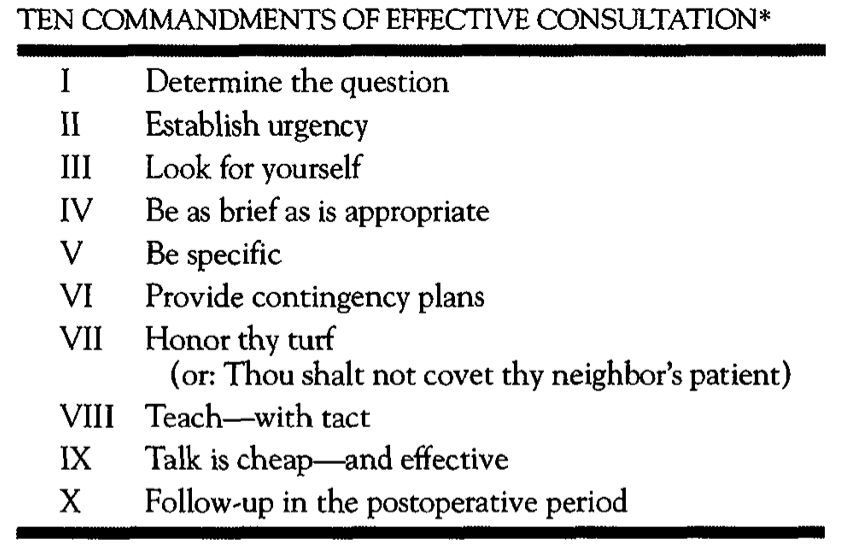 Figure. Ten Commandments of Effective Consultation from Goldman, et al.
Figure. Ten Commandments of Effective Consultation from Goldman, et al. Click the image above for a larger view.
One common theme that I have taken away from this framework and my own experience is the importance of direct communication. Taking the time to clarify the concerns of the primary team upfront, and then communicating recommendations in person or by phone (not just through the chart) can make a huge difference.
Reflecting on the instances when I felt most useful as a consultant, the tenet "be specific" rings true. Specific recommendations have been associated with improved implementation and they force us, as consultants, to explore more nuanced questions.
Consulting as a FIT is hard, but we learn an incredible amount about cardiology from the questions that come up. Having a framework for understanding the cognitive load can help to navigate the challenges of the role. In addition, being intentional about the mechanics of consulting has an important impact on the effectiveness of our recommendations and learning for everyone involved.

This article was authored by Paul Marano, MD, a fellow at Cedars-Sinai Medical Center. Twitter: @pjmarano1
This content was developed independently from the content developed for ACC.org. This content was not reviewed by the American College of Cardiology (ACC) for medical accuracy and the content is provided on an "as is" basis. Inclusion on ACC.org does not constitute a guarantee or endorsement by the ACC and ACC makes no warranty that the content is accurate, complete or error-free. The content is not a substitute for personalized medical advice and is not intended to be used as the sole basis for making individualized medical or health-related decisions. Statements or opinions expressed in this content reflect the views of the authors and do not reflect the official policy of ACC.