From the Starting Line | Left Main Bifurcation Stenting: Tips and Tricks

A 48-year-old woman presented with worsening exertional chest pressure on maximally tolerated anti-anginal medications. Exercise stress ECG was positive for ischemia. Coronary angiography revealed 50% stenosis in the left main (LM) with a minimum lumen area (MLA) of 4.9 mm2 on IVUS, 50% stenosis in the proximal left anterior descending (LAD) artery, 30% stenosis in the proximal left circumflex (LCx) and no significant lesions in the right coronary artery. She declined surgical revascularization.
Question: What is the current preferred revascularization strategy for distal LM lesion?
- One-stent approach (provisional stenting).
- Two-stent bifurcation stenting of the LM and LCx.
Left Main Bifurcation Stenting
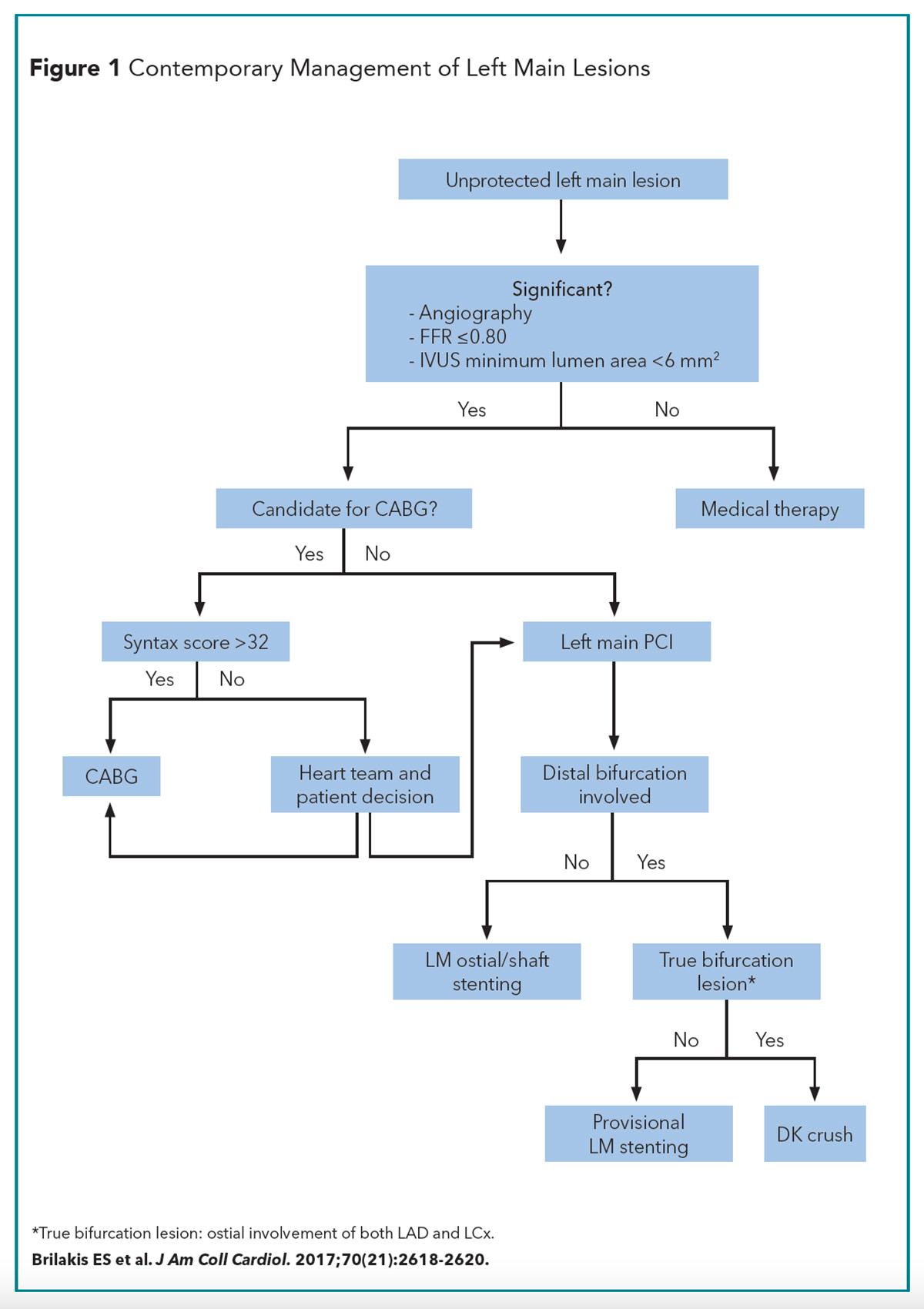
Compared with nonbifurcation PCI, bifurcation PCI is associated with a higher risk of procedural complications, restenosis and lower angiographic success rates.1 As part of our LM revascularization series, the management of LM bifurcation PCI is reviewed here (Figure 1).
