Cover Story | Environmental Stress and Cardiovascular Disease
Environmental stressors like air pollution and extreme temperatures have multiple deleterious effects on cardiovascular health, which have all but been ignored. Lately, in concert with the cry to attend to the current and upcoming calamities caused by climate change, are a chorus of cardiologists ensuring that the impacts on the heart are also considered.
"While we face the existential crisis of climate change, most people don't realize that of the many deleterious effects of of air pollution, cardiovascular disease is #1. It's not diseases of the lung or cancer, but it's in fact ischemic heart disease and stroke that top the list," says Jamal S. Rana, MD, PhD, FACC, chief of cardiology at Kaiser Permanente's Oakland Medical Center and governor of ACC's Northern California Chapter.
This month, Cardiology takes a look at the many environmental hits the heart takes from air pollution and extreme temperatures and what can, and should, be done to attenuate the effects of environmental stress on the heart. We focus primarily on air pollution, including wildfire smoke and extreme heat – two very, well, hot topics in 2022.
Every Breath You Take
The Global Burden of Disease (GBD) consortium found that pollution accounted for 9 million deaths worldwide in 2019. Of these, over 5 million were due to cardiovascular disease.1
Air pollution is split into two categories – ambient particulate matter (<2.5 μm [PM2.5]) and household air pollution. Household air pollution is primarily a result of indoor use of dirty solid fuels (e.g., coal, wood, agricultural waste, etc.). It is a substantial (albeit declining) contributor to cardiovascular mortality in low-income countries and not a major issue in North America.
Ambient air pollution arises principally from fossil fuel combustion and is a problem worldwide. Fine particulate matter refers to particles with an aerodynamic-mass median diameter <2.5 µm. To give an idea of the size of these particles, the average human hair is 70 µm in diameter.

While we face the existential crisis of climate change, most people don't realize that of the many deleterious effects of air pollution, cardiovascular disease is #1.
– Jamal S. Rana, MD, PhD, FACC
The good news is that efforts to decrease air pollution in Europe and North America appear to be working. Michael Brauer, ScD, a professor in the School of Population and Public Health at the University of British Columbia and an affiliate professor at the Institute for Health Metrics and Evaluation at the University of Washington, discussed the progress that's been made during a recent JACC online webinar focused on the global burden of cardiovascular disease:
"For the sources of air pollution that we can control, we've actually seen great progress in North America. It's one of the few places in the world where we've seen reductions in the health impacts of air pollution. Western Europe also has seen some reductions, but not as dramatic as in North America. Most of the rest of the world, though, is going in the other direction."
Strict regulation in the U.S. has worked to bring down the levels of pollutants, with a concomitant reduction in the risk of pollution-related cardiovascular disease. According to the U.S. Environmental Protection Agency (EPA), which tracks air quality trends using measurements from monitors located across the country, air quality based on concentrations of the common pollutants has improved nationally since 1980. For example, lead emissions have dropped 76% since 2000 and 99% since 1980, as a result of the permanent phase-out of leaded gasoline. And this is despite substantial increases in gross domestic product, vehicle miles traveled and energy consumption.
However, the bad news is that, beyond air pollution, the burning of fossil fuels is changing our climate by increasing levels of heat-trapping pollution such as carbon dioxide in the Earth's atmosphere. Those rising temperatures are fueling more extreme weather and contributing to dangerous heat waves, dramatic spikes in air pollution, a surge in wildfires, and other issues that are expected to trigger marked increases in harm to public health.
"Due to the warmer climate, we're pretty well locked into a future of more wildfires, more frequent wildfires, a longer wildfire season, and more severe wildfires that are very difficult, if not impossible, to suppress," says Brauer. Ironically, he adds, the wildfires are serving to increase awareness of air pollution.
