Cutting-Edge Structural Interventions | Building A Structural Program: Doing Your Homework

In my youth I was blessed to spend a lot of time with my father in his cardiac catherization (cath) lab. It was amazing what could be done percutaneously even 20 years ago: fixing people with heart attacks and helping improve blood flow to various limbs. I'd sit in the control room, feet dangling high off the floor, eating cookies while watching the black and white screens as one of the lab technologists would explain what was happening. Most of these procedures required the placement of balloons and stents over an artfully placed wire. But I never imagined that one day I would be implanting heart valves and moving objects inside the heart in 3D – off a wire!
The field of structural cardiology captivated me early in my medical training and I've dedicated my career to learning about the field and playing my part to ensure all patients have access to these burgeoning technologies.
Leadership Academy: Building For Tomorrow
ACC's Leadership Academy has a singular goal: to grow the College's leaders of tomorrow by developing early career leaders today.
The two-year, cohort-based program is open to cardiovascular professionals within the first seven years after the completion of their specialty education, residency or training. Participants are selected by an ACC member-led committee and participate in a comprehensive curriculum addressing topics ranging from critical leadership skills needed in today's health care environment to leading effectively within their respective institutions and within the ACC.
The program's second phase pairs young leaders with an ACC member mentor for a capstone project that meaningfully tackles real-world problems while also aligning with one or more of the College's strategic objective.
To date, more than 70 Leadership Academy participants have gone on to serve in leadership roles within the College, including on the ACC Board of Governors and as part of Section, Council and Chapter leadership.
Click here to read about the members of Cohort III and their capstone projects that will help to transform cardiovascular practice and improve heart health.
As I moved through my two-year fellowship at the University of Washington, I was fortunate to be able to impact patients' lives and see firsthand the difference possible with structural procedures. Now hooked, I've focused on bringing this technology to more patients nationwide and striving to eliminate some of the disparities when it comes to accessing this technology.
As the director of the structural heart program in a rural community hospital, I'm acutely aware of the disparities experienced by my patients because they live in a region with a low population density.1,2 My goal is to bring world-class care to my community in Appalachia. Early on I realized I needed more than just passion and motivation. I needed a business plan.
Despite our extensive medical training, there's no training for fellows in training on how to build a medical program. While I received valuable business advice from many mentors along the way, unlike my highly structured medical training, I had no idea how to systematically grow and build on an existing program. When I accepted my current position, colleagues and mentors emailed documents to me from the Advisory Board. But I found these 50+ page documents, despite their meticulous detail, were devoid of practical information. I had no idea where to start and often felt discouraged. I failed many times and made many faux pas along the way. But just like a baby learning to walk, I refused to accept failure and kept going.
Fortunately, I was part of ACC's Leadership Academy Cohort II and had the opportunity to learn from both an amazing peer group and leaders in the field, including John Gordon Harold, MD, MACC, who provided key lessons and mentorship. ACC's Rosanne Nelson armed us with powerful leadership tools including how to become an influential leader and how to lead through change.
The genesis of this article was numerous conversations with colleagues that made it clear that my lack of knowledge for starting a structural heart program was more the rule than the exception. As a disclaimer, this article reflects my humble opinions and represents but one way to skin the proverbial cat and is the first in a series. The focus will be three procedures: TAVR, transcatheter edge-to-edge repair (TEER) and left atrial appendage occlusion (LAAO).
