Feature | Cardio-Obstetrics: Insights From JACC Focus Seminar
Maternal mortality rates have been increasing in the U.S. for several decades and are among the highest seen in the developed world. The rates are highest in non-Hispanic Black women (41.7 deaths/100,00 live births) and lowest in non-Hispanic White women (13.4/100,000) and Hispanic or Latino women (11.6/100,000). The causes of pregnancy-related death are myriad, but cardiovascular disease tops the list.
"To save women's lives, we need to have a team approach to caring for pregnant and postpartum patients, to screen all pregnant and postpartum patients for cardiovascular disease and to learn to distinguish cardiovascular signs and symptoms from normal symptoms of pregnancy," says Janet Wei, MD, FACC, from Cedars-Sinai Smidt Heart Institute and Barbra Streisand Women's Heart Center in Los Angeles.
"We have recognized and studied this issue for years. It's now finally gaining more awareness in the cardiology community in the U.S.," adds Wei. "We now have scientific statements from the American Heart Association and the Focus Seminar series from the ACC. But we still need to collaborate with our colleagues in internal medicine, family practice, emergency medicine and anesthesiology to increase awareness."
In response to this connection between cardiovascular disease and maternal morbidity and mortality, calls for cardio-obstetric models of care and improved competencies have emerged. A recent issue of the Journal of the American College of Cardiology (JACC), in collaboration with ACC's Cardiovascular Disease in Committee and the Cardio-Obstetrics Work Group, published a five-part Focus Seminar that addresses a wide breadth of topics in this emerging field.
Cardio-obstetrics has emerged as a specialty in response to the rising rates of maternal morbidity and mortality related to cardiovascular disease during pregnancy.1 The field is multidisciplinary and focused on women from preconception through the postpartum period. The goal is to better evaluate and counsel women of childbearing age with or at risk for cardiovascular disease regarding maternal and fetal risks of pregnancy, to optimize medical intervention, and to provide appropriate contraception advice.
Postpartum care is an integral part of cardio-obstetric patient management. The "fourth trimester" refers to the 12 weeks after delivery and is a key time to identify any potential postpartum complications, including those related to mental health, and address contraception and cardiovascular risk factors. Included in this care should be women with adverse pregnancy outcomes that may be at increased risk of long-term cardiovascular disease and should receive appropriate education and longitudinal follow-up.
Q&A With Melinda B. Davis, MD, FACC, University of Michigan, Ann Arbor
How long has cardio-obstetrics existed as a subspecialty?
Much of the attention on heart disease during pregnancy has previously focused on women with congenital heart disease. While this remains an important area, more and more women with acquired heart disease and other cardiovascular risk factors are also becoming pregnant and require specialized attention. The terminology "cardio-obstetrics" has only been coined and widely recognized within the past few years (similar with the growing field of cardio-oncology).
Any thoughts of making it a fellowship?
Dedicated subspecialty fellowship training programs for cardio-obstetrics do not currently exist, but there is increasing recognition that exposure to the topic is important during cardiology fellowship training.
Who should be part of the cardio-obstetrics team?
Any cardiologist with interest and passion for caring for this patient population can be involved. Multidisciplinary teamwork is very important. Managing complex patients during pregnancy requires doctors with expertise in pregnancy as well as in particular conditions – congenital heart disease, valvular disease, aortic disease and cardiomyopathy.
Medical and surgical advances in the management of pediatric heart disease now permit survival of most women born with congenital heart disease (CHD), but pregnancy may be poorly tolerated by these women.2 CHD is the most common cardiovascular condition encountered during pregnancy. Yet, most women with CHD can be safely managed through pregnancy with a team-based approach.
Identification and risk stratification of women at highest risk from pregnancy and during pregnancy are important to optimize maternal and fetal outcomes. The section provides practical guidance from preconception through postpartum for cardiovascular conditions that are predominantly congenital or heritable in nature, including aortopathies, CHD, pulmonary hypertension and valvular heart disease. Long-acting reversible contraception is safe and effective for patients with congenital and heritable cardiovascular conditions.
Q&A With Katherine J. Lindley, MD, FACC, Washington University School of Medicine, St. Louis, MO
About what proportion of women with CHD need to avoid pregnancy?
