Quality Improvement For Institutions | Local Processes to Improve Clinician Well-Being: A Recipe for Success

Clinician burnout is a substantial concern throughout the house of medicine and within health care systems, as well as for clinicians themselves. Professional medical societies, including the ACC,1 are working to address clinician burnout.
The cost of burnout and the return on investment in addressing clinician well-being is now a focus in the medical literature.2
Increasingly clinicians across the care team are becoming dissatisfied. A 2019 Medscape survey found that cardiovascular specialists were ranked at number 23 for satisfaction in their chosen profession among 27 specialties.3
Further, only 31 percent of survey respondents said they were happy at work.
Most disturbing is a suicide rate of at least 400 physicians per year – a rate two-times higher than the general population, with physician rates of depression at 39 percent.4
Data clearly affirm that burnout affects productivity – a system issue. But more importantly it affects quality of care – a patient issue.5,6
Despite the magnitude of the problem, few practical solutions have been identified.7 In fact, the interventional cardiology community in a recent online discussion about clinician burnout suggested they may be far behind in recognizing the problem.8
Research at Lee Health's Heart and Vascular Institute

Clinician wellness is a top priority in the Lee Health System and its Heart and Vascular Institute (HVI). The HVI is a collaboration between cardiologists (both System-employed and independent) for quality and system improvement.
This year, HVI took a proactive approach to document the level of burnout within its entire cardiovascular team and to explore constructive ways to create system-wide processes to address the issues. The Provider Wellness Committee, including cardiologists, advanced providers and cardiovascular care nurses, ensured the effort was inclusive of all stakeholders.
While focusing on Lee Health locally, it is an aspiration that this may also serve as a template for other institutions to address the issue of burnout through a quality improvement process. A process metric for clinician burnout-related improvement developed by HVI leadership was approved by the HVI Board of Directors and System administration. This process metric was included in the HVI physician incentive bonus as part of core metrics for quality improvement for the current fiscal year.
The Maslach Burnout Inventory, modified to identify local issues, was selected as the survey instrument to identify and quantify burnout. This well-validated instrument has an advantage of relative ease of administration.9
The survey was sent to all cardiovascular clinicians at HVI: cardiologists, interventional cardiologists, advanced providers and cardiac nurses. The survey was administered by a third-party via email.
An initial email introduced the survey and subsequent follow-up emails encouraged participation. The survey was open from May 6, 2019 to June 19, 2019. All responses were anonymous. All results, including written comments, were sent to the Provider Wellness Committee.
Two working groups, subsets of the Provider Wellness Committee, one focused on IT and one on staffing, was charged with analyzing the data and developing specific recommendations and action plans. The working groups had the same diversity in staff representation as the overarching committee.
The recommendations and action plans were vetted by the HVI Board and submitted to senior System administrators. The System approved the action plans with assignments to specific administrators with ongoing monitoring and assistance from HVI to continue the process of improvement.
Survey Results
A total of 232 surveys were emailed. The overall response rate of 34 percent was high for general survey participation. There was a 50 percent return rate from physicians.
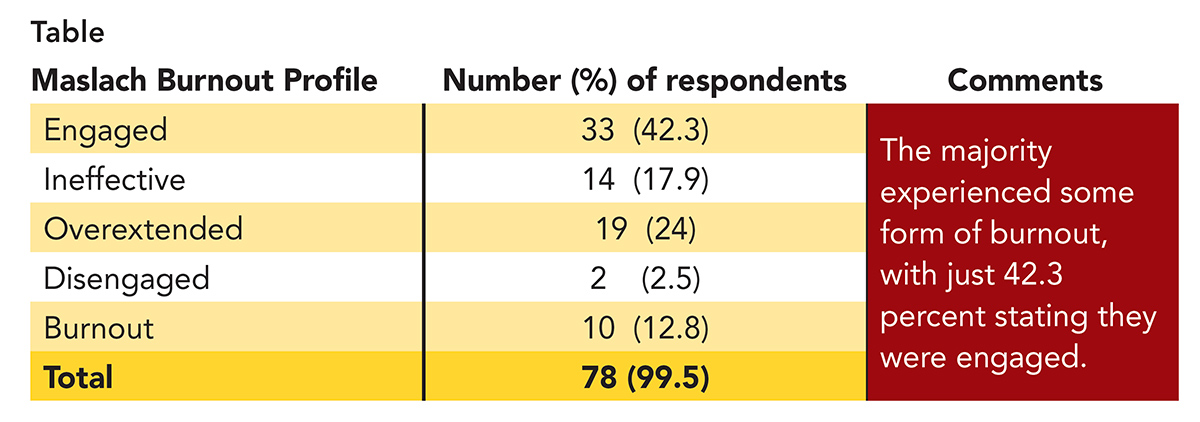
The rate of dissatisfaction with their work was high at 58 percent (Table). This finding is consistent with multiple national surveys.10,11 Ten clinicians (12.8 percent) met the criteria for burnout, which applies to a distinct subset of people who feel significantly challenged throughout all aspects of their job.