Don't Go Breaking My Heart
There is a wealth of data showing the effects of air pollution on the whole spectrum of cardiovascular disease, from myocardial infarction (MI) to stroke, to cardiac arrest, heart failure exacerbation and arrhythmias. Elevated levels of particulate matter in the air increase the relative risk of acute cardiovascular events by 1% to 3% within a few days. Longer-term exposure increases this risk by about 10%, says Sanjay Rajagopalan, MD, and colleagues in a JACC state-of-the-art review. Air pollution has also been associated with an increased risk of atrial fibrillation and ventricular arrhythmias.2
Long-term exposure to ambient PM2.5 has also been linked to subclinical cardiovascular disease such as left ventricular hypertrophy, increased carotid intima media thickness, and calcification of both the coronary artery and abdominal aorta.
In 2019, about 99% of the world population was living in places where the World Health Organization air quality guidelines of <10 mg/m3 for annual levels and <20 mg/m3 for daily levels were not met.3 Prolonged exposure to PM2.5 at 50 μg/m3 doubles the risk of developing cardiovascular diseaes.4
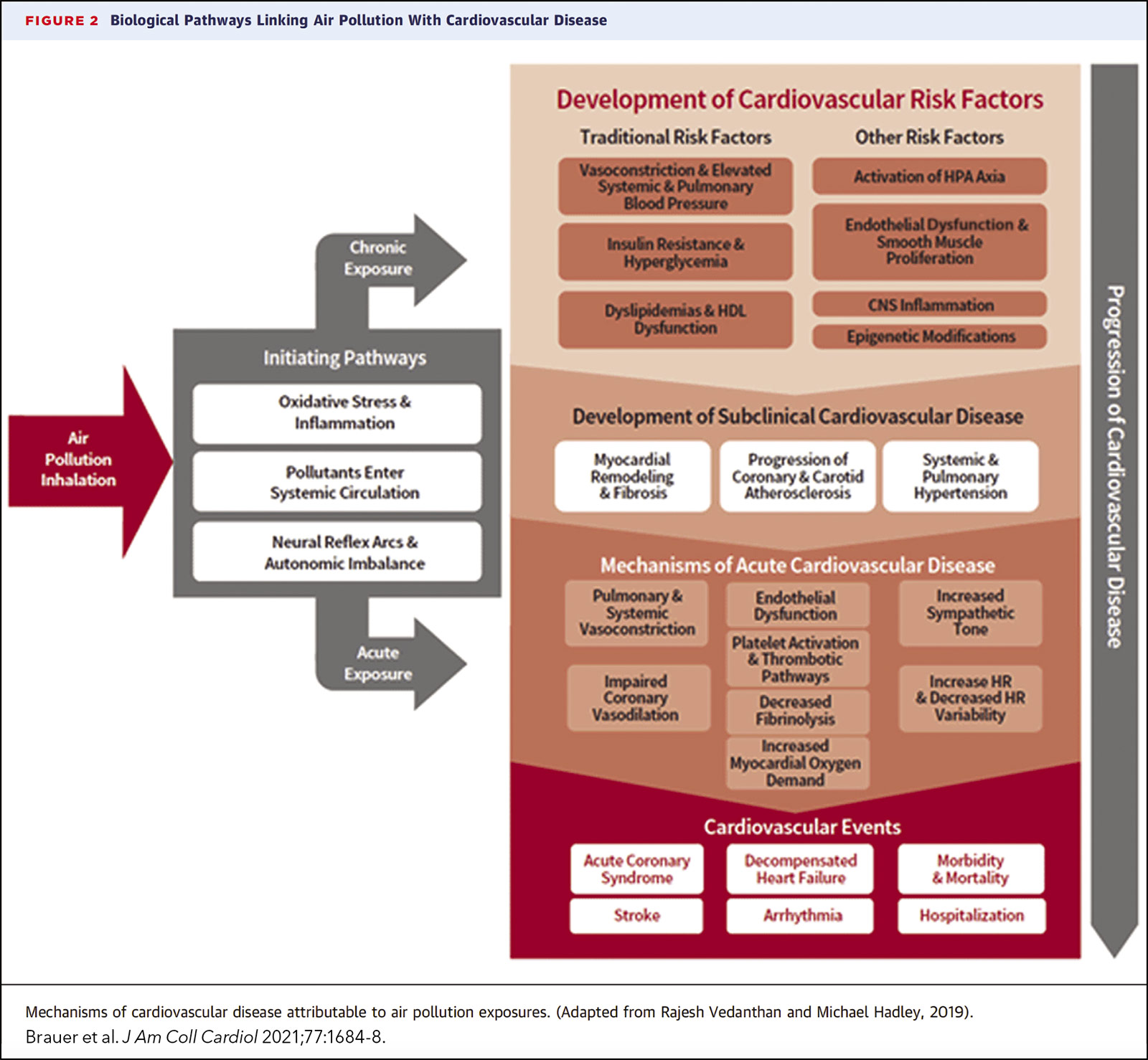
The pathophysiologic mechanisms and biologic pathways through which PM2.5 triggers cardiovascular events are numerous (Figure 1).5 A scientific statement from the American Heart Association suggests that acute and chronic inhalation of particulate matter initiates extrapulmonary effects on the cardiovascular system via three broad "intermediary" pathways: 1) the release of proinflammatory mediators or vasculoactive molecules; 2) perturbation of the autonomic nervous system balance or heart rhythm by particle interactions with lung receptors; and, 3) potentially, the translocation of particulate matter or particle constituents directly into the systemic circulation.6
