Feature | Coronary Revascularization the Focus of New ACC/AHA Clinical Guideline

The newest clinical guideline from the ACC and American Heart Association, in partnership with the Society for Cardiovascular Angiography and Interventions, provides an evidence-based approach to the treatment and management of patients with coronary artery disease who are undergoing coronary revascularization.
The 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization addresses a broad range of topics including health equity, duration of dual antiplatelet therapy (DAPT) following PCI, use of revascularization in specific patient populations, involvement of a multidisciplinary heart team, and more.
"Coronary artery disease remains a leading cause of morbidity and mortality globally, and coronary revascularization is an important therapeutic option when managing patients with this disease," said Writing Committee Chair Jennifer S. Lawton, MD. "Treatment recommendations in the guideline outline an evidence-based approach to managing patients … with the intent to improve quality of care and align with patients' interests."
Among the major guideline highlights: a recommendation that all revascularization treatment decisions be based on clinical indications, regardless of sex, race or ethnicity. The guideline notes there is no evidence that some patients with equivalent clinical indications benefit less than others; however, there is evidence that non-White patients are less likely to receive reperfusion therapy or an invasive strategy such as stenting or revascularization surgery.
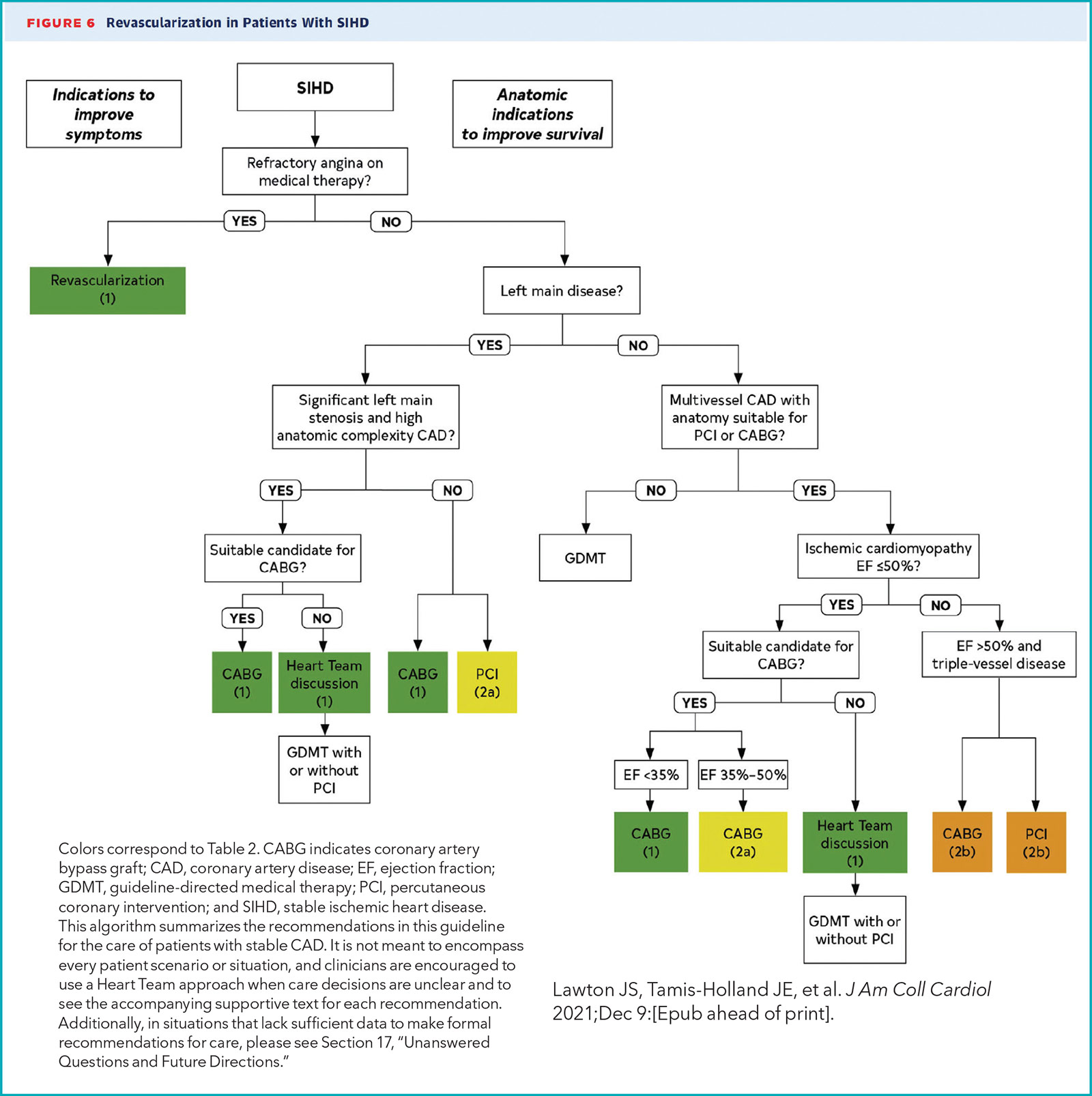
The guideline also updates recommendations for intervention, surgery and/or medical therapy in certain populations, including appropriate use of surgical revascularization or percutaneous revascularization for different disease states. For example, evidence has found that surgery is a reasonable recommendation to improve survival yet may not provide as strong a benefit over medication therapy as previously thought for patients with stable ischemic heart disease (SIHD), normal left ventricular ejection fraction and triple-vessel coronary artery disease. Evidence also shows the ability of PCI to improve survival over medical therapy in this population is uncertain.
When PCI is the most appropriate treatment, the guideline incudes recommendations for radial access vs. femoral when a clinician experienced in radial access is available. Of note, femoral access remains the default for people unable to receive radial artery catheterization because of anatomic limitations or because available clinicians are not experienced to perform radial access PCI. Other recommendations include the feasibility of a shorter duration of one to three months of DAPT after PCI in select patients to reduce the risk of bleeding, compared with previous recommendations of six or 12 months of DAPT.
