Peripheral Matters | Building Competencies to Optimize Care For Chronic Limb-Threatening Ischemia

Chronic limb-threatening ischemia (CLTI) is the end stage form of peripheral artery disease (PAD) characterized by pain on rest or tissue loss. CLTI affects roughly 2 million individuals in the U.S., and results in high rates of cardiovascular morbidity, mortality and amputation.1,2
Despite these realities, CLTI care continues to be suboptimal on many fronts. Medical therapy is underutilized, amputations are performed prior to proper vascular evaluations, and ongoing disparities in care delivery disproportionately affect certain disadvantaged patient groups, according to multiple studies of CLTI.3-5
Compounding the situation further, many components of CLTI care are delivered by clinicians across a variety of disciplines. For example, endovascular revascularization is performed by interventional radiologists, vascular surgeons, interventional cardiologists and others. The training backgrounds and clinical experiences of these specialists undoubtedly differ, which may foster inconsistent application of guideline-based therapies and variation in the revascularization skill sets that are required to prevent amputation in patients with CLTI. Indeed, many of the endovascular techniques required in CLTI are advanced relative to those for claudication, and many skills beyond revascularization are needed to achieve optimal patient outcomes.
Ensuring that endovascular specialists possess the cognitive, clinical and procedural skill sets germane to CLTI is a necessary step to improve the care of this patient population more broadly. A new multispecialty training statement for endovascular specialists engaged in CLTI care defines the requisite competencies needed to provide evidence-based and multidisciplinary care to the CLTI population. This framework allows training programs to construct curricula to facilitate competency acquisition, enable interested professional societies to create products to fill education needs, and enhance collaboration among specialties with interest in enhancing CLTI care more broadly.
The multispecialty effort was led by the Society for Cardiovascular Angiography and Interventions, and included the American College of Radiology, American Podiatric Medical Association, Society for Interventional Radiology, Society for Vascular Medicine, Society for Vascular Surgery, Society for Clinical Vascular Surgery and Vascular and Endovascular Surgical Society. The Position Statement on Competencies for Endovascular Specialists Providing CLTI Care was co-published in JSCAI and other journals.
Competencies For Endovascular Specialists
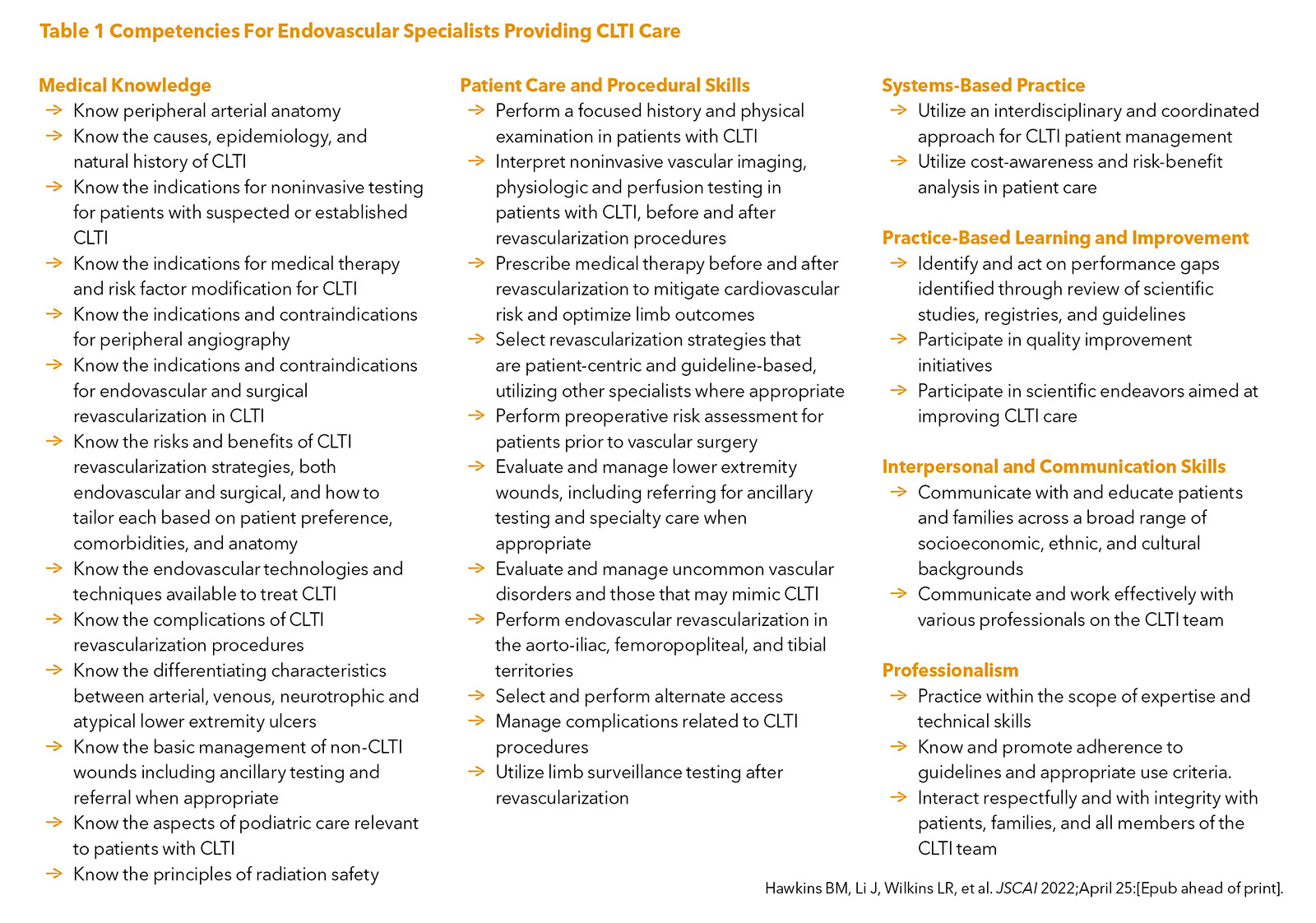
The training statement provides a set of competencies for endovascular specialists treating CLTI using the framework developed by the Accreditation Council for Graduate Medical Education with six core competencies: medical knowledge, patient care and procedural skills, systems-based practice, problem-based learning and improvement, professionalism, and interpersonal and communication skills (Table 1).
