Focus on Heart Failure | Pregnancy in Heart Failure: Concerns For All Clinicians

The rates of maternal mortality in the U.S. have risen steadily over the last 20 years, with cardiovascular disease the leading cause, chiefly from cardiomyopathy among other cardiovascular and cerebrovascular conditions.1 Maternal mortality is likely to be further impacted by the recent Supreme Court decision regarding Dobbs v. Jackson and subsequent changes at the state level that pose significant challenges to a woman's access to available health care options.2 These policies are likely to disproportionately impact racial and ethnic minorities as well as women of lower socioeconomic status.
It is the responsibility of all clinicians who care for women of childbearing age to understand the risks of pregnancy associated with particular cardiovascular conditions or direct them to appropriate cardio-obstetrics teams. This includes understanding the safety of various contraceptive options and obtaining a detailed pregnancy history, including preeclampsia and hypertensive disorders of pregnancy, for those with a previous pregnancy. Here is an overview of the relationship between pregnancy and heart failure (HF).
Women With Pre-Existing Cardiomyopathy
For all women with pre-existing cardiomyopathy, preconception counseling should occur in the context of a shared decision-making model to determine if pregnancy is desired and other related goals and patient preferences. If pregnancy is desired, risk assessment should be undertaken using various risk scores.
Advanced heart failure providers typically see women with pulmonary hypertension and/or severe left ventricular (LV) dysfunction (defined as LV ejection fraction (EF) <30% with NYHA Class III or Class IV disease) or previous peripartum cardiomyopathy (PPCM) with any residual systolic dysfunction. Using the modified WHO classification, these women are Class IV, a group associated with an estimated 50% rate of maternal adverse cardiac events.3
These scores help inform discussions with patients regarding the decision to proceed with pregnancy as well as the frequency of cardiac assessment. Management by a multidisciplinary cardio-obstetrics team is advised, including representatives from maternal fetal medicine, cardiology, anesthesia, nutrition and social work, at an experienced center.4
It is imperative that members of the treatment team be aware of the potential teratogenic effects of some guideline-directed medical therapy in women with pre-existing cardiomyopathy of childbearing age. Additionally, we should be empowered to ask patients about sexual activity as well as contraception, and ensure patients understand the potential cardiovascular risks of pregnancy, particularly in cases of advanced HF.