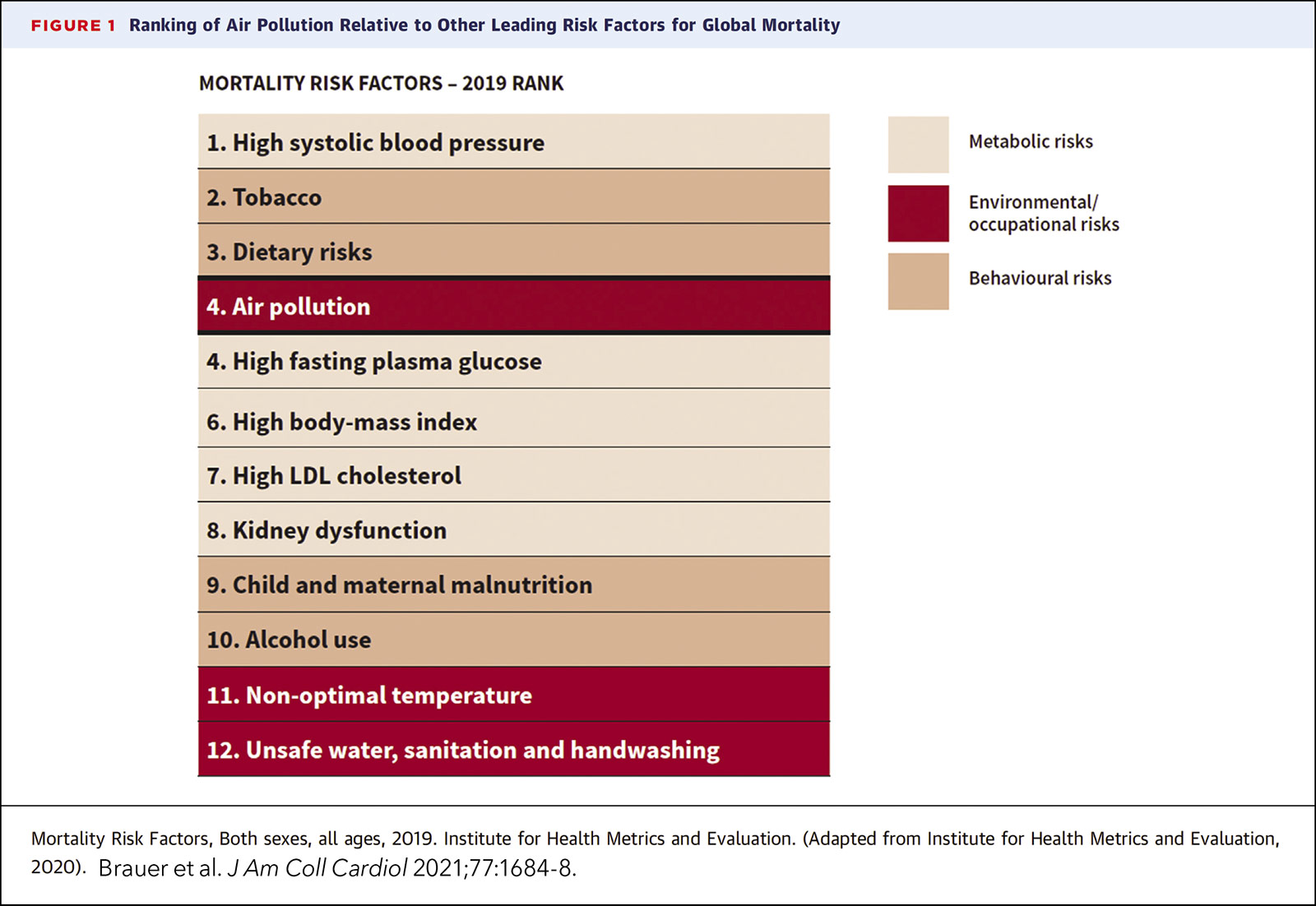
According to a recent report from the World Heart Federation Air Pollution Expert Group, globally, air pollution ranked the fourth highest among risk factors for mortality, beating out high LDL-C, high body mass index, physical inactivity and alcohol use (Figure 2).5 Nonoptimal temperature ranked 11th.

In the context of environmental risk factors, individuals really have very little control over what they're exposed to, which is different than, say, dietary risk factors for disease or other things related to behavior.
– Michael Brauer, ScD
"Certainly, anecdotally, when we've had these big wildfires around the San Francisco Bay Area, we felt like we were seeing many more MIs in the cath lab," says Rana, who is an adjunct investigator with the Division of Research at Kaiser Permanente. "But what we still need to better tease out is whether the increase in events is due to the smoke itself or to extra emotional distress from the fire, or something else."
Rana has teamed with Stacey E. Alexeeff, PhD, a research scientist and biostatistician at the Kaiser Permanente Norther California Division of Research, to conduct a study that aims to quantify the impact of wildfire air pollution on rates of cardiovascular events and mortality, and to determine which subpopulations are at greatest risk due to underlying comorbidities.
Their study is unique in that it uses detailed health information on important confounders (smoking status, body mass index, comorbidities) on the entire adult membership of Kaiser Permanente Northern California (3.7 million members) linked to geocoded longitudinal residential address data and air pollution and wildfire smoke data.