It is really the minority of women with congenital or heritable disorders who should completely avoid pregnancy – namely those with pulmonary arterial hypertension, severe aortic or mitral stenosis, and severe ventricular dysfunction or Fontan failure. Importantly, preconception evaluation can allow for recognition of these high-risk features to avoid exceedingly high-risk pregnancies.
Is the concern that women with CHD or a heritable disorder become pregnant, or that they are afraid of getting pregnant?
It is absolutely not a problem that women with CHD are having pregnancies – the value of a cardio-obstetrics team is to facilitate healthy pregnancies for mom and baby. Problems primarily arise when women have not been properly evaluated by an adult CHD/cardio-obstetrics specialist, and it is not recognized that they are at increased risk for cardiovascular complications. Many women have also been inappropriately told that they should avoid pregnancy when, in fact, they are expected to be able to safely undergo pregnancy with the right team caring for them.
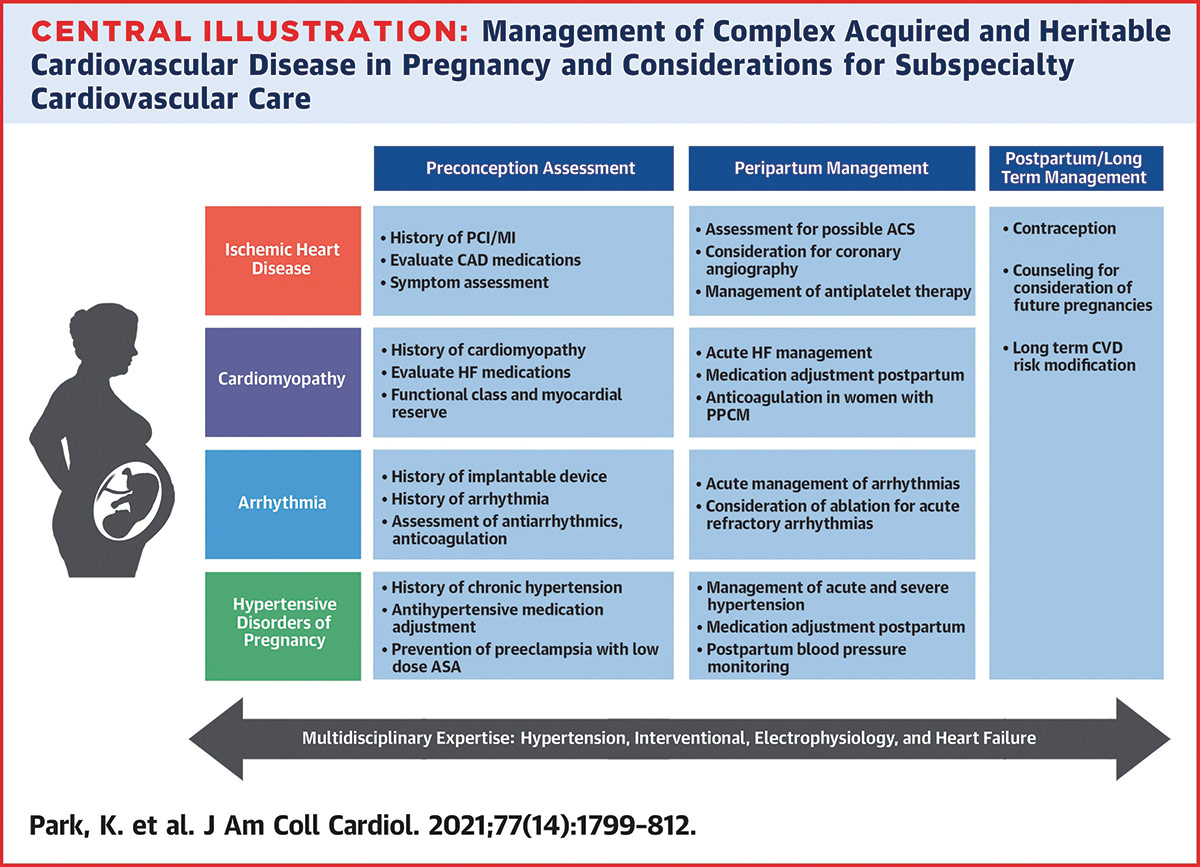
Acquired cardiovascular conditions, including arrhythmias, cardiomyopathies, hypertensive disorders and ischemic heart disease, are a leading cause of maternal morbidity and mortality.3 As the average age of childbearing rises, the prevalence of acute coronary syndromes, cardiomyopathy and other cardiovascular complications in pregnancy are also expected to increase.
