Feature | Advancing Health Equity For Heart Failure Patients: A Case Study for Team-Based Care and Innovation

Caring for vulnerable populations presents some unique challenges. It also offers immense opportunities for innovation to effect positive change for many lives.
To achieve health care parity, emphasis should be placed on addressing not only the medical needs but also the adverse social determinants of health that often serve as barriers to care.
We describe here the contributions of the Grady Heart Failure Program to decreasing health disparities and addressing the needs of our patients through a comprehensive and multidisciplinary approach.
Background

Grady Health System serves as the safety net hospital for residents of metro Atlanta and its environs, providing care for the underserved in partnership with Emory and Morehouse Schools of Medicine. The geographic area served by Grady comprises predominantly underrepresented minority population groups who call Grady their medical home.
The Grady Heart Failure Program (GHFP) is a unique and innovative multidisciplinary program with an overarching goal of promoting health equity by improving the quality of care and outcomes of vulnerable patients with HF.
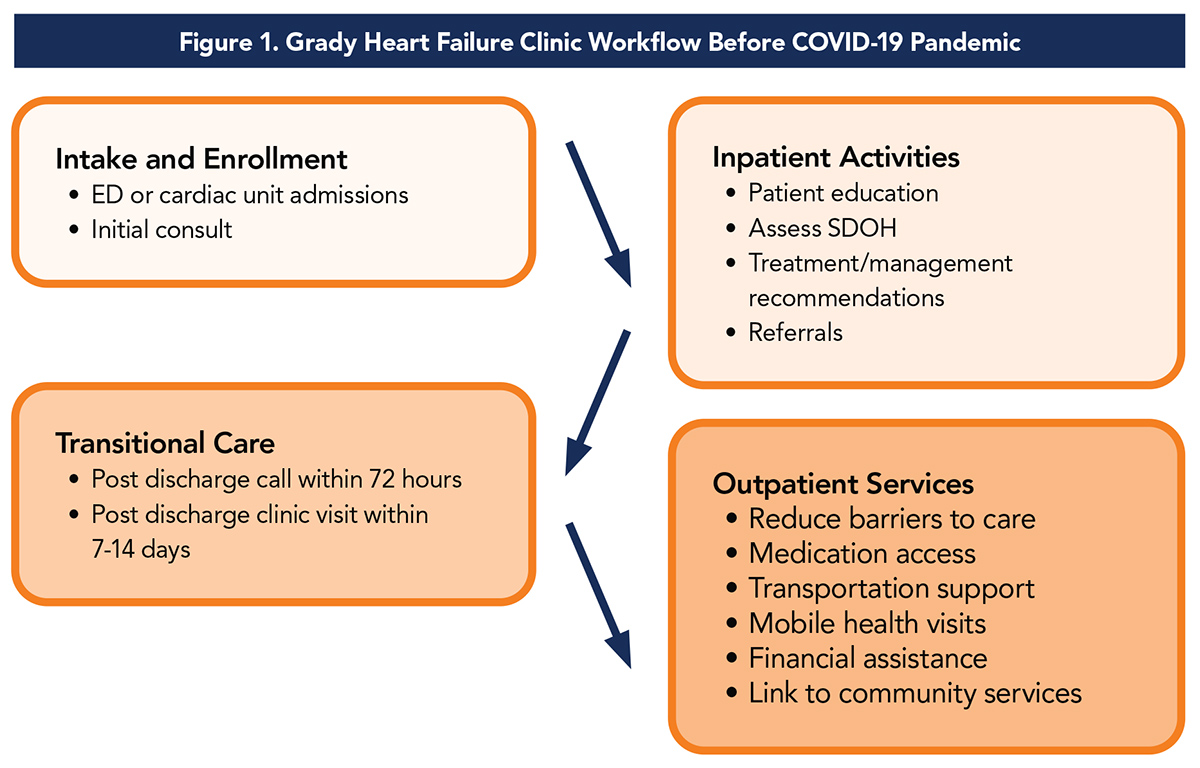
Our program provides a broad range of inpatient and outpatient services. Established in March 2011, the Grady Heart Failure Clinic provides comprehensive outpatient care for patients with HF through coordinated systems of care.