"Particulate matter is just a measure of how many particles of a certain size are in the air that we're breathing, but it doesn't differentiate the kinds of particles," says Alexeeff. "We feel pretty comfortable discussing at what level of particulate matter things get unhealthy, but we don't know as much about whether certain particles are more harmful than others."
"How are the particles from a wildfire different from the air pollution that we breathe every day, which mostly comes from vehicles and industrial sources," she asks. And what's burned by a wildfire can vary, sometimes it's vegetation and others it's buildings. When some 18,000 structures burned in Paradise in Northern California in 2018, there were higher levels of lead and zinc. Such impacts need to be better understood, she adds.
The Heat is On
Scorching heat, deadly floods, wildfires, drought. Around the world, climate change continues to make the unprecedented precedented, and to deadly effect.
According to a just-released report from the National Oceanic and Atmospheric Administration, the Earth had its sixth-warmest August in history; the Northern Hemisphere had its second-warmest meteorological summer on record; and the U.S. saw its third-hottest summer.
Studies show that as the climate warms, the frequency of heat waves dramatically increases – as does the severity and longevity of such events, and to deadly effect:
- A 3-day extreme heat event in the United Kingdom, where air conditioning in homes is not widespread, is thought to have killed upwards of 1,000 individuals, almost half of whom were aged 85 years or older.
