Feature | Structural Heart Disease Intervention: Quo Vadis
Interventional therapies for cardiac pathology have advanced at a rapid and accelerating rate during the last decade and are now legion. During the latter half of the last century there was a rapid expansion of surgical solutions which more recently have been standardized, promoting reliable and durable results. This is now the era of safe and reproducible surgery.
The advent of minimal access and percutaneous procedures have altered the landscape irreversibly, often, but not always for the good. The trend towards the apparent universal dissemination of coronary angioplasty and stenting applied in a staged approach has been replaced by the demonstration of the superiority of surgery in certain defined groups; this, plus the advent of the "heart team" operating within the confines of a good evidence base has resulted in a balanced approach with a more appropriate use of surgery and catheter-based procedures to the betterment of patient outcomes.
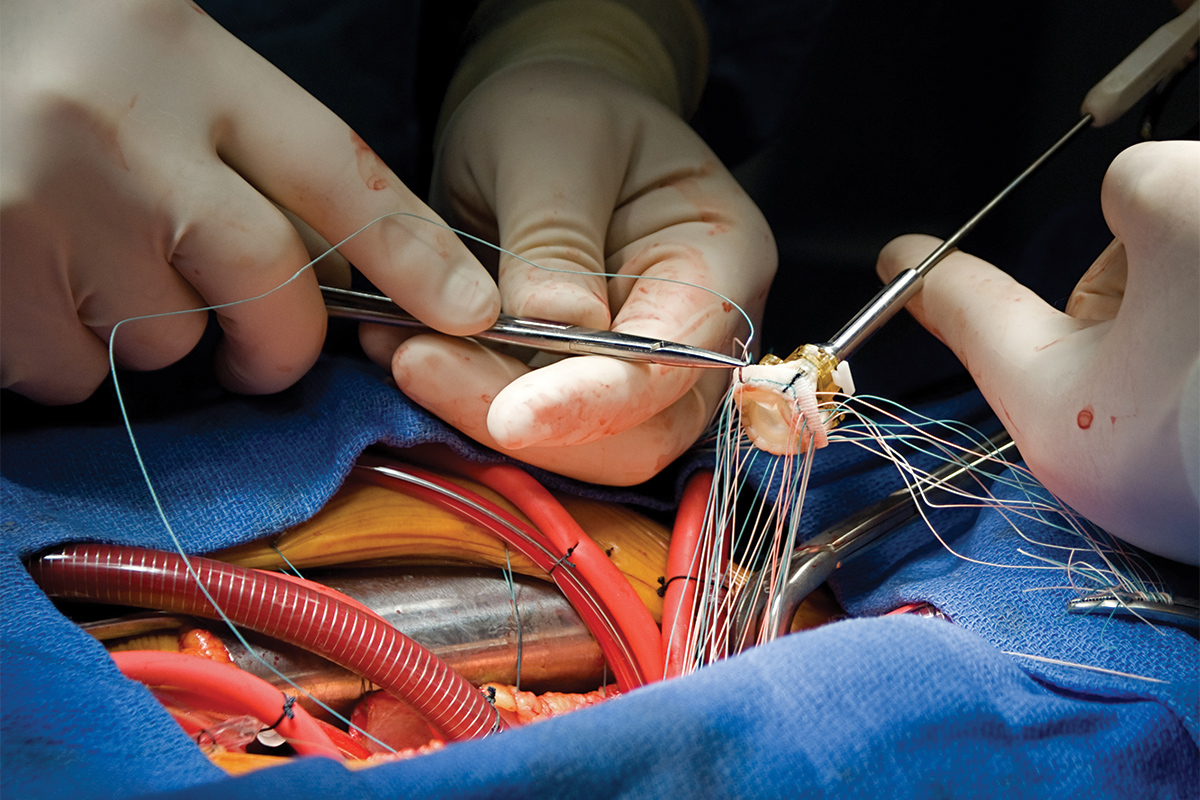
A new revolution is happening now in the management of heart valve disease. Effective therapies for the mitral and aortic valves are evolving quickly and whilst short-term outcome data are being generated and published, some in the form of randomized-controlled trials, meaningful mid- to long-term data (five to 15 years) is absent. Conversely, while the vast surgical experience is short on controlled prospective data, it is replete with long-term of the performance of most important extant valve types.