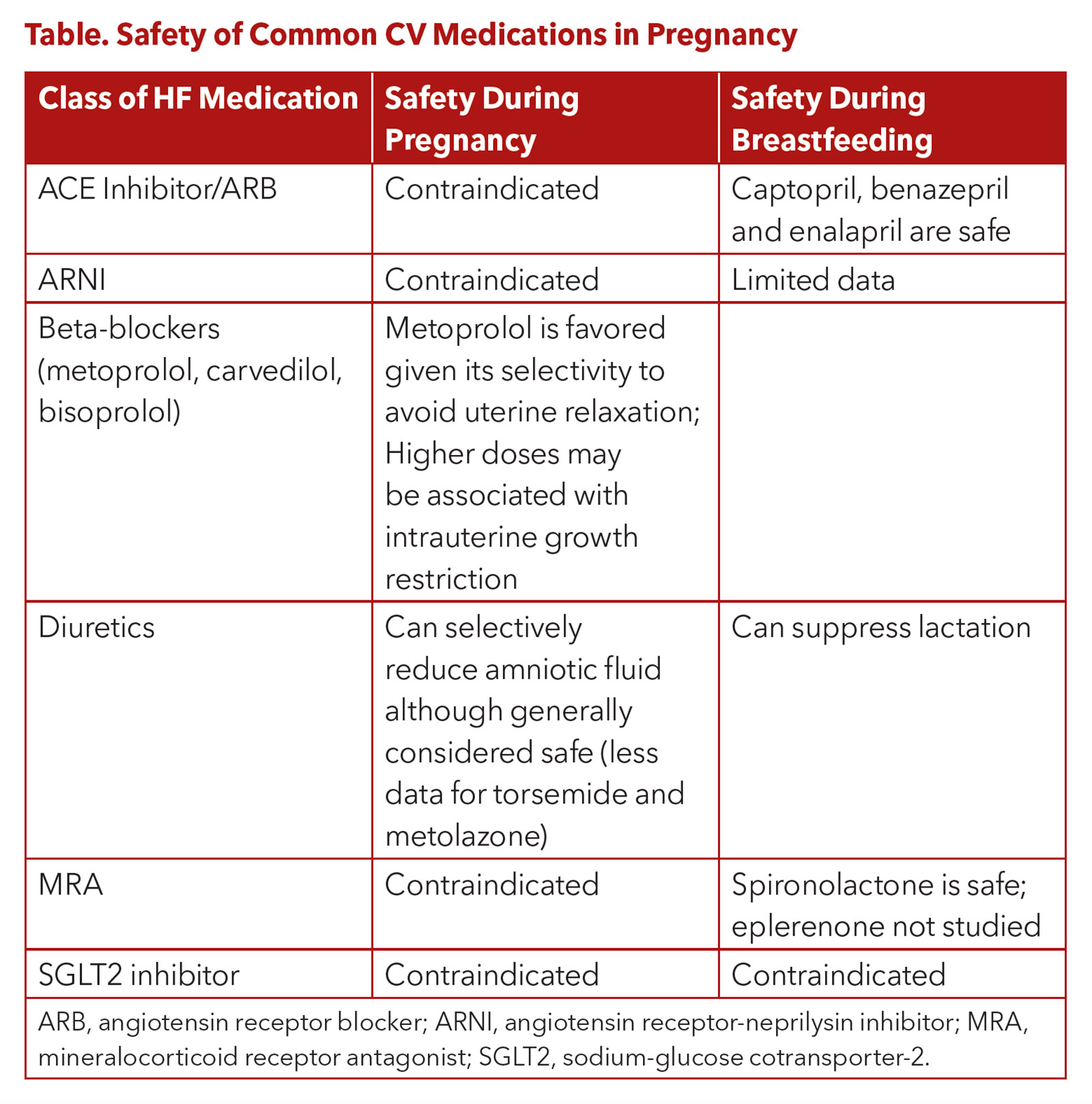
The safety of various commonly used medications for HF are shown in the Table. Pregnancy is not recommended for women supported by LV assist devices (LVAD), although cases of successful pregnancy have been reported.3 After heart transplantation, select women can safely undergo pregnancy. For more detailed information regarding pregnancy after heart transplantation, please refer to dedicated reviews on this topic.3,5
Contraception For Preventing Maternal Cardiac Risk
What's New in HF Pharmacotherapies
Learn to navigate the new and complex heart failure (HF) management landscape with ACC's clinical spotlight series online course, "What's New in HF Pharmacotherapies: The What, How, and Wow." This free on-demand webinar reviews emerging therapies and their practical applications. Complete all three certified patient cases and earn 0.75 CME/CNE credits and MOC points. Click here to learn more.
Given the potential maternal cardiac risks associated with unplanned pregnancy, clinicians should discuss available contraception options with patients who have concomitant cardiac conditions. According to the Centers for Disease Control and Prevention and the American College of Obstetricians and Gynecologists, intrauterine devices are the recommended reversible option for women with high-risk conditions, such as LVEF <30% or a heart transplant.6,7 Combined oral contraceptive pills should be avoided in these patients given the increased risk for thrombotic complications, hypertension and fluid retention. However, progestin-only options may be considered.
New Diagnosis of HF During Pregnancy

Pregnancy serves as a "stress test" for the mother as a result of the increased stroke volume, increased cardiac output, increased heart rate and decrease in systemic vascular resistance.8
PPCM, the most common diagnosis for pregnant women with HF, is defined by a nonischemic cardiomyopathy with LVEF <45% that occurs in the third trimester or in the early postpartum period. Risks factors include preeclampsia, maternal age >30 years, African American race and pregnancies with multiple gestations (i.e., twins, triplets).9 Notably, there may be a delay in diagnosis because of the overlap in common symptoms in HF and normal pregnancy, including lower extremity swelling or shortness of breath. African-American women are known to have a worse prognosis, further highlighting the importance of improving equitable access to cardiovascular care for these women.