Interdisciplinary care is critical to managing complex acquired and pre-existing cardiovascular disease in pregnant women. Preservation of maternal stability during pregnancy is important for optimizing fetal health. In this third part of the series, Park, et al., provide guidance on the management of acquired arrhythmias and acute management of tachyarrhythmias during pregnancy, hypertrophic cardiomyopathy, hypertension, ischemic heart disease and other conditions from preconception through delivery and the postpartum period.
Q&A With Ki Park, MD, FACC, University of Florida College of Medicine, Gainesville
What is the most important takeaway from this Focus Seminar in the series?
Acquired cardiovascular conditions are a significant contributor to maternal morbidity and mortality during pregnancy.
About what proportion of women with acquired heart disease need to avoid pregnancy?
Acquired heart disease for the most part can be managed throughout pregnancy but women with certain conditions such as severe peripartum cardiomyopathy and spontaneous coronary artery dissection (SCAD) should either avoid becoming pregnant or consult with a cardio-obstetrics specialist to discuss risks prior to conception.
It is perhaps surprising to think of pregnant women having STEMIs and ACS. How often does this happen?
ACS is rare in pregnancy. However, the overall trends in MI in pregnancy are increasing and SCAD accounts for a significant proportion of MI in pregnancy.
Women of child-bearing age have historically been underrepresented in clinical research, leaving knowledge gaps in the cardiovascular care of pregnant and lactating women.4 Pregnant women represent a complex population when considering the use of noninvasive imaging and therapeutics. To avoid radiation exposure, ultrasound and MR without gadolinium-based contrast are preferred over other imaging modalities for pregnant women. If imaging with ionizing radiation is necessary, strategies to minimize exposure should be employed. Most drugs given to a mother will cross the placenta. Fetal drug concentration may be similar with, higher than, or lower than the maternal concentration. This part of the Focus Seminar provides evidence-based recommendations regarding the use of common cardiovascular diagnostic tests and medications in pregnant and lactating women.
Q&A with Natalie A. Bello, MD, MPH, FACC, Columbia University Irving Medical Center, NY
What is the key takeaway for readers from this article?
In all situations involving a pregnant or lactating patient, the best test to diagnose a potential maternal condition should be utilized to optimize the health of both mother and fetus/baby. This can often be done without ionizing radiation. But in situations where radiation exposure is unavoidable in pregnancy, dose modification strategies should be undertaken, and consultation with a radiology or imaging specialist should be sought.
When you say pregnant women are a complex population but not a vulnerable one, what does this mean?
This is how the National Institutes of Health recommends we refer to pregnant women in research – as complex, not vulnerable. Vulnerable populations are ones that cannot protect their interests and/or provide informed consent. This is not true across the board for pregnant women. Most pregnant women have the same capacity for autonomous decision-making as when they were not pregnant or as other non-pregnant women or as men. Thus, they are capable of making a decision to participate or decline participation in appropriate research studies while pregnant. Performing research that includes pregnant women is scientifically complex because of the remarkable physiologic changes that occur, as well as the ethical complexity of balancing the potential risks and benefits of both mother and fetus. When interests align, this can be easy. But if they diverge, then the inclusion of pregnant women is more complex.
Disease-specific contraceptive safety and effectiveness is imperative in preventing unplanned pregnancies in women at high-risk with cardiovascular disease.5 This final part of the five-part series reviews the evidence and provides recommendations regarding contraceptive options for younger women with CHD and women with, or at high risk for, cardiovascular disease. The article also discusses recommendations regarding pregnancy termination for women at excessive cardiovascular mortality risk due to pregnancy.
Q&A with Kathryn J. Lindley, MD, FACC, Washington University School of Medicine, St. Louis, MO
Are there certain contraceptive options that are better or worse for women with CHD? Or is it about effectiveness and compliance?
The long-acting reversible contraceptives (IUD and subdermal implant) are really the optimal contraceptive options for women with either congenital or acquired heart conditions. They are both safe for all cardiovascular conditions as well as highly effective – with effectiveness rates comparable to tubal ligation. However, they are completely reversible, allowing women at high risk to effectively plan their pregnancies and optimize their heart health prior to pregnancy. These contraceptive options do not increase the risk of thrombosis, hypertension, MI or stroke. And they also often improve menorrhagia for women who require antiplatelet or anticoagulation therapy.