Data at 15 and 20+ years are available for valve replacement and valve reconstruction. A great deal is known about prosthetic valve function and deterioration, the incidence of significant para-prosthetic leaks and patient-prosthesis mismatch. Current mortality should be very low with rates of less than 1% mortality and six days or less length of hospital postoperative stay being almost the rule in good centers, and excellent and durable quality of life is now the norm. However, all is not perfect.

Remember, the elephant in the room is there is no such thing as "surgery," there are only "surgeons" and their results are variable. Hence the need for specialist centers.
Variable results between surgeons and centers continue and poor surgery results in the complications raised above. A recent paper reported a mortality of 3.6% for SAVR in a study which contrasted this with the results for TAVR, portraying SAVR in a poor light.1 However, the quoted incidence of mortality is at a level that would cause horror in quality institutions. (Current mortality for all-comers for AVR in our hospital runs at 0.8% and we believe this can be improved upon).
Hospital length of stay is an average of five days and para-prosthetic leaks and early valve failure are rare. Contrast this with TAVR where mortality is also low, but para-prosthetic leaks and pacemaker use are high and mid- to long-term failure rate remains largely unknown.
In the mitral arena, reconstructive surgery of the "degenerative" valve is now the norm in most expert centers where expertise is focused in fewer, expert hands. Repair rates exceeding 90% are expected with a mortality of less than 1%.1 Mitral valve replacement with complete subvalve preservation is similarly an excellent procedure with well-defined and excellent long-term outcomes.
Into this arena steps percutaneous interventions that are as yet not well tested outside a few specialist centers. The Mitraclip, where the opposing leaflets are fixed together producing a double-orifice valve, has now secured approval in some countries and institutions.
Its initial use has been in patients otherwise deemed too high risk for surgery and patients with functional mitral regurgitation resulting in satisfactory initial results in controlling and/or reducing the amount of mitral regurgitation.
However, several learning points from the surgical groups are being ignored. One is that ischemic mitral regurgitation is a ventricular disease which will progress as ventricular degeneration continues causing a return of mitral regurgitation.

With a surgical approach, multiple procedures exist to mitigate against this including annuloplasty, papillary muscle approximation and ventricular wall plication. Indeed, the most recent studies have shown superiority of mitral valve replacement with subvalvular preservation in the worst cases.
Its move into degenerative cases is being enhanced by poorly controlled mitral valve surgery in some centers where repair in even infirm elderly patients can be achieved with excellent permanent results in the correct surgical hands.
It can be argued that all of this reveals a focus on the careers of some professionals rather than what is best for patients. One has to ask how much professional empowerment and perhaps arrogance plays over the Hippocratic stance of first do no harm on both sides of this particular fence.
Thus, what should be the way ahead? First, the use of such devices is discussed by a well-informed heart team. Second, ready access to the evidence base. Third, the prospective collection of all data. With this in place, the best plan for each patient can be formed.
Finally, it is vital that the patient is given a full review of the discussion surrounding their case, not "edited highlights" to enable them to make the best decision for themselves.
And, cardiologists, do not forget that the more routine surgery keeps surgeons in practice for the more difficult problems whence many patients will still need their skills.
Editor's Note: Click here for an editorial on patient selection for TAVR and here for recommendations for TAVR and more from the newly released ACC/AHA Guideline on Valvular Heart Disease.
Reference
- Braunberger E, Deloche A, Berrebi A, et al. Circulation 2001;104:I8–I11.
Clinical Topics: Cardiac Surgery, Invasive Cardiovascular Angiography and Intervention, Valvular Heart Disease, Aortic Surgery, Cardiac Surgery and VHD, Interventions and Structural Heart Disease, Mitral Regurgitation
Keywords: ACC Publications, Cardiology Magazine, Aortic Valve, Quality of Life, Mitral Valve, Mitral Valve Insufficiency, Papillary Muscles, Incidence, Length of Stay, Transcatheter Aortic Valve Replacement, Prospective Studies, Heart Valve Prosthesis, Heart Valve Diseases, Tricuspid Valve, Pacemaker, Artificial, Catheters, Surgeons, Hospitals, Reconstructive Surgical Procedures, Angioplasty
< Back to Listings