The guideline also notes that performing PCI of all other significant arteries at a time remote from the initial primary PCI in patients with STEMI and multivessel disease is associated with a lower risk of death or recurrent infarctions than continuing with medical therapy alone. It also underscores that revascularization treatment decisions for coronary artery disease should be based on clinical indications and involve shared decision-making with patients. Specifically, use of the Society of Thoracic Surgeons' score to calculate a patient's surgical risk is recommended. The use of a multidisciplinary heart team approach, especially with patients who have diabetes and triple-vessel disease, is also encouraged to help inform revascularization decisions and optimize outcomes.
"The heart team has become an important paradigm in clinical practice, emphasizing the importance of team consensus on the optimal approach to revascularization," said Jacqueline E. Tamis-Holland, MD, FACC, guideline writing committee vice chair.
Per the rigorous guideline development process, the writing committee for the 2021 Guideline for Coronary Revascularization conducted a comprehensive review of the latest studies, reviews and other literature. The resulting guideline and recommendations replace the coronary artery bypass graft surgery guideline published in 2011, as well as the PCI guidelines published in 2011 and 2015. The guideline was published in the Journal of the American College of Cardiology.
Additionally, the revascularization guideline complements the recently released 2021 AHA/ACC/ASE/CHEST/ SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain – part of strategic efforts by the ACC and AHA to approach guidelines from a real-practice perspective, rather than solely topic-based guidelines.
Clinical Topics: Cardiac Surgery, Cardiovascular Care Team, Invasive Cardiovascular Angiography and Intervention, Stable Ischemic Heart Disease, Vascular Medicine, Atherosclerotic Disease (CAD/PAD), Aortic Surgery, Cardiac Surgery and SIHD, Interventions and Coronary Artery Disease, Interventions and Imaging, Interventions and Vascular Medicine, Angiography, Nuclear Imaging, Chronic Angina
Keywords: ACC Publications, Cardiology Magazine, Platelet Aggregation Inhibitors, Stroke Volume, Coronary Artery Disease, Percutaneous Coronary Intervention, American Heart Association, Consensus, Decision Making, Shared, Feasibility Studies, Health Equity, Mobile Applications, Netherlands, Radial Artery, ST Elevation Myocardial Infarction, Social Media, Ventricular Function, Left, Coronary Artery Bypass, Cardiology, Risk Factors, Catheterization, Reperfusion, Angiography, Algorithms, Chest Pain, Morbidity, Diabetes Mellitus, Surgeons, Writing, Writing
< Back to Listings