LM bifurcation lesions can be classified as simple or complex lesions.2
- Simple: Side branch diameter stenosis <70% and LCx lesion length <10 mm (major criteria).
- Complex: Side branch diameter stenosis >70%, LCx lesion length >10 mm plus presence of any two of six minor criteria: 1) bifurcation angle >70 degrees, 2) presence of thrombus, 3) moderate to severe calcification, 4) main branch diameter <2.5 mm, 5) main branch lesion length >25 mm, 6) multiple lesions.
The challenge with LM bifurcation PCI relates to management of the side branch (LCx in most cases). A provisional one-stent strategy is recommended for simple LM lesions, with conversion to a two-stent approach if the side branch artery is compromised.1
Bifurcation PCI Principles3,4
- Bifurcation anatomy: Assess plaque burden, plaque composition and plaque location (ostial or beyond the ostium) in the LCx and LM, assess LCx diameter and lesion length (≥10 mm) and the bifurcation angle.
- Recognize these mechanisms that may lead to compromised flow in the ostial LCx: 1) plaque shift, 2) carina shift, 3) ellipse deformation of ostial side branch and impact of dissection and protrusion of LM stent struts on side branch arterial flow.
- Predictors of compromised coronary flow in the LCx side branch after LM-to-LAD crossover stenting include: 1) LM artery stent length, 2) LCx plaque burden, 3) ostial LCx MLA on IVUS.5
- Bifurcation angle: The angle between the LCx and LAD determines the risk of side branch (LCx) occlusion during LM PCI, which is impacted by choice of bifurcation stent technique.
- The angle between the LM and LCx determines the ease of wire access into the LCx (side branch). Side branch (LCx) wiring is easier if the bifurcation angle is <70 degrees and difficult when >90 degrees.
- The bifurcation angle is independently associated with vessel revascularization and restenosis.6
- IVUS plays an important role in stent optimization and reduction of adverse cardiac events.7
- True bifurcations, where both the main and side branch are significantly narrowed (>50% stenosis), are Medina 1,1,1 and Medina 0,1,1.
- The decision to treat the bifurcation with a two-stent approach is dictated by the side branch. Non-true bifurcations should be treated with a one-stent technique.
Distal LM PCI Scenario I: LCx Ostium With Minimal Disease (Simple Lesion)
One stent LM-to-LAD crossover (provisional approach) strategy is recommended.1 If ostial LAD is not diseased and predominant lesion is in the LCx, provisional one-stent approach from LM-to-LCx (inverted provisional) can be performed.
- Wire both the LM-LAD and LCx.
- Predilate the main branch.
- A noncompliant (NC) balloon can be used for the LM if sized to the distal main branch diameter.
- If a soft lesion in the LM is anticipated and/or no angiographic evidence of fibrotic/calcified tissue, direct stent implantation to the LM can be performed.
- Consider predilating the LCx if ostial LCx access is difficult, severe and/or calcified LCx lesions exist or LCx coronary flow is compromised after initial wiring.
- Stent the LM artery, jailing the LCx wire.
- The LM artery stent diameter should be sized in reference to the diameter of the distal branch (LAD) to reduce the risk of LCx occlusion from carina shift.
- Balloon dilate the stent in the LM artery with the balloon sized 1:1 to the LM diameter (proximal optimization technique [POT]).
- Rewire the LCx and then remove the jailed LCx wire. The jailed LCx wire helps serve as a marker until LCx rewiring has been successfully performed.
- There are no data to support routine final kissing balloon inflation (KBI) for the one-stent (provisional) approach. If needed, balloon dilation of the LCx and simultaneous KBI should be performed with the LM balloon sized 1:1 with the LAD and the LCx balloon sized 1:1 with the LCx.
- Repeat POT in the LM with the balloon sized 1:1 with the LM.
- If the LCx has a suboptimal result, defined as plaque shift with >75% LCx diameter stenosis or TIMI flow <3 in the LCx, convert to a two-stent approach and perform LCx artery PCI with mandatory final balloon kissing inflation.