- By mid-July, over 2,000 people had died in Spain and Portugal over a span of less than 12 days from heat-related causes as a heat wave moved through Europe. The heat wave was accompanied by wildfires that forced firefighters to battle flames in searing heat in France, Spain, Portugal, Greece, Croatia and Slovenia. Tens of thousands of people were evacuated from their homes.
- As per the U.S. Centers for Disease Control and Prevention, from 2018-2020, 3,066 people died from heat-related causes in the U.S. Heat-related deaths in 2021 exceeded both 10-year and 30-year averages, and 2022 was even hotter. Estimates suggest the number of heat-related deaths in 2022 could be double previous highs.
Deaths attributable to heat stroke are actually a minority of the overall deaths attributed to extreme heat.7 Similar to air pollution, it's the deaths from cardiovascular and cerebrovascular disease that are likely the more important contributor to overall heat-related deaths.
Age is an important factor, with the elderly shouldering the lion's share of the heat-related increase in death. Some of the reasons for this are logistic – elderly people are more likely to have physical and socioeconomic limitations that limit their ability to manage extreme heat events.
But there are a number of physiological changes associated with aging that also predispose older folks to heat-related circulatory collapse.8 Older adults produce less sweat so they have less evaporative cooling efficiency, a problem exacerbated by the fact that elderly people are less able to redirect blood flow away from the deep splanchnic vasculature to the skin to facilitate cooling. Also, the aging heart has weaker contractile force in response to heat, limiting cardiac output in response to drops in blood pressure and left ventricular preload (both of which are a response to dehydration).
These physiologic limitations are particularly intensified in older adults with cardiovascular disease, many of whom are also taking medications that further increase vulnerability to heat. For example, diuretics increase dehydration risk and beta-blockers reduce the heart's ability to augment rate and stroke volume in response to increased circulatory demand.
Quit Playing Games (With My Heart)
At first glance, one might expect environmental assaults like air pollution and extreme heat to be equal opportunity killers. Neither respect boundaries of any sort. But, in reality, like so much else, the disadvantaged are far more likely to be adversely impacted by extreme weather events.
Of course, as with most research into the social determinants of health, the causal chain is near impossible to disentangle. One study published earlier this summer looked at data from 3,108 counties from 2008 to 2017, matching up county-level maximum heat index for all counties in the contiguous U.S. in summer months and monthly cardiovascular mortality rates.7

Proximity to industry, high traffic areas, less greenspace – these are things that play into disparities in the impact of air pollution and extreme heat that are likely multiplied by other disadvantages in these populations.
– Stacey E. Alexeeff, PhD
For each additional extreme-heat day (maximum heat index ≥90°F [32.2°C]), there was a 0.12% higher monthly rate of cardiovascular mortality (p=0.004), leading to an estimated 5,958 additional deaths from cardiovascular disease over the study period (which is more than the EPA estimate for all heat-related deaths, suggesting some likely undercounting on the part of the EPA).
In subgroup analyses, greater relative increases in mortality were seen among men compared with women (0.20%) and among non-Hispanic Black compared with non-Hispanic White adults (0.19%). Not surprisingly, there was also a greater absolute increase among elderly adults compared with nonelderly adults (16.6 additional deaths per 10 million individuals per month).
"In the context of environmental risk factors, individuals really have very little control over what they're exposed to, which is different than, say, dietary risk factors for disease or other things related to behavior, says Brauer. "Where you live really determines your level of risk. But if we modify an environmental risk factor, everyone benefits because there is no behavioral aspect."
In a study that used Land Surface Temperature data to understand patterns of surface urban heat disparities in >1,000 counties across the continental U.S., across most of the country daytime urban warming was greater in lower-income census tracts. This meshes with Alexeeff's research, which has shown that neighborhoods with more greenspace and greater walkability housed populations with lower cardiovascular disease mortality compared with areas with low greenspace and walkability.9
"Proximity to industry, high traffic areas, less greenspace – these are things that play into disparities in the impact of air pollution and extreme heat that are likely multiplied by other disadvantages in these populations," says Alexeeff.
