Innovative Endovascular Therapies For Iliofemoral Disease

Successful cardiac catheterization begins with safe vascular access and ends with effective hemostasis after equipment removal. Approximately 8 million Americans are affected by peripheral arterial disease (PAD).1 The prevalence of PAD in patients >70 years is as high as 29%.2 The risk of PAD increases with more comorbidities and risk factors, including tobacco smoking, chronic kidney disease, diabetes, hypercholesterolemia and Black race.
Operators who perform interventions for complex coronaries and structural heart disease are often challenged with complex PAD that precludes insertion of a large-bore vascular sheath unless preemptive intervention is planned. Large-bore femoral vascular artery access is feasible, safe and associated with low complication rates if a strict protocol is planned and implemented before the procedure.
Bleeding and vascular complications continue to be a substantial source of morbidity, especially in patients undergoing large-bore access procedures.3-5 In an attempt to overcome the challenges of PAD interventions, especially in the iliofemoral space, alternative access and new technology have helped operators treat patients with occlusive disease and severe symptomatic PAD or those who require large-bore vascular access for TAVR or mechanical circulatory support (MCS).
Innovation in the vascular access space is ongoing to optimize procedural success, reduce complications, and improve outcomes and patient satisfaction. This has led to more frequent referral of elderly patients with multiple comorbidities for high-risk structural and endovascular interventions that often require MCS, oftentimes using large-bore arterial access.6,7 I'll review here two cases that illustrate the benefit of these innovations.
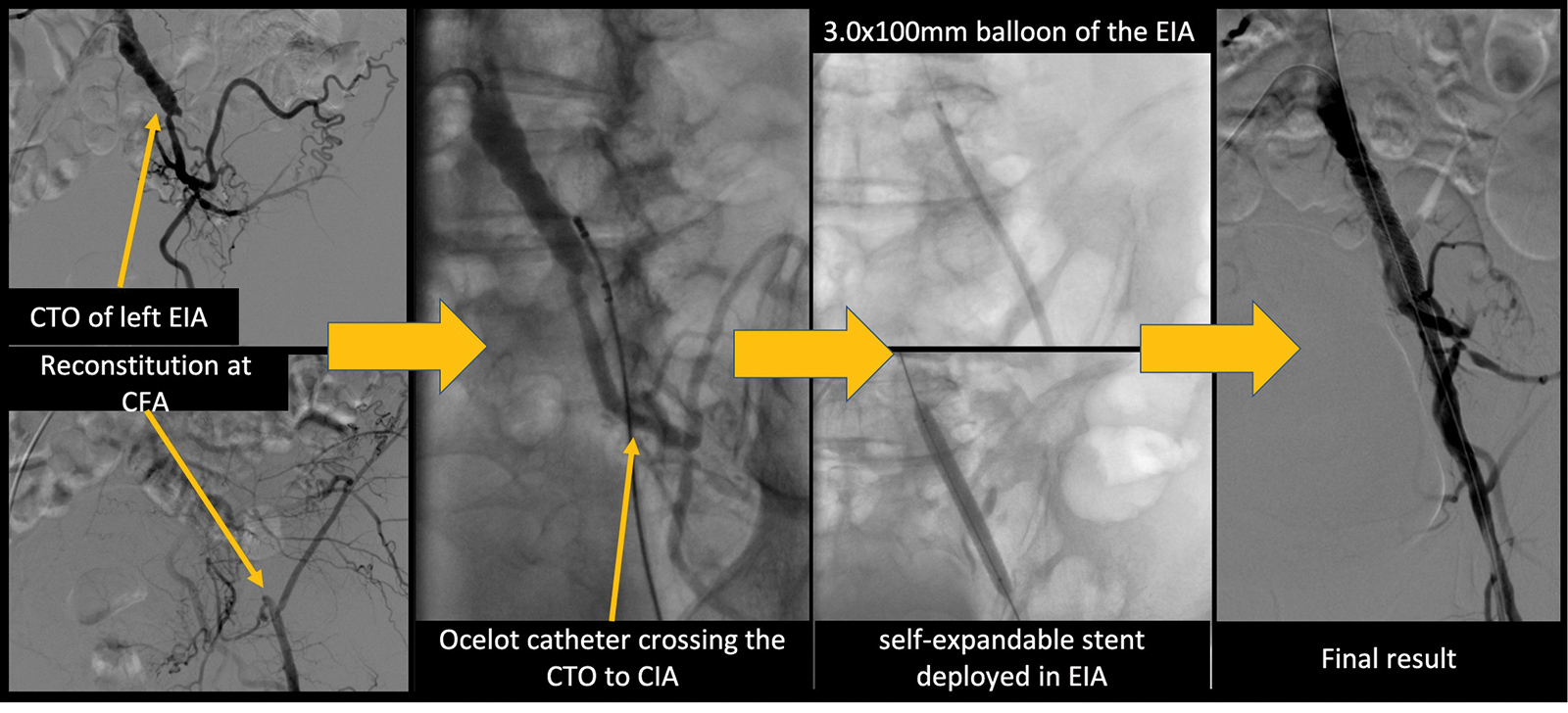
My first case highlights the convenience of advanced technology to provide endovascular therapy for complete total occlusions of the iliac arteries. A 61-year-old man presented with lifestyle-limiting claudication and an ankle-brachial index of 0.61 in the left leg. He had a history of smoking, diabetes, hypertension and coronary artery disease. Despite maximal medical therapy and exercise therapy he continued to have pain with short distances. A peripheral angiogram revealed complete total occlusion (CTO) of the left external iliac artery (EIA) and reconstitution at the common femoral artery (CFA).