In the U.S., >50% of women with PPCM will recover cardiac function. However, some women will go on to require an LVAD or transplant or experience cardiac death.10
Women with PPCM should be counseled regarding the risk with future pregnancies and have access to contraception. Subsequent pregnancies can lead to worsening of systolic function as well as progressive symptoms and worsening functional status.9 Approximately 20% of women who fully recover cardiac function will have a decline in ventricular function in a subsequent pregnancy.10
It is worth noting that PPCM is often a diagnosis of exclusion. The differential diagnosis of HF in pregnancy should also include dilated familial cardiomyopathy, stress cardiomyopathy, hypertrophic cardiomyopathy, LV noncompaction and chemotherapy-induced cardiomyopathy, among others, all of which could be unmasked by the hemodynamic changes associated with pregnancy.3
Learn the Fundamentals of Cardio-Obstetrics on Nov. 18
Join ACC's inaugural Cardio-Obstetric Essentials: Team-Based Management of Cardiovascular Disease and Pregnancy course designed for the entire CV Care Team. Mark your calendar for Nov. 18. Click here to register today.
Advocating For Patients
Now, more than ever, it is important to openly discuss reproductive health as a larger cardiovascular community as well as with our patients. We must ensure, in so much as we can, access to the necessary health services as well as specialized cardio-obstetric care for our patients.
This article was authored by Ersilia M. DeFilippis, MD, FACC, an assistant professor of medicine, Division of Cardiology, Center for Advanced Cardiac Care, at Columbia University Irving Medical Center-New York Presbyterian Hospital.
References
- Mehta LS, Sharma G, Creanga AA, et al. Call to action: Maternal health and saving mothers: A policy statement from the American Heart Association. Circulation 2021;144:e251-e269.
- American College of Cardiology. Guiding Principles and Member Guidance: Maternal CV Care. July 15, 2022. Available here.
- DeFilippis EM, Haythe JH, Walsh MN, Kittleson MM. Intersection of Heart failure and pregnancy: beyond peripartum cardiomyopathy. Circ Heart Fail 2021;14:e008223.
- Magun E, DeFilippis EM, Noble S, et al. Cardiovascular care for pregnant women with cardiovascular disease. J Am Coll Cardiol 2020;76:2102-13.
- Defilippis EM, Kittleson MM. Pregnancy after heart transplantation. J Card Fail 2021;27:176-84.
- Curtis KM, Zapata LB, Pagano HP, et al. Removing unnecessary medical barriers to contraception: celebrating a decade of the U.S. medical eligibility criteria for contraceptive use. J Womens Health (Larchmt) 2021;30:293-300.
- American College of Obstetricians and Gynecologists' Committee on Adolescent Health Care. Gynecologic considerations for adolescents and young women with cardiac conditions: ACOG Committee Opinion, Number 813. Obstet Gynecol 2020;136:e90-e99.
- Davis MB, Arendt K, Bello NA, et al. Team-based care of women with cardiovascular disease from pre-conception through pregnancy and postpartum. J Am Coll Cardiol 2021;77:1763-77.
- Davis MB, Arany Z, McNamara DM, et al. Peripartum cardiomyopathy: JACC State-of-the-Art Review. J Am Coll Cardiol 2020;75:207-21.
- DeFilippis EM, Beale A, Martin T, et al. Heart failure subtypes and cardiomyopathies in women. Circ Res 2022;130:436-54.
Clinical Topics: Heart Failure and Cardiomyopathies, Acute Heart Failure
Keywords: ACC Publications, Cardiology Magazine, Pregnancy, Obstetrics, Heart Failure
< Back to Listings