These competencies range from the prescription of medical therapy, wound assessment, selecting revascularization strategies based on anatomy and patient characteristics, and the performance of complex endovascular procedures.
Importantly, the document emphasizes the need for a multidisciplinary approach to CLTI management, and that best care is often delivered within the context of a CLTI team with specialists able to provide both surgical and endovascular revascularization. Indeed, surgical revascularization remains an important therapeutic modality for many CLTI patients.
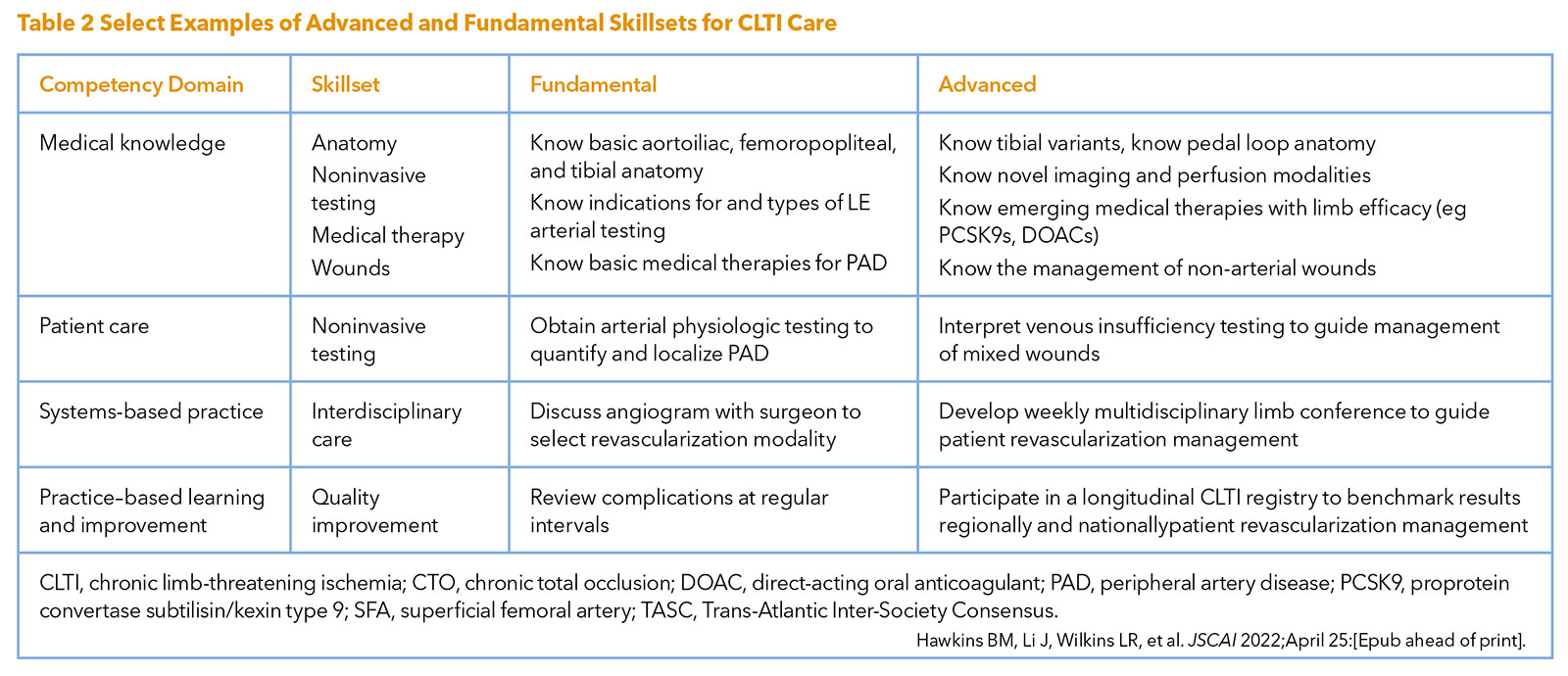
Notably, many competencies were stratified into fundamental and advanced categories to account for the range of complexity in delivering care (Table 2) and recognizing that many CLTI specialists will gain additional skill sets after completing training and as the field of CLTI care evolves. It was recognized that many skill sets may not be easily obtained within a single training environment or experience, and that some competencies exist within a spectrum ranging from simple to very complex tasks. As an example, in the case of below knee revascularization, angioplasty of a focal, proximal tibial lesion is relatively straightforward, whereas performing atherectomy, angioplasty, and tacking of a lengthy tibial chronic total occlusion is more complex.