Therefore, using the left CFA, a 6 French sheath was inserted using US guidance and micropuncture technique. Using the Avinger Ocelot catheter to the EIA, the CTO was crossed successfully from the CFA to the left common iliac artery (CIA). The lesion then was ballooned with a 3.0 x 100 mm balloon and stented with 8.0 x 59 mm and 8.0 x 60 mm balloon-expanding stents. The final angiogram showed complete resolution of the stenosis with reduction of stenosis from 100% to 0%. At his clinic visit a few weeks later, he reported resolution of his claudication.
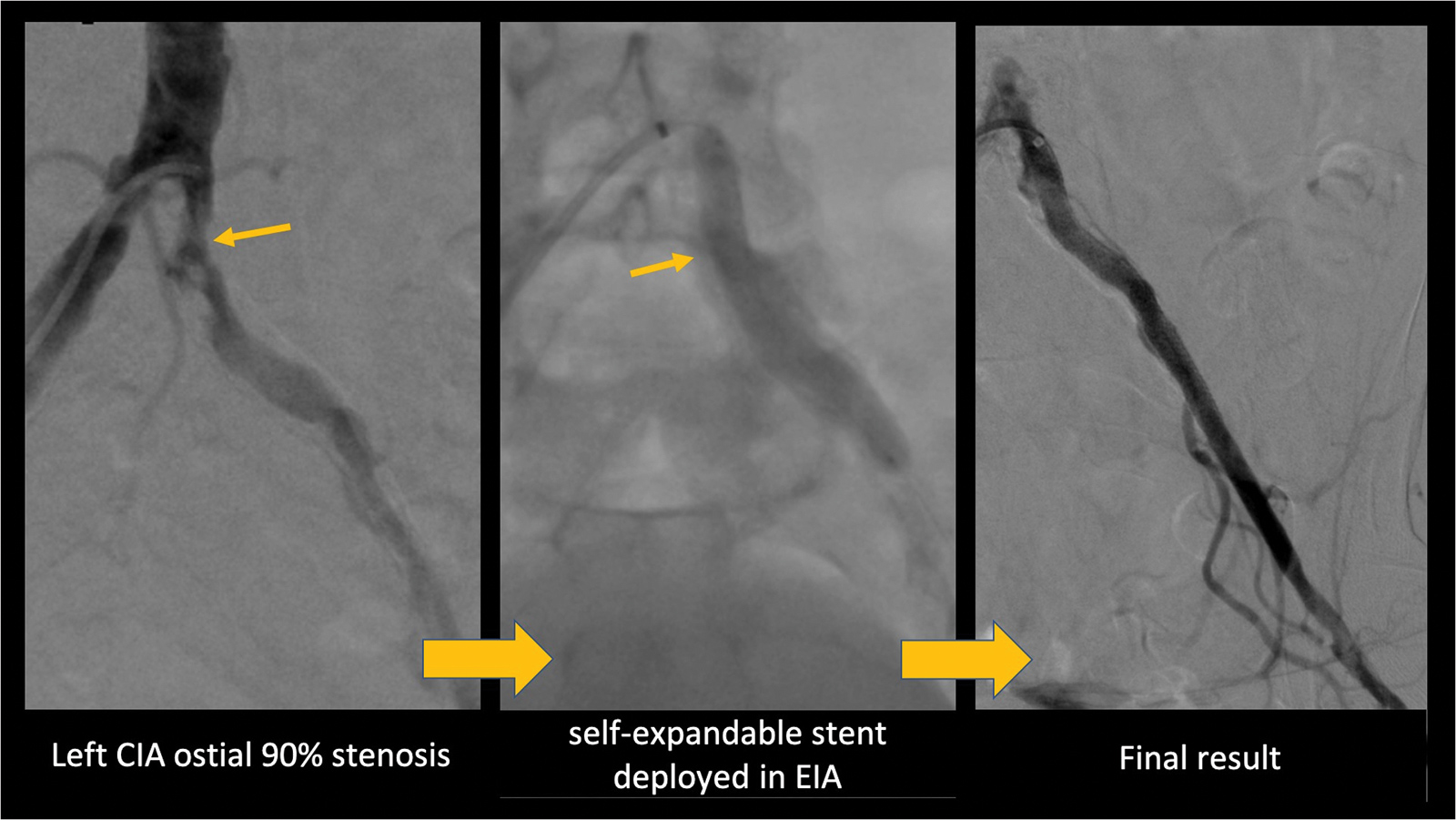
The second case highlights the possibility to "stay femoral" for a large-bore sheath for a structural heart intervention and to avoid alternative access using new technology. A 79-year-old woman presented with shortness of breath lasting several months, chest pain and resting pain in both legs. Severe aortic valve stenosis was revealed on workup and she was referred for TAVR. However, because of severe bilateral iliac disease she was referred to the cath lab for a peripheral angiogram and intervention in preparation for the TAVR procedure. The angiogram showed severe right EIA and left ostial CIA stenosis and right external artery disease. Using the right CFA, a 6 French sheath was inserted using US guidance and micropuncture technique.
The left CIA was crossed using a 0.014 Runthrough wire that was advanced distally into the left superficial femoral artery. A 0.014 microcatheter was advanced over the Runthrough wire and exchanged for a Viper wire. A 2.0 mm Diamondback 360 Peripheral Orbital Atherectomy System was advanced over the Viper wire and atherectomy was performed.
A Shockwave intravascular lithotripsy 6.0 x 60 mm balloon was advanced over the Viper wire and the balloon was inflated to 4 atmospheres and 30 pulse therapies were delivered twice to the ostial left CIA. After lithotripsy was delivered, the balloon was inflated to 6 atmospheres for three minutes. Then two balloon-expandable stents were deployed (7.0 x 59 mm and 7.0 x 19 mm) with reduction of stenosis from 90% to 0%.