What is the message for cardiologists regarding contraception and reproductive planning considering this isn't typically their domain?
Contraception counseling should be a routine, integral part of standard cardiovascular care for women of childbearing age. Pregnancy potentially carries significant risk to women with underlying cardiovascular disease, and we routinely prescribe medications that are potentially teratogenic. It is important for cardiologists to recognize the importance of having this discussion with their patients and to have a good understanding of the safety and efficacy of the available methods of contraception so that they may provide accurate counseling. I also think that cardiologists should be comfortable prescribing hormonal contraceptives and/or emergency contraception to young women with cardiovascular conditions. It is really preventive cardiovascular care for this population, just as is the treatment of diabetes, hypertension or dyslipidemia.
References
- Davis MB, Arendt K, Bello NA, et al. Cardio-Obstetrics Part 1: Team-Based care of women with cardiovascular disease from pre-conception through pregnancy and postpartum: JACC Focus Seminar 1/5. J Am Coll Cardiol 2021;77:1763-77.
- Lindley KJ, Bairey Merz CN, Asgar AW, et al. Management of women with congenital or inherited cardiovascular disease from pre-conception through pregnancy and postpartum: JACC Focus Seminar 2/5. J Am Coll Cardiol 2021;77:1778-89.
- Park K, Bairey Merz CN, Bello NA, et al. Management of women with acquired cardiovascular disease from pre-conception through pregnancy and postpartum: JACC Focus Seminar 3/5. J Am Coll Cardiol 2021;77:1799-1812.
- Bello NA, Bairey Merz CN, Brown H, et al. Diagnostic cardiovascular imaging and therapeutic strategies in pregnancy: JACC Focus Seminar 4/5. J Am Coll Cardiol 2021;77:1813-22.
- Lindley KJ, Bairey Merz CN, Davis MD, et al. Contraception and reproductive planning for women with cardiovascular disease: JACC Focus Seminar 5/5. J Am Coll Cardiol 2021;77:1823-34.
Clinical Topics: Acute Coronary Syndromes, Arrhythmias and Clinical EP, Cardiovascular Care Team, Congenital Heart Disease and Pediatric Cardiology, Diabetes and Cardiometabolic Disease, Heart Failure and Cardiomyopathies, Prevention, Pulmonary Hypertension and Venous Thromboembolism, Valvular Heart Disease, Vascular Medicine, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Congenital Heart Disease, CHD and Pediatrics and Arrhythmias, CHD and Pediatrics and Prevention, CHD and Pediatrics and Quality Improvement, Pulmonary Hypertension, Hypertension
Keywords: ACC Publications, Cardiology Magazine, Abortion, Induced, Acute Coronary Syndrome, Anesthesiology, Aortic Diseases, Arrhythmias, Cardiac, African Americans, Cardiomyopathies, Cardiomyopathy, Hypertrophic, Cardiovascular Diseases, Contraceptive Agents, Decision Making, Coronary Vessels, Diagnostic Tests, Routine, Dissection, Emergency Medicine, Family Practice, Fellowships and Scholarships, Fertilization, Follow-Up Studies, Gadolinium, Fetus, Goals, Heart Defects, Congenital, Hispanic Americans, Hypertension, Pulmonary, Hypertension, Pregnancy-Induced, Internal Medicine, Informed Consent, Live Birth, Lactation, Maternal Mortality, Mental Health, Mitral Valve Stenosis, Neoplasms, National Institutes of Health (U.S.), Mothers, Peripartum Period, Pharmaceutical Preparations, Postnatal Care, Postpartum Period, Pregnancy, Pregnancy, Obstetrics, Placenta, Pregnancy Outcome, Pregnancy, High-Risk, Pregnancy, High-Risk, Pregnant Women, Prevalence, Pregnancy, Unplanned, Radiation, Ionizing, Radiology, Referral and Consultation, Risk Assessment, Risk Factors, Sterilization, Tubal, Tachycardia, Thrombosis, Ventricular Dysfunction, Stroke, Vulnerable Populations, Universities
< Back to Listings