Shelter From the Storm
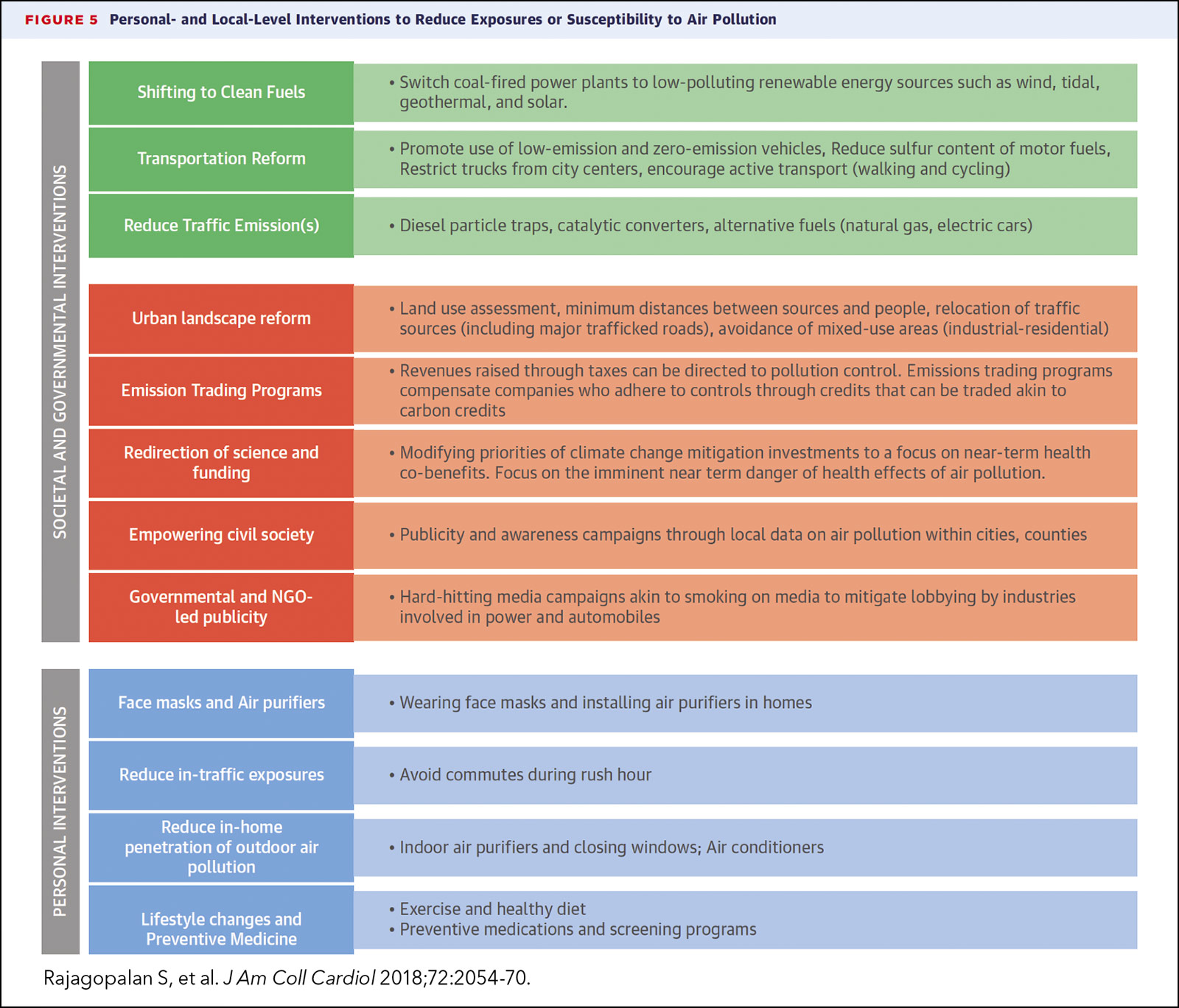
Obviously, climate change requires a societal response. Yet, there are important patient-level and community-level activities that can mitigate risk (Figure 3). "Society can't put the entire onus on the individual patient when it comes to things like extreme heat and air pollution. But there are ample opportunities to be more mindful and pre-emptive to reduce the risks for your patients," says Rana.