Analysis of the Data
The Provider Wellness Committee reviewed all survey data, including write-in comments related to concerns specific to the Lee Health System. Comments and concerns fell into two predominant categories: information technology (IT)/electronic health records (EHR) issues and staffing issues, leading to the formation of the two working groups for these areas.
IT/EHR Stressors
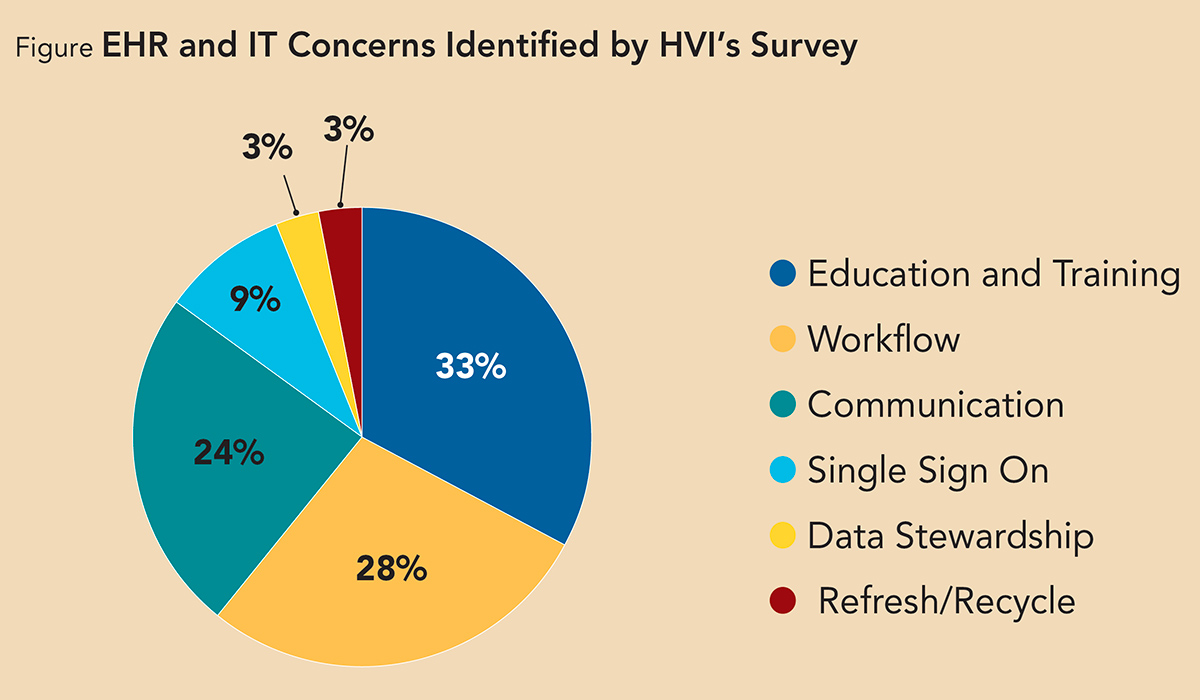
The responses regarding six different domains related to electronic documentation are detailed in the Figure. These results are consistent with other studies suggesting the EHR has a significant impact on clinician burnout.9,10
A notable concern identified through survey comments is that the EHR is shifting tasks back to clinicians, including billing, coding, quality control, data entry, computerized decision support, order entry and e-scribing. Other issues related to efficiency, sign-on and education.
Frustration was voiced about the frequency of changes to the EHR and the volume of emails announcing these changes. Concerns were raised regarding the efficacy of current communications in facilitating smooth integration of new updates. Survey respondents voiced a need for regular training to better learn how to incorporate updates into workflow.
Staffing Issues Stressors
The geographic market served by Lee Health is highly seasonal, presenting real challenges in ensuring adequate and appropriate staffing at all levels, from physicians to nursing and support/office staff.
