Quality Improvement and Patient Safety For FITs Part 1

The Accreditation Council for Graduate Medical Education requires that cardiology fellows take part in quality improvement (QI) projects or patient safety (PS) investigations.1 The interpretation of this requirement varies across institutions, from required quality improvement projects to simulated exercises. When I was applying to cardiology fellowship, I searched for a program that valued quality and safety as an integral part of the cardiovascular medicine experience. Three years later, I am now leading a QI and PS didactic fellowship curriculum, serving as a mentor for fellow-led QI projects, and working toward a Master of Health Policy Research with a focus on Quality and Safety.2 My goal is to convey why QI and PS should be a formal part of cardiovascular education and to provide some tools to carve out a quality and safety curriculum at your institution.
We are fixers.
As cardiologists, we love to find a fix. Whether it's performing a complex percutaneous intervention for refractory angina or tinkering with outpatient diuretic management for chronic heart failure, we gain satisfaction by knowing our treatments lead to improvement. The same is true for practice-based process improvement.
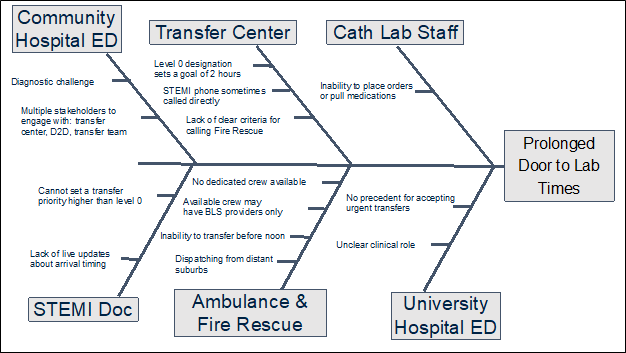 Figure 1. Fishbone Diagram from Quality and Safety Grand Rounds. It displays root causes for a prolonged door-to-lab time for patients with STEMI presenting at a community hospital.
Figure 1. Fishbone Diagram from Quality and Safety Grand Rounds. It displays root causes for a prolonged door-to-lab time for patients with STEMI presenting at a community hospital.
Take, for example, a pain point observed by my co-fellows last year. Our institution had recently acquired a community hospital in an under-resourced area of our city, and patients needing catheterization required transfer to the University hospital. Fellows and staff lamented that the transfer process was arduous, and some patients presenting with STEMI were not meeting door-to-balloon time quality metrics.3 Using QI methodology, the fellows took it upon themselves to investigate the problem (Figure 1). They presented their findings during Grand Rounds, and we now have an ambulance dedicated to urgent transfers from the community hospital. This is one of many examples of how a fellow's pain point has led to tangible improvement at our institution (Table 1).
In a "high reliability organization," promoting QI and PS generates a culture of safety.
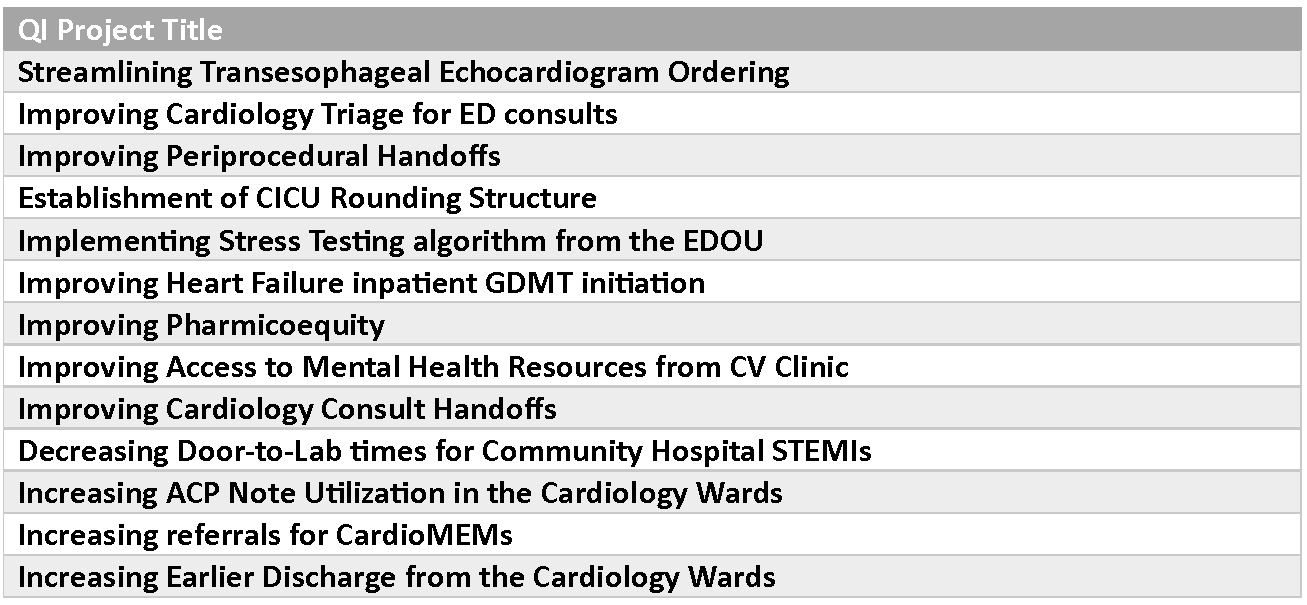 Table 1. Representative Sample of Fellow-Led QI projects from 2014-2023.