PAD revascularization should be reserved for a select group of patients with critical limb ischemia or lifestyle-limiting claudication. Emerging endovascular approaches reduce vascular complications and bring new options for these patients.
References
- Hirsch AT, Criqui MH, Treat-Jacobson D, et al. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001;286:1317-24.
- Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999-2000. Circulation 2004;110:738-43.
- Webb JG, Chandavimol M, Thompson CR, et al. Percutaneous aortic valve implantation retrograde from the femoral artery. Circulation 2006;113:842-50.
- Howell M, Villareal R, Krajcer Z. Percutaneous access and closure of femoral artery access sites associated with endoluminal repair of abdominal aortic aneurysms. J Endovasc Ther 2001;8:68-74.
- Redfors B, Watson BM, McAndrew T, et al. Mortality, length of stay, and cost implications of procedural bleeding after percutaneous interventions using large-bore catheters. JAMA Card. 2017;2:798-802.
- O'Neill WW, Kleiman NS, Moses J, et al. A Prospective randomized clinical trial of hemodynamic support with Impella 2.5 TM versus intra-aortic balloon pump in patients undergoing high-risk percutaneous coronary intervention: the PROTECT II Study. Circulation 2012;126:1717-27.
- Werdan K, Gielen S, Ebelt H, Hochman JS. Mechanical circulatory support in cardiogenic shock. Eur Heart J 2014;35:156-67.
Clinical Topics: Cardiac Surgery, Dyslipidemia, Invasive Cardiovascular Angiography and Intervention, Atherosclerotic Disease (CAD/PAD), Aortic Surgery, Homozygous Familial Hypercholesterolemia, Interventions and Coronary Artery Disease, Interventions and Vascular Medicine
Keywords: ACC Publications, Cardiology Magazine, Femoral Artery, Iliac Artery, Peripheral Arterial Disease, Coronary Artery Disease, Ankle Brachial Index, Tobacco, Risk Factors, Constriction, Pathologic, Prevalence, Hypercholesterolemia, Patient Satisfaction, Transcatheter Aortic Valve Replacement, Atherectomy, Intermittent Claudication, Cardiac Catheterization, Endovascular Procedures
< Back to Listings