"Importantly, health care providers should screen older patients regularly to assess their level of vulnerability to weather-related events and provide personal risk mitigation strategies," says Rana. One simple solution on bad air days is face masks. "It's hard to say there are any silver linings to COVID, but certainly people are more accepting and attuned to wearing N95 masks on bad air days than they were before."
"Environmental stressors should be included in the list of risks we discuss with patients," says Alexeeff. Along with talking with a patient about a better diet, more exercise and taking their medications, clinicians should routinely discuss wearing a mask or taking other measures when exposure could be high. "This would be a big step forward," she adds, "along with acknowledging that a patient lives in a high pollution area and how that might impact their health status."
Clinicians also need to provide vulnerable patients with personal management plans, says Brauer, which is a combination of ensuring patients have access to their clinical care and their medications in the event they are displaced by an event. Add to that access to personal protective equipment and HEPA filtration devices, "which might entail providing these items to low-income populations." As well as making sure they have access to clean air shelters during a wildfire, cooling stations during extreme heat events, etc. The important part is that these things should be put in place before the events occur, says Brauer.
Most personal mitigation strategies have not been formally tested and shown to reduce clinical events, but some have been shown to at least improve some biomarkers of cardiometabolic health. Portable air filters can lower indoor PM2.5 levels by >50% and are proven to improve a growing list of surrogate endpoints, including blood pressure, insulin sensitivity, inflammatory markers, stress hormones and metabolomic profiles.10
"I think clinicians have a role to play in raising awareness and advocating for change, in general, but for air pollution specifically," says Brauer. "Understanding that it's a risk factor for cardiovascular disease and understanding that an improvement in air quality will equitably and efficiently benefit everyone is really important."
This article was authored by Debra L. Beck, MSc.
References
- Murray CJL, Aravkin AY, Zheng P, et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1223-49.
- Rajagopalan S, Landrigan PJ. Pollution and the heart. N Engl J Med 2021;385:1881-92.
- Ambient (outdoor) air pollution. Accessed Sept. 18, 2022. Available here.
- Rajagopalan S, Al -Kindi Sadeer G, Brook RD. Air pollution and cardiovascular disease. J Am Coll Cardiol 2018;72:2054-70.
- Brauer M, Casadei B, Harrington RA, et al. Taking a Stand against air pollution—The Impact on cardiovascular disease. J Am Coll Cardiol 2021;77:1684-88.
- Brook RD, Rajagopalan S, Pope CA, et al. Particulate matter air pollution and cardiovascular disease. Circulation 2010;121:2331-78.
- Khatana SAM, Werner RM, Groeneveld PW. Association of Extreme Heat and Cardiovascular Mortality in the United States: A county-level longitudinal analysis from 2008 to 2017. Circulation 2022;June 21:[Epub ahead of print].
- Chang AY, Tan AX, Nadeau KC, Odden MC. Aging hearts in a hotter, more turbulent world: The impacts of climate change on the cardiovascular health of older adults. Curr Cardiol Rep 2022;24:749-60.
- Liao NS, Van Den Eeden SK, Sidney S, et al. Joint associations between neighborhood walkability, greenness, and particulate air pollution on cardiovascular mortality among adults with a history of stroke or acute myocardial infarction. Environ Epidemiol Phila Pa 2022;6(2):e200.
- Newman JD, Bhatt DL, Rajagopalan S, et al. Cardiopulmonary impact of particulate air pollution in high-risk populations. J Am Coll Cardiol 2020;76:2878-94.
Clinical Topics: Acute Coronary Syndromes, Geriatric Cardiology, Heart Failure and Cardiomyopathies, Prevention, Acute Heart Failure
Keywords: ACC Publications, Cardiology Magazine, Heart Failure, Acute Coronary Syndrome, Secondary Prevention, Geriatrics, Social Determinants of Health, Health Equity, Climate Change
< Back to Listings