Feature | Familial Hypercholesterolemia: Illuminating Current Practice Patterns

One in 250 people of all races and ethnicities have familial hypercholesterolemia (FH), one of the most common genetic diseases that if left untreated increases the risk of early coronary artery disease (CAD) by 20-fold. In fact, a myocardial infarction (MI) will occur in 30% of women with untreated FH by the age of 60 years and in 50% of men with untreated FH by the age of 50.
While heterozygous FH (HeFH) is the most common form of HF, approximately one in 250,000 persons has homozygous FH (HoFH). These patients typically have very high levels of LDL-C (>400 mg/dL) and even in their adolescence can have evidence of CAD and aortic stenosis. Without aggressive treatment, including medications specific to HoFH and LDL-C apheresis, early mortality before the age of 30 is common among HoFH patients.
Notably, early diagnosis and treatment of FH has been shown to reduce the risk of CAD by 80%. Thus, it remains concerning that FH is diagnosed in only about 10% of individuals who have it.
A recent ACC survey of 153 practicing clinicians in the U.S. suggests limited training for clinicians and gaps in patient understanding of the disease are among the reasons for the low diagnosis rates.
Current Practice Landscape
1
in
250
people of all races and ethnicities have familial hypercholesterolemia, one of the most common genetic diseases, that left untreated increases the risk of early coronary artery disease by
20-fold
One-third of survey respondents said they are seeing patients with treated LDL-C >300 mg/dL and only 17% have patients with untreated LDL-C >400 mg/dL. Of note, more than half (54%) are not treating patients in either category. Of the respondents, 15% indicate they are treating a family with a parent having LDL-C >400 mg/dL plus all offspring having LDL-C levels of 160-400 mg/dL.
More cardiologists who have diagnosed patients with HoFH before, compared with those who have not, are seeing patients with treated LDL-C >300 mg/dL (46% vs. 29%).
HoFH was the most common diagnosis by 67% of clinicians for a patient presenting with an untreated LDL-C >400 mg/dL, compared with HeFH at 21%. However, nearly a quarter of clinicians were unsure of their diagnosis.
Diagnosing HoFH in the past influenced the diagnosis they'd make now for a patient with an untreated LDL-C >400 mg/dL. Among the third of cardiologists who reported previously diagnosing HoFH, most would diagnose such patients with HoFH compared with HeFH (78% vs. 25%). For cardiologists who have not previously diagnosed HoFH, the diagnosis would be HoFH by 64% and HeFH by 19%, and 20% were unsure.
In terms of managing patients with untreated LDL-C >400 mg/dL, medication and reviewing family history were the top priorities for the majority of clinicians at 68% and 54%, respectively. These priorities were followed by referral to a specialist by less than a third (29%) and encouraging lifestyle changes and repeating the lipid panel in six months by 17%. Nearly one-third were unable to rank the level of lifestyle changes and a repeat lipid panel.
Making the Diagnosis: Family Influence?
Screening and/or testing of children with a family history of cardiovascular disease is the biggest challenge for cardiologists in diagnosing HoFH in children and adults, according to the survey.
Less than half of respondents indicate they would diagnose HoFH (44%) or HeFH (32%) in a patient with a parent who had LDL-C >400 mg/dL and offspring with LDL-C of 160-400 mg/dL. An additional 18% say they are unsure of their diagnosis.
