New in Clinical Guidance | Same-Day Discharge For Intracardiac Catheter Ablation; Chronic Coronary Disease Performance, Quality Measures
Same-Day Discharge For Intracardiac Catheter Ablation: New HRS/ACC Scientific Statement
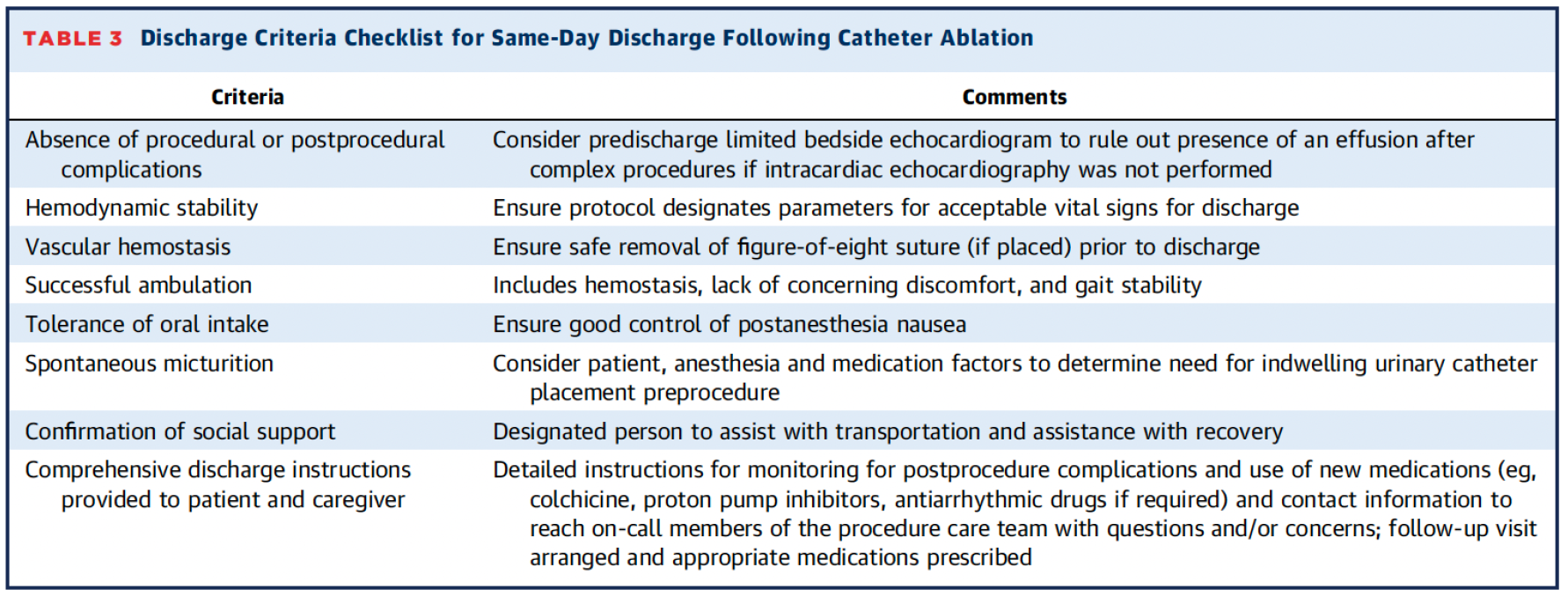
With an increasing shift towards same-day discharge (SDD) as a means of improving access for an increasing number of patients undergoing intracardiac catheter ablation, a new Scientific Statement from the Heart Rhythm Society (HRS) and the ACC offers guiding principles and best practices for effective SDD strategies based on the latest global clinical data and real-world evidence.
The statement, chaired by Amit J. Shanker, MD, FACC, and Samuel O. Jones, MD, MPH, FACC, and published in JACC, highlights recent data underscoring the benefits of cardiac ablation SDD strategies on patient safety and access, as well as advances in technology that are helping to improve procedural efficiencies and reduce the length of hospitalization and mitigate costs.
Among the recommendations when considering an SDD strategy, the statement urges a shared decision-making approach between the clinician and patient that takes into account patient safety, comfort and procedural outcomes. It also recommends that any SDD protocol carefully consider baseline patients factors for preprocedural screening, procedural planning and postprocedure management. Additionally, the statement stresses the need for "well-considered plans" that anticipate complications, potential transfer to inpatient facilities if at an ambulatory surgery centers (ASC), and other logistical issues and that "intentionally support close coordination of care with patients and their caregivers."
Looking ahead, the statement supports the use of clinical registries and quality measures to track real-world outcomes and continues to inform and evolve future SDD best practices and strategies.
"Access challenges (exacerbated during the COVID-19 public health emergency) and economic pressures have driven a shift in practice trends to reduce hospitalization duration and optimize resource utilization," write Shanker, Jones and colleagues. "This has necessitated an evolution in clinical flow paradigms to include alternate sites of care (i.e., ASCs and office-based laboratories). To that end, an SDD strategy could result in significant operational efficiencies at the hospital/facility level, improvement in patient access, improvement in the patient's perceived benefit, and result in reduction in overall health care expenditures and resource utilization."
Read the full document in JACC.
New ACC/AHA Performance and Quality Measures Address Chronic Coronary Disease
With chronic coronary disease (CCD) the leading cause of death in the U.S., new clinical performance and quality measures released by the ACC and the American Heart Association offer practical steps for managing patient care that are aligned with the latest evidence-based CCD guidelines.
The comprehensive measure set document developed in collaboration with the American College of Clinical Pharmacy, American Society for Preventive Cardiology, Preventive Cardiovascular Nurses Association, and the Society for Cardiovascular Angiography and Interventions, includes 10 performance measures and three quality measures – six of which are new.
Most measures are appropriate for public reporting or pay-for-performance programs, with those that are not ready for reporting purposes potentially useful to clinicians and health care organizations for quality improvement, according to Writing Group Chair Marlene S. Williams, MD, FACC, Vice Chair Glenn N. Levine, MD, FACC, et al.
Highlights from the document include new performance measures for lipid measurement, high-intensity statin use, medical management therapy for blood pressure, and avoidance of routine periodic testing in stable patients. New quality measures address imaging for CCD "to ensure appropriate evaluation in the setting of changing symptoms," as well as ongoing patient education to help inform discussions between patients and clinicians.
Additionally, the writing group revised several measures to reflect new evidence involving blood pressure and lipid control, as well as screening, cessation and intervention for tobacco use. Other revised measures address appropriate antiplatelet therapy; beta-blocker therapy for patients with prior myocardial infarction or left ventricular systolic dysfunction (LVSD); ACE Inhibitor and ARB use in patients with diabetes or LVSD; and cardiac rehabilitation referral for patients with CCD from an outpatient setting.
Looking forward, the document also includes a focus on possible future areas of research ranging from "ideal antiplatelet regimen for secondary prevention and post–acute coronary syndrome" to "clarification on ambulatory blood pressure measurements" in the CCD population.
Keywords: Cardiology Magazine, ACC Publications, Cardiac Catheters, Quality Indicators, Health Care, Registries, Patient Discharge, Quality Improvement, Coronary Disease, Quality Control