Distal LM PCI Scenario II: LCx Suitable For Stenting With Ostial Disease >10 mm (Complex Lesion):
A two-stent approach is recommended. Techniques for LCx stenting for bifurcation PCI are:
- T-stenting and T-and-small protrusion (TAP) stenting
- Recommended for bifurcations angles close to 90 degrees.
- T-stenting and TAP can be used when a one-stent strategy (provisional or inverted provisional) is converted to a two-stent strategy.
- In T-stenting, a stent is positioned at the LCx ostium without protruding into the LM artery stent. TAP is a modification of T-stenting with intentional minimal protrusion of the LCx stent into the LM stent.
- An uninflated balloon (sized 1:1 with LAD) is placed in the LM and then the LCx stent is deployed.
- The LCx stent balloon is then retracted a few mm into the LM and used to flare the protruded (ostial) portion of the LCx stent.
- Simultaneous KBI is then performed with the stent balloon and the previously positioned LM artery balloon. Final POT then can be performed on the LM stent.
- Disadvantages: For a bifurcation angle <0 degrees, T-stenting can lead to incomplete LCx ostial scaffolding or stent protrusion into the LM.
- Culotte
- Culotte is suited for bifurcations with similar diameters in the side branch and distal main branch.
- Culotte can be performed as an upfront two-stent strategy or as a bail-out technique after one-stent deployment in the LM.
- Culotte technique entails rewiring the LCx via a distal stent strut from the LM, then opening LM stent strut with balloon inflation (balloon sized 1:1 with LCx). Subsequently deploy a stent in the LCx with overlap in the distal LM artery. Perform POT of LM artery (balloon sized 1:1 with LM) and final simultaneous KBI.
- Inverted culotte differs from culotte by placing the first stent in the LCx protruding into the LM (size stent to the distal LCx diameter). Inverted culotte is more commonly used when an upfront two-stent strategy is employed for LM bifurcation lesion.
- Double Kissing (DK)-Crush
- DK-Crush is superior to culotte and provisional T-techniques for LM bifurcation in terms of target lesion failure (TLF), target vessel MI and stent thrombosis as shown in DK-CRUSH III and DK-CRUSH V studies which studied true LM bifurcation lesions.8
- The DK-Crush technique starts with predilation of LM and LCx lesions. After placing an uninflated balloon in the LM, deploy a stent (sized 1:1 for the LCx) in the LCx with 1-2 mm protrusion into the LM. After confirming an optimal result in the circumflex and removing the stent balloon, crush the part of the LCx stent protruding in the LM by inflating the LAD balloon. Consider performing POT with a short balloon sized 1:1 with the LM. Rewire the LCx through the crushed stent (preferably proximal recrossing). Perform simultaneous KBI of the LCx and LM (balloons sized 1:1 with LCx and LAD). Deploy a stent in the LM extending into the LAD (sized 1:1 with the LAD), then carefully perform POT of LM portion of the stent (balloon sized 1:1 with LM), then rewire the LCx through the LM stent (crossing proximal stent strut), repeat simultaneous KBI and then final re-POT of LM stent.9
- The 2018 ESC Guideline states the DK-Crush technique (upfront two-stent technique) may be preferred over a provisional one-stent strategy in true LM bifurcations (Class IIb, level of evidence B).10
- Importantly, the DK-Crush trials were performed by operators who perform >300 PCIs per year and at least 20 LM PCIs per year.
- The European Bifurcation Club Left Main Study randomized 467 patients with true unprotected LM bifurcation disease (Medina 1,1,1 or 0,1,1) and side vessel reference diameter >2.75 mm to either stepwise provisional stenting or an intention-to-treat two-stent strategy.11 Patients with acute STEMI, cardiogenic shock, chronic total occlusion or life expectancy <12 months were excluded. The primary endpoint of all-cause death, any MI and target lesion revascularization was similar in both groups: 14.7% (provisional) vs. 17.7% (two-stent) (hazard ratio, 0.8; 95% confidence interval, 0.5-1.3; p=0.34]. Importantly, the majority of patients in the two-stent group underwent T/TAP or culotte stenting and only 5% of patients underwent DK-Crush stenting.
Proximal Optimization Technique
Take-Home Points
- Provisional approach (one-stent technique) is the recommended approach for non-complex LM bifurcation lesions.
- DK-Crush (two-stent approach) is recommended for complex LM bifurcations with extensive LCx disease and/or anticipated difficulty reassessing the LCx artery.
- POT is a critical technique during any LM bifurcation PCI, whether provisional or two-stent.