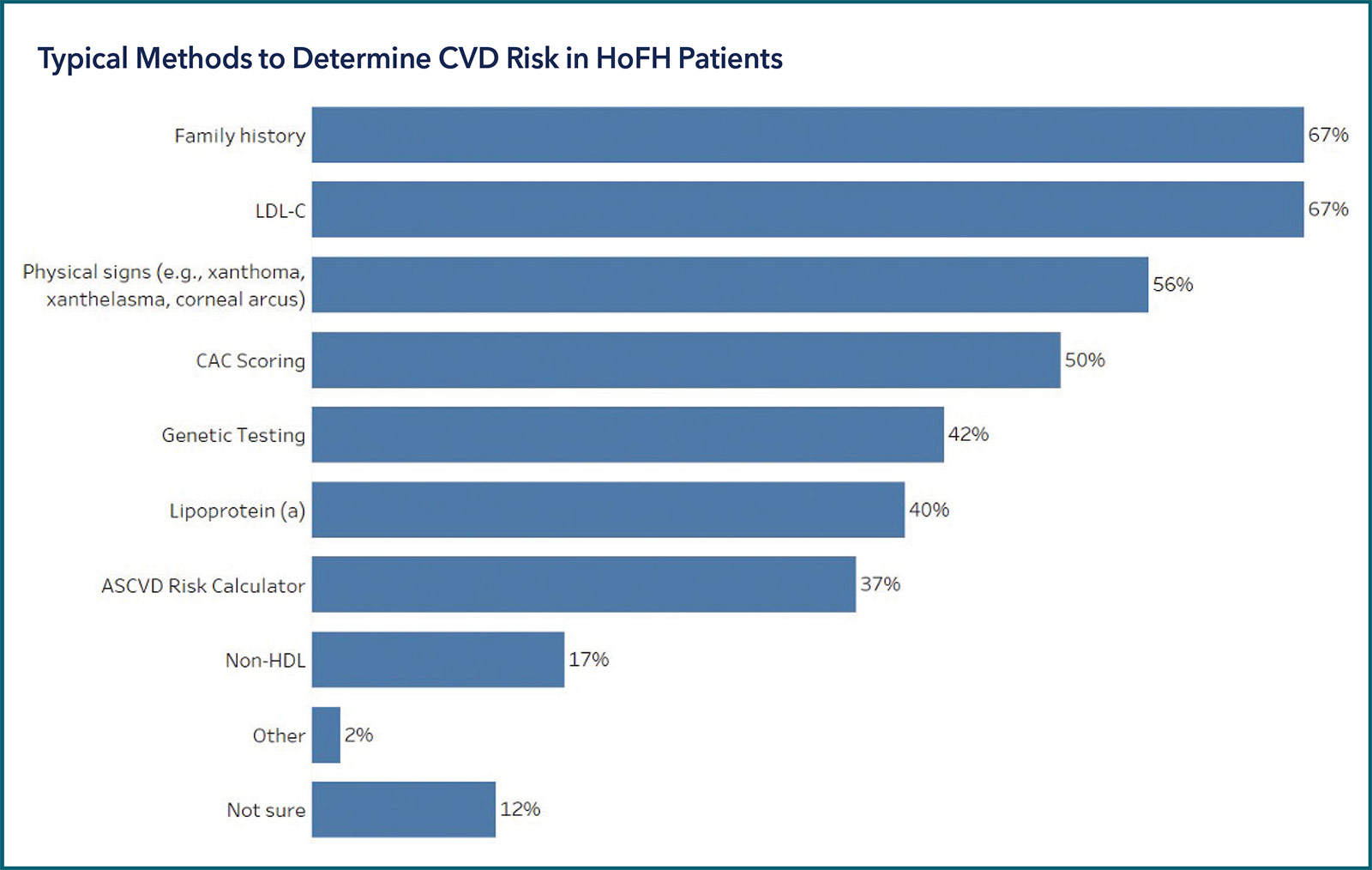
Determining the risk of cardiovascular disease in HoFH patients would be based on family history and LDL-C level for two-thirds of the cardiologists. About a half would rely on physical signs or coronary artery calcium (CAC) scoring (50%). More of the cardiologists with past experience diagnosing HoFH relied on LDL-C to determine risk, compared with their colleagues who had not (81% vs. 60%), and they were more likely to use CAC scoring (65% vs. 44%). Nearly one-fifth (18%) of those without past experience were unsure of the methods to use to determine cardiovascular disease risk in HoFH patients.
Cascade screening lipid level testing should be done for first-degree relatives more than 75% of the time, believe the majority (68%) of respondents, and 59% believe it should almost always be used. This is more likely to be the case for general cardiologists/pediatric cardiologists (77%) and those who have previously diagnosed HoFH (78%).