Learn More About PAD
Get up to speed on the latest evidence-based strategies with ACC's free online education course Peripheral Artery Disease: Optimizing Treatment Strategies. Visit ACC.org/LearnPAD for self-paced learning with certified education, patient cases, quick tips, videos and interactives lessons.
Click here to learn more about the disparities in the prevalence, management and outcomes in PAD from a recent Peripheral Matters article in Cardiology.
The institutional characteristics important in allowing endovascular specialists to gain the needed competencies are also outlined. For example, sophisticated noninvasive vascular testing is critical, and includes both physiologic and perfusion testing, as well as imaging. Access to other components of the CLTI team (e.g., wound care, podiatry) and working in an environment with a framework to assess quality aspects of CLTI care are ideal. Procedural areas must have equipment to perform multilevel and distal revascularization, and should be equipped with devices to perform alternate access and treat the complex lesions frequently encountered in patients with CLTI.
In summary, this multispecialty initiative to define CLTI competencies serves as a starting point by which endovascular training can be standardized across specialties. It is hoped this effort will enhance training program curricula, foster collaboration across specialties, and thereafter improve the care received by individuals with CLTI.

This article was authored by Beau M. Hawkins, MD, FACC, (@BeauHawkinsMD) and Razan Elsayed, MD, at the Cardiovascular Section, University of Oklahoma Health Sciences Center, Oklahoma City, OK.
References
- Abu Dabrh AM, Steffen MW, Undavalli C, et al. The natural history of untreated severe or critical limb ischemia. J Vasc Surg 2015;62:1642-51 e3.
- Duff S, Mafilios MS, Bhounsule P, Hasegawa JT. The burden of critical limb ischemia: a review of recent literature. Vasc Health Risk Manag 2019;15:187-208.
- Armstrong EJ, Chen DC, Westin GG, et al. Adherence to guideline-recommended therapy is associated with decreased major adverse cardiovascular events and major adverse limb events among patients with peripheral arterial disease. J Am Heart Assoc 2014;3:e000697.
- Lefebvre KM, Chevan J. The persistence of gender and racial disparities in vascular lower extremity amputation: an examination of HCUP-NIS data (2002-2011). Vasc Med 2015;20:51-9.
- Reinecke H, Unrath M, Freisinger E, et al. Peripheral arterial disease and critical limb ischaemia: still poor outcomes and lack of guideline adherence. Eur Heart J 2015;36:932-8.
- Creager MA, Gornik HL, Gray BH, et al. COCATS 4 Task Force 9: Training in Vascular Medicine. J Am Coll Cardiol 2015;65:1832-43.
- King SB 3rd, Babb JD, Bates ER, et al. COCATS 4 Task Force 10: Training in Cardiac Catheterization. J Am Coll Cardiol 2015;65:1844-53.
Clinical Topics: Cardiac Surgery, Cardiovascular Care Team, Invasive Cardiovascular Angiography and Intervention, Vascular Medicine, Atherosclerotic Disease (CAD/PAD), Aortic Surgery, Interventions and Imaging, Interventions and Vascular Medicine, Angiography, Nuclear Imaging
Keywords: ACC Publications, Cardiology Magazine, Accreditation, Amputation, Angiography, Angioplasty, Atherectomy, Cardiologists, Cardiology, Cardiovascular Diseases, Cognition, Communication, Contraindications, Culture, Education, Distance, Education, Medical, Graduate, Endovascular Procedures, Heart Disease Risk Factors, Lower Extremity, Oklahoma, Patient Care, Patient Preference, Patient-Centered Care, Perfusion, Peripheral Arterial Disease, Physical Examination, Podiatry, Prescriptions, Problem-Based Learning, Professionalism, Quality Improvement, Radiologists, Radiology, Interventional, Referral and Consultation, Registries, Risk Assessment, Risk Factors, Socioeconomic Factors, Support Vector Machine, Surgeons, Ulcer
< Back to Listings