The clinic model focuses on four pillars of management:
- optimizing guideline-directed medical therapy (GDMT)
- patient education
- improving process and access to care, and
- addressing social determinants of health (SDOH)
Integrated in this model are facilitating follow-up in the cardiology and primary care clinics, cardiovascular risk factor management, depression screening and a personalized care approach that focuses on patient autonomy/empowerment skills such as adherence to therapy, dietary modifications, physical activity and daily weight self-assessment.
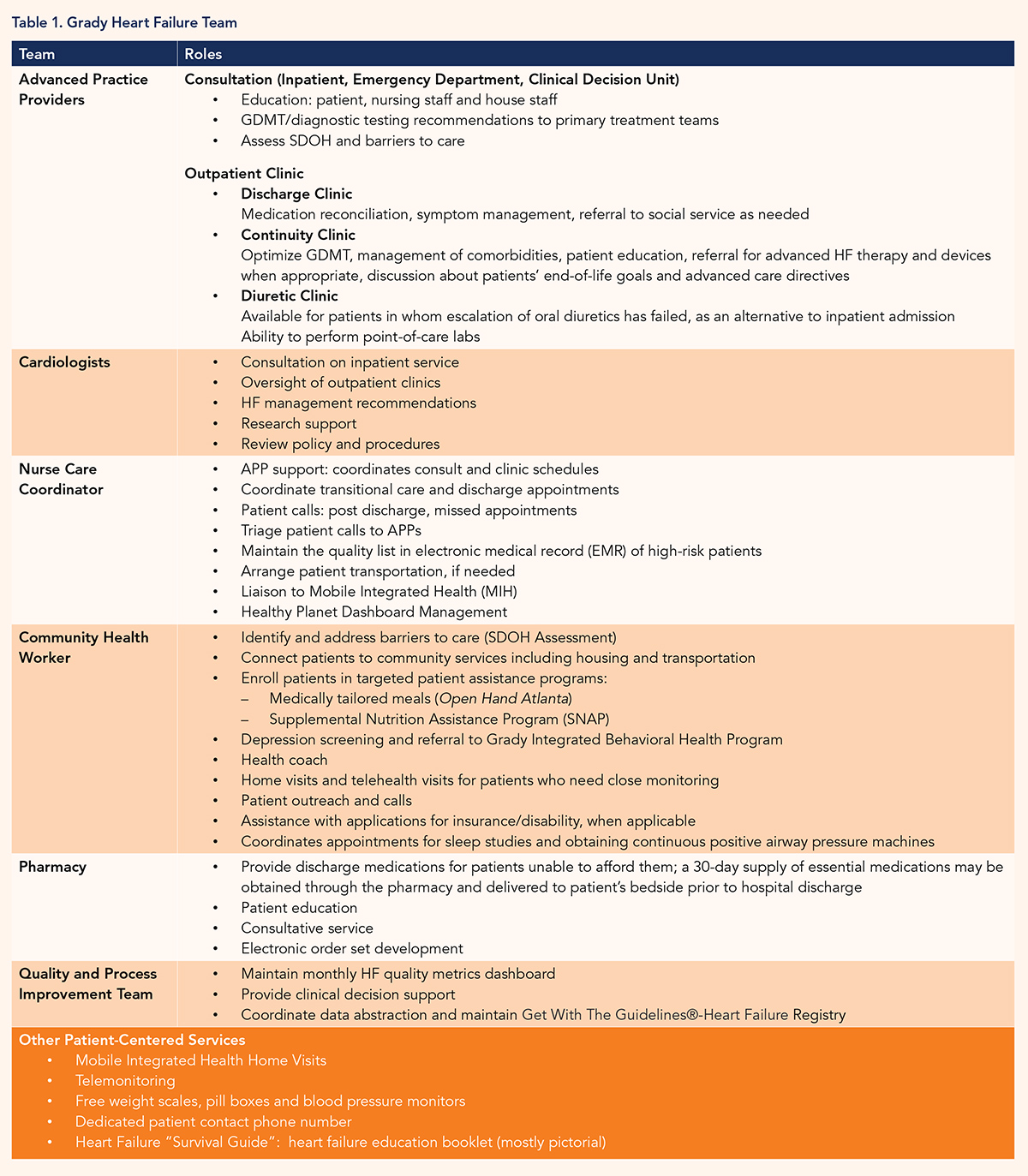
Our Team
Our multidisciplinary team consists of eight full-time and several part-time advanced practice providers (APPs) in collaboration with cardiologists, a community health worker, nurse care coordinator, pharmacist and quality/process improvement personnel (Table 1).