Patient Challenges Affect Diagnosis
The primary challenge for patients with HoFH is the lack of awareness of the condition and the risk among offspring, say 65% of respondents. This is followed by patient's not understanding their disease and the familial link, and the importance of medication/treatment.
Interestingly, cardiologists who have diagnosed HoFH before are more likely to view the patient's understanding of their medication/treatment (73%) as a primary challenge much more so than their colleagues (48%).
Meanwhile, slightly more than a third of respondents say patient understanding of other risk factors such as obesity, diabetes, metabolic syndrome, etc., are the bigger challenge when it comes to managing FH diagnosis and treatment.
Treating HoFH: What Do They Think?
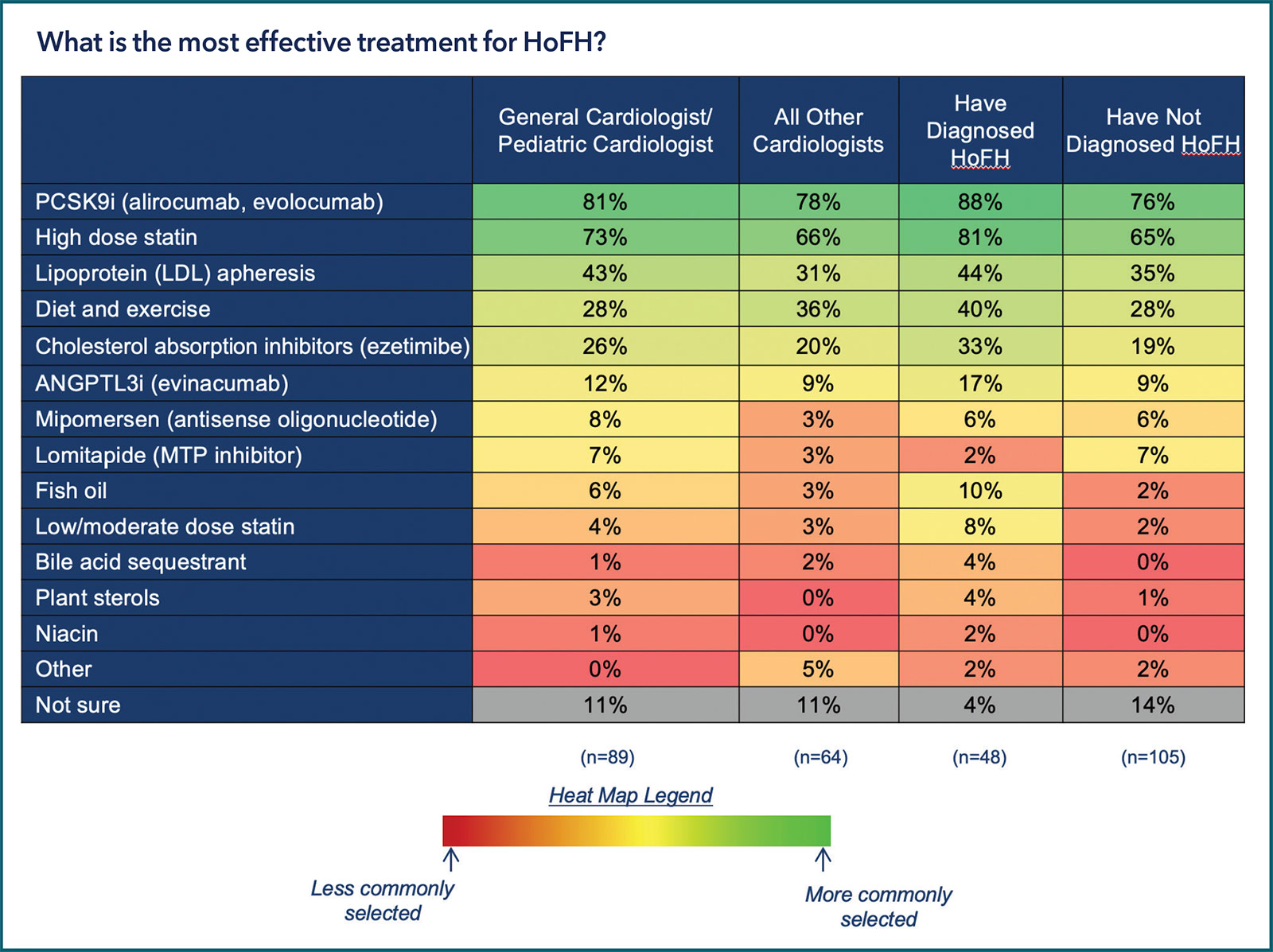
PCSK9 inhibitors (alirocumab, evolocumab) and high-dose statins were ranked as the two most effective treatments for HoFH (by 80% and 70%, respectively). This view was held across type of cardiologist and was slightly stronger among those who had previously diagnosed HoFH.