- Final kissing balloon inflations are optional for provisional but mandatory for any two-stent bifurcation LM technique to reduce complications.
- Mechanical benefits of POT: reduces side branch (LCx) occlusion, facilitates recrossing of the side branch (LCx), reduces risk of inadvertent abluminal wire position (i.e., wire entering the space between the stent and vessel wall), facilitates distal stent strut LCx access, enhances symmetric circular expansion of LM stent and optimizes apposition of the main branch (LM) stent to the side branch (LCx) after LM-LAD crossover stenting is performed.12
- POT reduces TLF, target vessel MI and stent thrombosis.
- POT should be performed after main branch (LM) stenting to correct stent undersizing.
- POT balloon sizing: Use a short NC balloon sized 1:1 with the proximal main vessel (LM in this case).
- POT balloon positioning: Position the POT balloon just proximal to the carina with the distal marker of the balloon placed at the carina, level with the side branch (LCx) ostium. The distal marker of the POT balloon parallelism should not be advanced distal to the carina or it may lead to carina shift. Too proximal balloon positioning leads to inadequate stent expansion over the side branch (LCx) ostium.
Kissing Balloon Inflation
- The combined size of the two balloons inflated simultaneously can be calculated using Finet's law: LM final stent diameter = (balloon 1 diameter + balloon 2 diameter) x 2/3.
- Accurate balloon sizing is important.
- KBI corrects underexpansion and malapposition in the main branch (LM).
- Regains central position of the carina.
- Reduces late-loss and restenosis at the side branch (LCx) and the need for target lesion revascularization.
- Reduces incidence of incomplete stent apposition.
POT-side-POT
- This strategy can be performed as an alternative to simultaneous KBI in the one-stent approach.
- POT is initially performed using a short NC or semicompliant balloon after main branch (LM) stenting.
- Wire exchange is then performed, followed by side branch (LCx) dilation with a NC or semicompliant balloon.
- Final/second POT is then performed with the same NC or semicompliant balloon as the first POT.
Case Wrap-Up
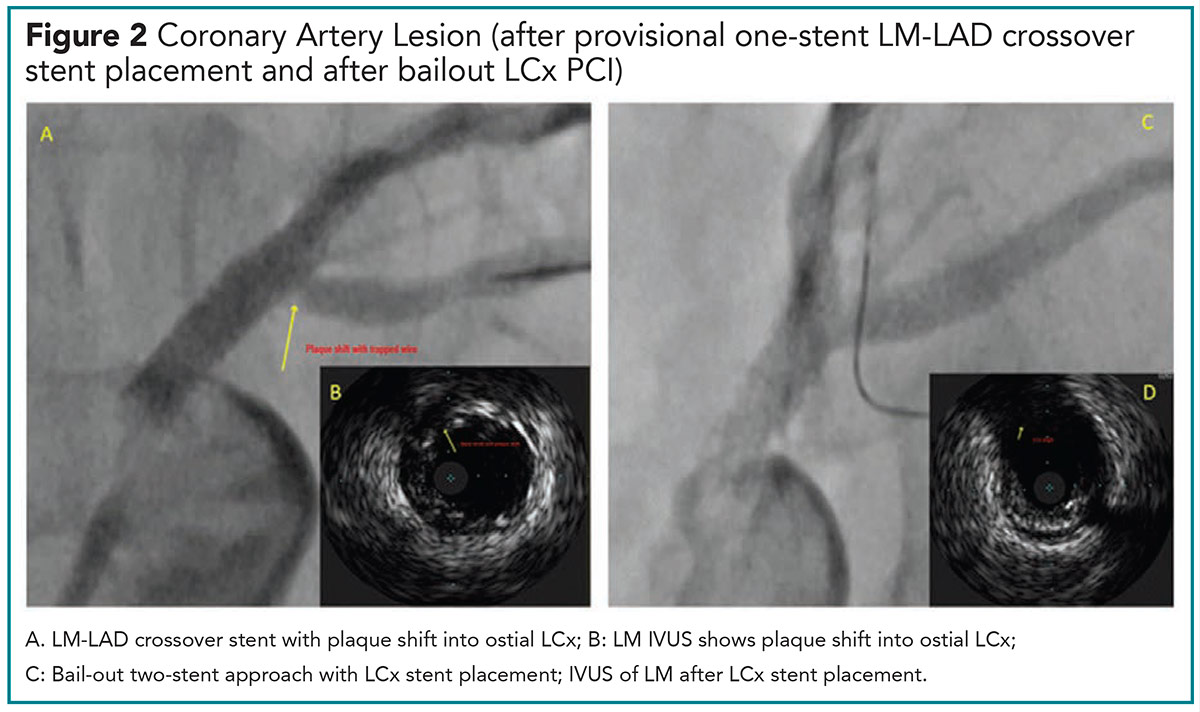
For our patient, a provisional one-stent approach was used. Using a 3.0 mm balloon, the LM-proximal LAD was predilated and a 3.5 x 24 mm DES deployed across the ostial LM into the proximal LAD lesion. A NC 4.0 mm balloon was used for POT of the LM portion of the stent. IVUS revealed a well expanded stent in the LAD, stent malapposition in the LM and plaque shift in the ostial LCx. Given these findings, a two-stent bail-out strategy of the LCx was performed with a 3.0 x 16 mm DES stent deployed in the LCx (Figure 2).