Core Program Components Addressing Barriers to Health Equity
The core components of the GHFP that address barriers to health equity include a 30-day supply of HF medications at hospital discharge, hospital-based financial assistance, connection to community resources by a dedicated community health worker, rideshare support for patients who lack means of transportation to or from clinic appointments, provision of medically tailored meals post discharge, and mobile health home visits for patients unable to leave their residence due to mobility problems or caregiver responsibilities.
Program Innovation
We have developed several innovative programs specifically tailored to meet the unique needs of our patients and improve quality of care. The routine assessment of SDOH is incorporated into our EMR – a care management tool that has an HF-specific component, completed during the initial consultation by the APP.
With the aid of a community grant to support and expand our partnerships, we created education initiatives for patients and their caregivers that included support to overcome identified barriers to care such as low health literacy, financial strain, lack of insurance and lack of transportation.
Remote blood pressure and weight monitoring using a telehealth program was initiated for patients at high risk for recurrent admissions. Although the initial grant funding has ended, we continue to offer remote patient monitoring, free weight scales and blood pressure monitors, and a 30-day supply of medications to our patients through support from the health system and partnerships with national and community organizations.
We provide rideshare support for patients to attend clinic appointments. Our nurse care coordinator and community health worker also manage other innovative services and partnerships: community partnerships such as Open Hand (prepares and delivers healthy meals to patients), Home Instead (provides in-home care and support with common activities of daily living) and mobile integrated health (MIH) home visits.
The Grady MIH Team conducts home visits to patients identified as high-risk for hospital readmissions within 30 days post discharge. Working in close collaboration with the GHFP team, they assess vital signs, assess home safety, perform medication reconciliation and optimization of HF therapy, and administer appropriate point of care tests and intravenous diuretics if needed. Our partnership with the MIH Team has evolved significantly during the COVID-19 pandemic.
Impact of Our Program on Patients With HF
We perform an average of 140 inpatient and 25 clinical decision unit consults each month. We have completed >1,700 inpatient consults in the past year. The HF clinic consists of nine half-day clinic sessions plus four half-day clinic sessions at a neighborhood health center.
A combined census of approximately 600 patients are seen in clinic each month, with >5,000 patient visits in the past year with a staff of five APPs. Over 6,500 unique patients have received care at the Grady HF clinic since its inception in 2011.
By addressing socioeconomic barriers to care, the program has reduced 30-day readmission rates. For FY 2019, the 30-day all-cause readmission rate dropped to 18.5%, compared with 24.9% at inception, and a 30-day HF-related readmission rate of 10.7%.
The program's goal is to reach 85% of eligible patients within three days of initial discharge. To date, we have surpassed that goal, contacting 94.3% of patients by telephone within three days of hospital discharge and scheduling follow-up clinic visits within seven to 14 days post discharge for more than 97% of our patients.
Awards and Recognition
In recognition of the outstanding service provided by the GHFP, the National Association of Public Hospitals and Health Systems (now America's Essential Hospitals) presented our team with the Gage Award for improving quality in vulnerable populations.