Table 1. Representative Sample of Fellow-Led QI projects from 2014-2023.
We all operate within "high reliability organizations," which are "organizations that consistently minimize adverse events despite carrying out intrinsically complex and hazardous work."4 A key component of these organizations is working toward a culture of safety. In medicine, this requires us to break through traditional hierarchies to establish a blame-free environment, where everyone is encouraged to report and openly discuss adverse events or near misses.
With a culture of safety in mind, our cardiology fellowship rebranded our Morbidity and Mortality Conferences to "Quality and Safety Grand Rounds." Using QI and PS tools, fellows present any system-based practice issues, not only adverse events. Over time, these Grand Rounds have shifted away from academic discussions about where things went wrong (though still important!), toward introspective conversations about how we as a division can improve (Figure 2).
 Figure 2. Cardiology fellows presenting their Fishbone Diagram at Quality and Safety Grand Rounds
Figure 2. Cardiology fellows presenting their Fishbone Diagram at Quality and Safety Grand Rounds
I believe a culture of safety starts from the top down. Through adopting the Quality and Safety Grand Rounds, our division leadership demonstrated that they value the fellows' voice. With the entire division as our audience, we use the platform to advocate for issues we care about and to directly involve stakeholders in actionable solutions. As empowered actors of change, fellows can then propagate safety culture as clinical team leaders, consultants and educators.
Formal QI and PS experience prepares us to be leaders in cardiovascular medicine.
The field of cardiology faces two large chasms: the clinical implementation gap between research output and real-world practice, and the clinical outcomes gap based on patient socioeconomic characteristics. The future of our field will count on current Fellows in Training (FITs) to work on closing these gaps, pushing forward care for the growing population of cardiovascular patients. QI initiatives, with a focus on implementing change in real-time, take a central role in understanding and narrowing these chasms. Familiarizing ourselves with these tools early and often in cardiovascular training prepares us to lead the charge.
My hope is that I sparked your interest in quality and safety education and convinced you that it is an integral component to our careers as cardiologists.
The ACC Quality Summit, a live-format conference, provides a platform for you to present your abstract, connect with health care quality experts, share insights and engage in discussion with peers and mentors on advancing quality care in cardiology. Abstract submissions are currently open. Learn more about submitting an abstract for Quality Summit here.
References:
- ACGME Program Requirements for Graduate Medical Education in Cardiovascular Disease. Accreditation Council for Graduate Medical Education. Available at: https://www.acgme.org/globalassets/pfassets/reviewandcomment/rc/141_cardiovasculardisease_rc_012023.pdf
- Penn Master of Science in Health Policy Research. Penn Medicine. Available at: https://mshp.med.upenn.edu/concentration-healthcare-quality-and-safety
- Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction- Executive Summary. Am Heart J. 2004;110:588-636. Doi: doi.org/10.1161/01.CIR.0000134791.68010.FA
- Culture of Safety. Patient Safety Network. Available at: https://psnet.ahrq.gov/primer/culture-safety

This article was authored by Jadry Gruen, MD, a chief cardiology fellow at the University of Pennsylvania in Philadelphia, PA, and a master’s candidate in Health Policy Research with a Concentration in Quality and Safety.
This content was developed independently from the content developed for ACC.org. This content was not reviewed by the American College of Cardiology (ACC) for medical accuracy and the content is provided on an "as is" basis. Inclusion on ACC.org does not constitute a guarantee or endorsement by the ACC and ACC makes no warranty that the content is accurate, complete or error-free. The content is not a substitute for personalized medical advice and is not intended to be used as the sole basis for making individualized medical or health-related decisions. Statements or opinions expressed in this content reflect the views of the authors and do not reflect the official policy of ACC.