A significant majority (78 percent) of respondents indicated concern about staffing issues that are greatly impacted by temporal shifts in demand. Observations were made regarding both hospital and outpatient facilities and the perceived lack of a systematic approach to address shortages.
Work Group Recommendations
Lee Health HVI made specific recommendations within three principle areas, based on analysis of the survey results, to Lee Health System administrators.
- IT/EHR
- Increase education and training for all clinicians regarding updates and upgrades in the EHR.
- Develop improved workflows to eliminate redundant work.
- Create an efficient sign-on process.
- Include a member of the IT/EHR Work Group in the system-wide EHR committee.
- Create a feedback mechanism for clinicians to report EHR issues to ensure concerns are identified and addressed.
- Staffing
- Increase the PRN nursing pool.
- Create a work group to address creative job management for all clinicians (locums, part time, job share).
- Evaluate office processes contributing to burnout.
- Develop specific ad hoc committee to address nursing issues.
- Monitoring and Reporting
- Enable ongoing monitoring by the work group with reporting to HVI and administration.
Steps to Address Burnout

The Provider Wellness Committee identified four steps to address burnout:
- Education of System administrators regarding the scope of problem, survey data and comments, and the issues that should be addressed.
- Development of a collaborative process between clinicians and the health system (led by clinicians) to address the issues (a quality process metric was an important driver for engagement in the Lee Health HVI model).
- Assembling a diverse group of clinicians dedicated to documenting important stressors and strategizing ways to collaborate to increase clinician well-being.
- Development of an ongoing plan to continually identify issues and solutions to spur system-wide change.
Actions to Date
As a result of this work, the Lee Health System leadership has accepted all the survey data and reviewed all recommendations. Immediate actions from the leadership include:
- An HVI representative has been added to the System-wide EHR group.
- A feedback mechanism was created to ensure responses to tickets that are submitted for IT problems.
- Two administrators, one for nursing and one for office staff, were assigned to work with the Provider Wellness Committee to address specific staffing concerns.
- The Provider Wellness Committee has been made a standing committee, with ongoing responsibilities for continual improvement to meet clinician needs within HVI.
- The survey will be repeated before the end of the next fiscal year (September 2020) to gauge progress and identify issues.
Conclusion
The issues surrounding clinician well-being and burnout affect patients, physicians, nurses, advanced providers and the health care system. Working with a health care system whose leaders are educated on the importance of dealing with clinician burnout is crucial.
It is incumbent on physicians and clinicians to interact with hospitals and health care systems and move from a paradigm of complaint to a culture of solutions. Our health, and the health of our patients, relies on such leadership.
References
- ACC Leaders Address the Realities of Clinician Burnout at ESC Congress 2019. Available here. Accessed Nov 11, 2019.
- Shanafelt T, Goh J, Sinsky C. The business case for investing in physician well-being. JAMA Intern Med 2017;177:1826-32.
- Medscape National Physician Burnout, Depression & Suicide Report 2019. Available here. Accessed Nov 19, 2019.
- Anderson P. Doctors' suicide rate highest of any profession. Available here. Accessed Nov. 21, 2019.
- White T. Medical Errors May Stem More From Physician Burnout Than Unsafe Health Care Settings. Available here. Accessed Nov. 19. 2019.
- National Academy of Medicine: Action Collaborative on Clinical Well-Being and Resilience. Available here. Accessed Nov 19, 2019.
- Physician Burnout. The scope of the crisis and how to fix it. Medical Economics. Aug 25, 2019. Available here. Accessed Nov 19, 2019.
- Conversations in Cardiology: Should interventional cardiologists get paid for being on call? Available here. Accessed Nov 19, 2019.
- Maslach Burnout Inventory. Available here. Accessed Nov 19. 2019.
- Kroth PJ, Morioka-Douglas N, Veres S, et al. Association of electronic health record design and use factors with clinician stress and burnout. JAMA Netw Open 2019 Aug 2;2(8):e199609.
- Collier R. Electronic health records contributing to physician burnout. CMAJ 2017;189:E1405-6.
Clinical Topics: Prevention, Stress
Keywords: ACC Publications, Cardiology Magazine, Electronic Mail, Electronic Health Records, Depression, Motivation, Frustration, Personal Satisfaction, Quality Improvement, Specialization, Benchmarking, Follow-Up Studies, Outpatients, Physicians, Burnout, Professional, Societies, Medical, Suicide, Quality Control
< Back to Listings