The GHFP actively participates in national quality improvement initiatives such as the Get with the Guidelines and Target-Heart Failure programs of the American Heart Association (AHA). Since 2015, the GHFP has received annual recognition for our participation. We are recipients of the highest form of recognition, "Gold Plus Target-Heart Failure Honor Roll" Award, since 2018. This is an advanced level of recognition that acknowledges hospitals for consistent compliance with quality improvement measures outlined in the AHA secondary prevention guidelines for the treatment of HF patients.
The Centers for Disease Control and Prevention (CDC) recognized the GHFP as a promising program that advances health equity, reduces health disparities and addresses the SDOH related to heart disease. We were selected to participate in a rigorous evaluation process with feedback from experts on how to continually improve our processes and practices. Results from this evaluation showed that our patients had significantly fewer readmissions and reduced length of stay, with estimated net savings to the health system of $899,059 for 348 annual averted readmissions.
These national recognitions and awards are a testament to the dedication and passion of our multidisciplinary team to improve outcomes of the patients we serve.
Adapting HF Care in the Time of COVID-19
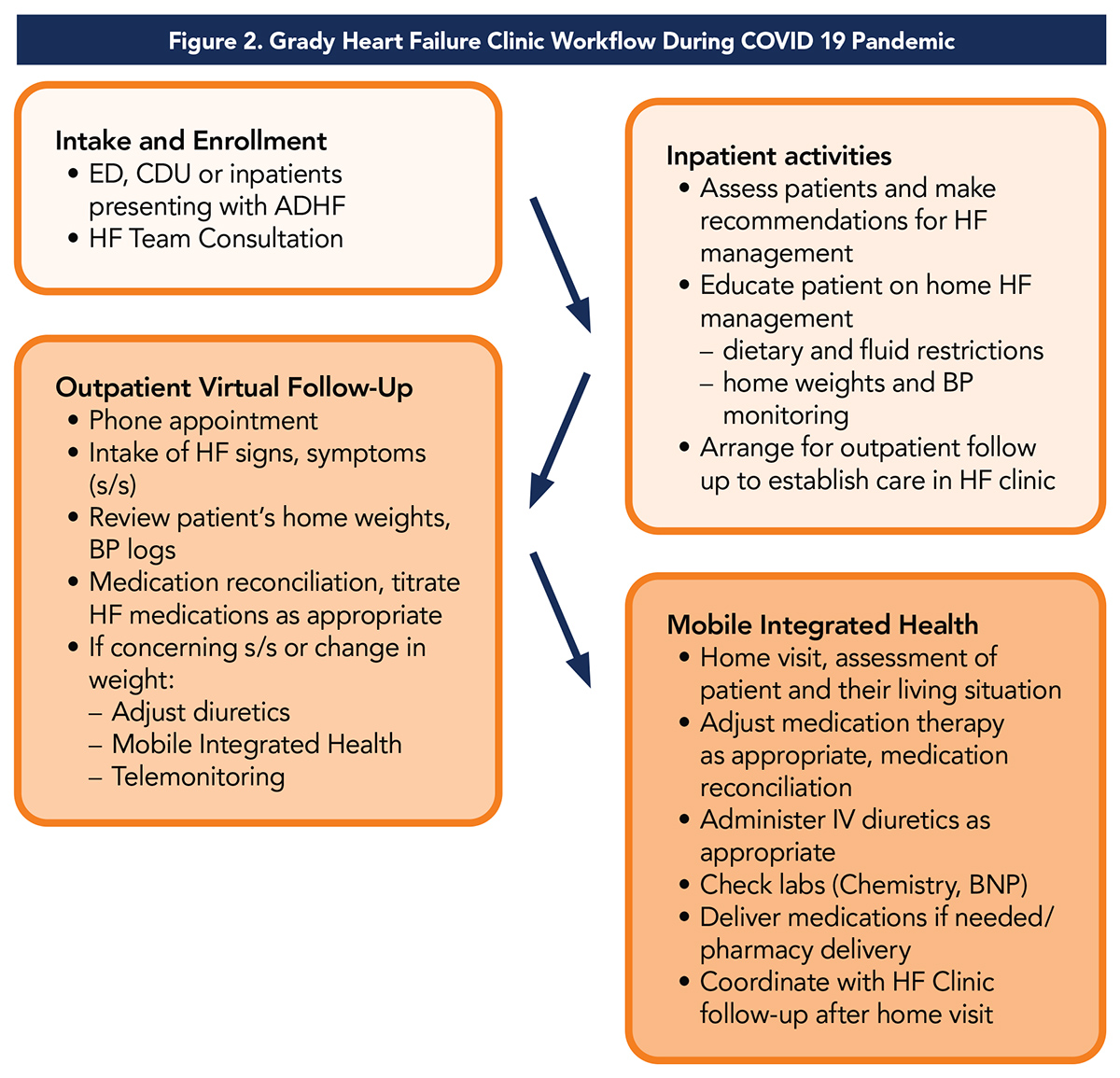
The advent of the novel SARS-CoV-2 virus in 2019 has led to significant changes in the delivery of health care. Accordingly, we modified our clinic workflow to deliver continuous and effective care to our patients during this period. Prioritizing the safety of our patients while recognizing the unique needs of our population has been our primary goal.
Despite the challenges we faced, we continue to provide our patients with access to quality HF care safely, thus promoting health equity during this COVID-19 pandemic, a time that has magnified the effects of health disparities.
The Heart Failure Society of America recently issued a statement, providing guidance on virtual visits, emphasizing the need for patient risk stratification, the importance of having a virtual visit workflow and the role of multidisciplinary HF clinicians such as APPs, physicians, pharmacists and licensed social workers.1
We developed new protocols, which included virtual visits, MIH home visits and remote patient monitoring.