These were followed by LDL apheresis by 38%, diet and exercise by 31% and cholesterol absorption inhibitors (ezetimibe) by 24%. Only a minority selected an ANGPLT3 inhibitor (evinacumab), antisense oligonucleotide (mipomersen) or MTP inhibitor (lomitapide), ranging from 11% down to 5%.
Not surprisingly, the majority of respondents expressed greater familiarity with PCSK9 inhibitor therapy and less familiarity with ANGPLT3 inhibitors and MTP inhibitors.
Of the survey respondents, only 10% consider themselves a lipid specialist and only 2% are certified by the American Board of Clinical Lipidology or the Accreditation Council for Clinical Lipidology. But two-thirds say they have access to a lipid specialist and 38% have access to an apheresis center.
For the one-third of respondents who treat patients younger than 18, the lack of screening and/or testing of children with family history of cardiovascular disease is the biggest diagnostic challenge in this age group. Nearly half (47%) believe the biggest treatment challenge in patients under 18 is that the medications effective for adults are not approved for them. Additionally, more than one-fifth (22%) say the lipid specialist is too far away for treatment, and 20% of respondents believe ineffective/inadequate treatments for younger patients is the biggest challenge and 20% selected access to an apheresis treatment center. However, more than one-third (37%) were unable to respond.
Education: The Path Forward
In terms of patient education, respondents believe useful tools include a decision aid to help guide treatment selection, along with a topic page and an infographic on HoFH from CardioSmart.
"I suspect [FH] is underdiagnosed in my practice," says one respondent, adding that hopefully resources from ACC will improve identification and treatment.
Clinicians also reported that online education and e-learning on HoFH would be very helpful to their practice. One respondent shared there was little and "not great" training on HoHF during fellowship, with others echoing limited training and knowledge, and that an opportunity to learn through web-based or interactive tools would be welcomed. Specific topics for education include guidelines, the impact of genetics on families, importance of screening, testing and diagnosis, as well as new therapies in development. An interactive infographic focused on guidelines was selected by 73% as being very beneficial.
Clinical Topics: Cardiovascular Care Team, Congenital Heart Disease and Pediatric Cardiology, Diabetes and Cardiometabolic Disease, Dyslipidemia, Prevention, Valvular Heart Disease, Atherosclerotic Disease (CAD/PAD), CHD and Pediatrics and Prevention, CHD and Pediatrics and Quality Improvement, Lipid Metabolism, Nonstatins, Novel Agents, Statins, Diet
Keywords: ACC Publications, Cardiology Magazine, Adolescent, Middle Aged, Child, Preschool, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Cholesterol, LDL, PCSK9 protein, human, Proprotein Convertase 9, Calcium, Cardiologists, Data Visualization, Coronary Artery Disease, Cardiovascular Diseases, Centers for Medicare and Medicaid Services, U.S., Checklist, Computer-Assisted Instruction, Education, Distance, Fellowships and Scholarships, Metabolic Syndrome, Blood Component Removal, Early Diagnosis, Oligonucleotides, Antisense, Myocardial Infarction, Aortic Valve Stenosis, Genetic Testing, Accreditation, Decision Support Techniques, Risk Factors, Life Style, Life Style, Ezetimibe, Referral and Consultation, Internet, Diabetes Mellitus, Obesity, Parents, Diet
< Back to Listings