Left Main Bifurcation Stenting: Tips and Tricks
Left Circumflex Artery Wiring Techniques9,13,14
- A workhorse or polymer-jacketed guidewire should be used for trapping/jailing the wire.
- Wire the more difficult vessel first – LM artery or LCx, to reduce the risk of wire twisting around a previously placed guidewire (wire wrap).
- Guidewire tip: four basic curves: single bend with short tip (2-3 mm); single bend with long tip (4 -6 mm); single wide bend (preferred if main artery wire is to be used for LCx rewiring); and double bend shape.
- For wide carina angles, a wide smooth bend or double bend tip (for more severe side branch stenoses).
- Antegrade wiring: advance the wire directly from the proximal LM into the LCx ostium.
- Pullback wiring: retrieve the wire from the distal LM-LAD vessel into the bifurcation and redirect into the ostial LCx. A broad smooth distal tip curve (fish hook-like bend) helps the guidewire engage the LCx during the pullback from distal LM branch (LAD) towards the ostial LCx. Gentle counterclockwise rotation is recommended to advance the guidewire in the LCx.
- Reverse wire technique: use for extreme angles (>150 degrees). Create a hairpin bend about 3-5 cm from the wire tip. Advance the guidewire with the hairpin bend into the distal main branch (LAD) vessel. Once the guidewire is in the LAD, pull the guidewire back towards the bifurcation. Once the tip of the guidewire enters the LCx, gentle counterclockwise rotation advances the wire in the LCx.
- Deflectable tip/microcatheter guidewire technique: load the guidewire onto a microcatheter with a deflectable tip. Advance the microcatheter just distal to the origin of the side branch (LCx), retract the guidewire into the microcatheter, deflect the catheter's tip toward the LCx and then advance the wire through the deflected catheter into the LCx.
- Last resort for difficult LCx wiring: perform LM artery balloon predilation. This can cause undesired plaque or carina shift. Alternatively, perform debulking techniques such as rotational atherectomy or laser.
- Balloon block and support technique: inflate a balloon about 1- 2 mm from the carina in the distal main branch (LAD).15 The balloon inflation helps advance the guidewire into the LCx. Balloon to LAD diameter ratio should be 1:1. Balloon inflation should be low pressure (8-10 atm). Balloon is deflated once guidewire reaches the mid-LCx.
Left Circumflex Rewiring After LM Stent Implant13
- Goal is to recross from a distal stent strut of the LM stent as this is associated with improved ostial scaffolding and outcomes.
- The LCx could be rewired with the LM guidewire before removing the jailed LCx wire, the jailed side branch wire retracted from the LCx and redirected into the LM–LAD vessel. Alternatively, a third wire could be used if it is important to keep the main branch wire in situ.
- Pullback rewiring technique is preferred to access the distal stent cells.
- A guidewire with a wide curve allows the wire to slide across the LM-LAD stent struts during pullback and protrude into the LCx once it is reached.
- Long tips and wide curves facilitate LCx access.
- To avoid using a third wire, pre-shape the distal tip of the left main wire to match the angulation of the LCx and the diameter of the LM, i.e., primary and secondary curves.
- An underexpanded stent in the LM can hinder recrossing into the left main. Hence POT should routinely be performed to aid rewiring.