Preliminary comparison of HF clinic visits in the early COVID-19 a seven-week period (March 23-May 9) in 2020 vs. 2019 showed we had only 24 face-to-face visits, vs. 677 in 2019. This reflects a shift from no virtual visits in 2019 to 679 telephone virtual visits and 13 video virtual visits in 2020, along with 122 MIH home visits (vs. none in 2019).
Here are some key changes we made to address disparities during this COVID-19 era:
- Provision of free weight scales and blood pressure monitors to patients prior to hospital discharge or during MIH visits (traditionally given at follow-up clinic visits)
- Access to medications: patients receive their medications from the Grady Pharmacy by mail at no cost
- Access to Care: nurse care coordinator, community health worker and APPs increased communication with our patients through telehealth (decreasing transportation needs)
- MIH Home Visits: in-home follow-up visits for concerns noted during virtual visit. See Figure 2 for more detail.
Conclusion

The success of the Grady Heart Failure Program has truly demonstrated the importance of multidisciplinary team-based care and innovative approaches in managing adverse SDOH and reducing disparities in care for vulnerable patients with HF, as outlined in a recent scientific statement from the AHA on SDOH in this population.2
Since the Program was established nearly a decade ago, we have achieved consistency in the quality of care despite challenges we face in our safety net health system.
Although the COVID-19 pandemic has highlighted significant disparities in health care and intensified the impact of adverse SDOH, we made swift modifications to our current care delivery process to mitigate its effects and ensure that both medical and nonmedical needs of our HF patients are met.
Our ongoing quest remains achieving health equity for our patients through patient-centered activities.
Our passion to ensure equitable access to high-quality medical care for the underserved gives credibility to the saying, "Atlanta can't live without Grady."
Clinical Topics: Cardiovascular Care Team, COVID-19 Hub, Heart Failure and Cardiomyopathies, Acute Heart Failure
Keywords: ACC Publications, Cardiology Magazine, Patient Readmission, Patient Discharge, Pharmacists, Caregivers, Medication Reconciliation, Diuretics, COVID-19, Safety-net Providers, House Calls, Community Health Workers, Inpatients, Blood Pressure, Pregnancy, Heart Failure
< Back to Listings