Bifurcation Definitions
One-stent technique (provisional approach or inverted provisional approach) refers to implantation of one stent in the main branch (from the LM into the LAD in our case) and balloon dilation/stenting performed in the side branch (LCx in our case) only if indicated.16
Two-stent technique refers to an intentional (upfront) decision to stent both the main branch (LM-LAD) and side branch (LCx). Crossover stenting refers to stent implantation from the main branch (LM) across the ostium of the side branch (LCx) and usually refers to LM-to-LAD stent placement. Bifurcation angles are defined as "A," the angle between the LM and the LCx artery; "B," the angle between the LAD and LCx (bifurcation angle); and "C," the angle between the LM and LAD.17
References
- Latib A, Colombo A. Bifurcation disease: what do we know, what should we do? JACC Cardiovasc Interv,2008;1:218-26.
- Chen SL, Sheiban I, Xu B, et al. Impact of the complexity of bifurcation lesions treated with drug-eluting stents: the DEFINITION study (Definitions and impact of complEx biFurcation lesIons on clinical outcomes after percutaNeous coronary IntervenTIOn using drug-eluting steNts). JACC Cardiovasc Interv 2014;7:1266-76.
- Lassen JF, Burzotta F, Banning AP, et al. Percutaneous coronary intervention for the left main stem and other bifurcation lesions: 12th consensus document from the European Bifurcation Club. EuroIntervention 2018;13:1540-53.
- Burzotta F, Lassen JF, Lefevre T, et al. Percutaneous coronary intervention for bifurcation coronary lesions: the 15(th) consensus document from the European Bifurcation Club. EuroIntervention 2021;16:1307-17.
- Kang SJ, Mintz GS, OH J-K, et al. Intravascular ultrasound assessment of distal left main bifurcation disease: the importance of the polygon of confluence of the left main, left anterior descending, and left circumflex arteries. Catheter Cardiovasc Interv 2013;82:737-45.
- Godino C, Al-Lamee R, La Rosa C, et al. Coronary left main and non-left main bifurcation angles: how are the angles modified by different bifurcation stenting techniques? J Interv Cardiol 2010;23:382-93.
- Kang SJ, Ahn J-M, Song H, et al. Comprehensive intravascular ultrasound assessment of stent area and its impact on restenosis and adverse cardiac events in 403 patients with unprotected left main disease. Circ Cardiovasc Interv 2011;4:562-9.
- Chen S-L, Zhang J-J, Han Y, et al. Double kissing crush versus provisional stenting for left main distal bifurcation lesions: DKCRUSH-V Randomized Trial. J Am Coll Cardiol 2017;70:2605-17.
- Hall AB, Chavez I, Garcia S, et al. Double kissing crush bifurcation stenting: step-by-step troubleshooting. EuroIntervention 2021;17:e317-e325.
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J 2019;40:87-165.
- Hildick-Smith D, Egred M, Banning A, et al. The European bifurcation club Left Main Coronary Stent study: a randomized comparison of stepwise provisional vs. systematic dual stenting strategies (EBC MAIN). Eur Heart J 2021;42:3829-39.
- Stankovic G, Milasinovic D. Standardisation of techniques for bifurcation stenting optimisation: the journey continues. EuroIntervention 2021;17:701-2.
- Burzotta F, De Vita M, Sgueglia G, et al. How to solve difficult side branch access. EuroIntervention 2010;6 Suppl J:J72-80.
- Burzotta F, Lassen JF, Banning AO, et al. Percutaneous coronary intervention in left main coronary artery disease: the 13th consensus document from the European Bifurcation Club. EuroInterention 2018;14:112-20.
- Li L, Liu J, Jin Q, Chen S. Case report of a novel maneuver to facilitate wire access to the side branch in bifurcation intervention - balloon block and support technique. Medicine (Baltimore) 2018;97:e9673.
- Burzotta F, Lassen JF, Louvard Y, et al. European Bifurcation Club white paper on stenting techniques for patients with bifurcated coronary artery lesions. Catheter Cardiovasc Interv 2020; 96:1067-79.
- Louvard, Y., et al. Classification of coronary artery bifurcation lesions and treatments: time for a consensus! Catheter Cardiovasc Interv 2008;71;175-83.

This article was authored by Nkechi Ijioma, MD, FACC, senior associate consultant cardiologist with the Mayo Clinic Health System in La Crosse, WI. She acknowledges and appreciates the expert content review by Jose Emilio Exaire, MD, FACC, at Mayo Clinic; Emmanouil S. Brilakis, MD, PhD, FACC, at Minneapolis Heart Institute; Kwan S. Lee, MD, FACC, at the University of Arizona, Tucson; and S. Michael Gharacholou, MD, FACC, at Mayo Clinic.
Keywords: ACC Publications, Cardiology Magazine
< Back to Listings