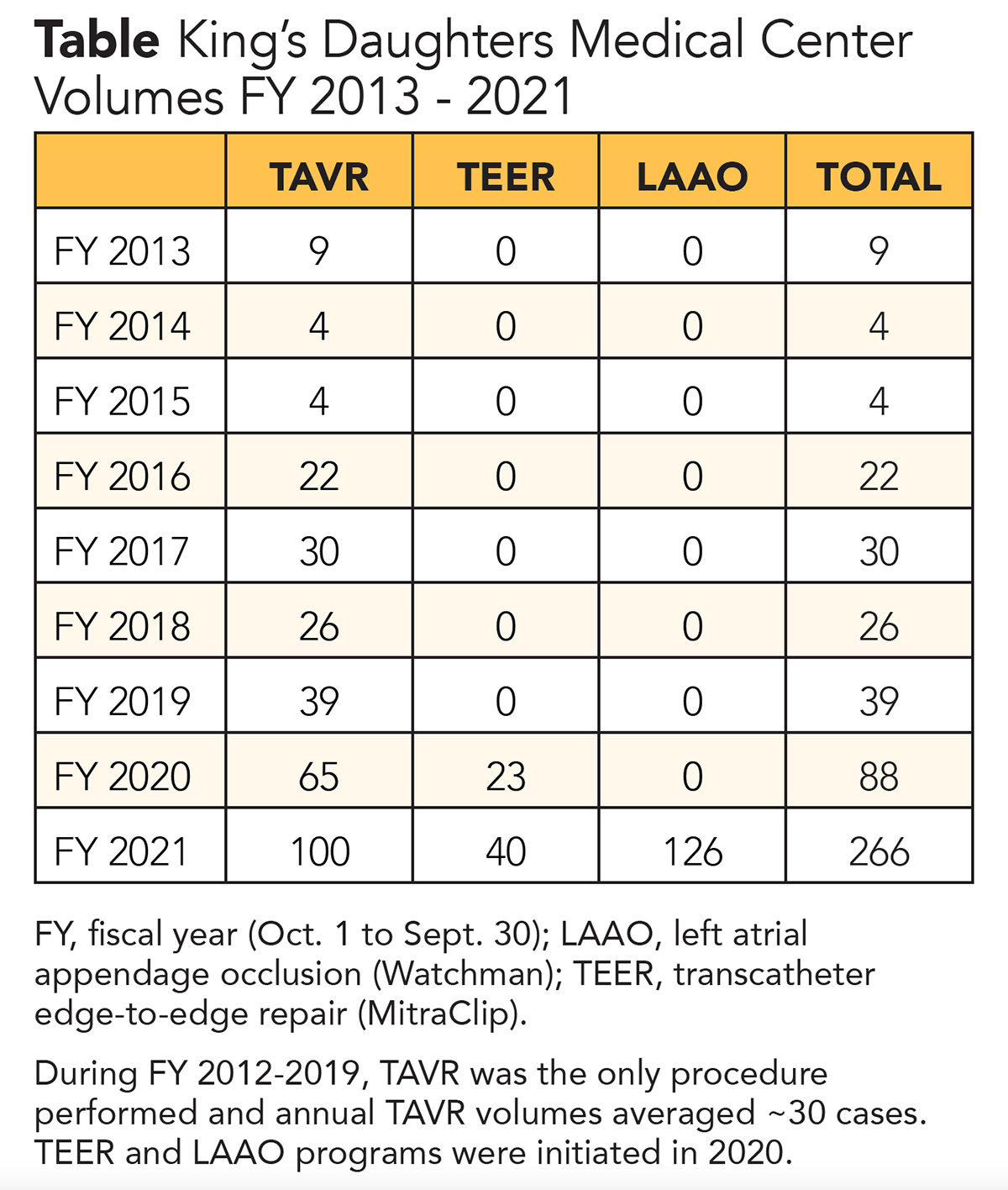
At King's Daughters Medical Center (KDMC), we have experienced tremendous growth over the past three years. The Table lists volumes for these three common structural procedures which form the building blocks for a structural program. Our program started in 2012 with TAVR and our annual TAVR volume through 2019 was approximately 30-40 cases. All TAVR cases were performed in the operating room under general anesthesia with transesophageal echocardiography (TEE) guidance. Only balloon-expandable valves were available and the alternative access site was usually transapical.
Beginning in 2020, we began to perform the majority of TAVR cases in the cath lab under conscious sedation using both self-expanding and balloon-expandable valves. Alternative access is selected in consultation with peripheral vascular colleagues: a combination of percutaneous and surgical cut down techniques are used.
This success of KDMC's Structural Heart Program is due to the success of the entire cardiovascular team, which will be a common thread in this series. Each specialist and team member from sonographer to surgeon to hospital administrator must work together in harmony to achieve the goals we set.
Building Blocks of a Program
Growth and change always involves working with a strong team and respecting everyone's expertise and views. Our trajectory is a powerful example of how alignment between administration and physicians can fuel growth of any cardiac program. My goal is to share these building blocks to help others on this journey avoid many of my blunders and missteps and be more confident in formulating a plan to lead change. I'm confident that if we can increase access to care in rural Appalachia to this magnitude, it can be done anywhere.
Step 1: Visit other programs in the same "class"
I reached out to program leaders at high volume, successful community structural programs across the U.S. I'd met early in my career. This led to visits with Mir Wail Hashimi, MD, FACC, in Mobile, AL, who helped build a high-volume program within a private practice model. I met with the president of the Arkansas Heart Hospital, Drew Jackson, who helped craft a high-quality and cost-efficient structural program in a nonteaching community integrated hospital. These visits to two completely different programs gifted me with some practical ideas I employed as I started my own journey.
Seek out a well-established program and leaders in the same type of setting for your own potential program to serve as a model, whether it's an integrated community hospital or a private practice, etc. Every model comes with its own predefined challenges. If you work in a private practice setting at three hospitals, it may be inherently more challenging to gain alignment with any particular hospital administration.
Step 2: Learn the geography of your practice
KDMC is in a very rural area in eastern Kentucky. I knew that despite the low population density, it's the only tertiary center capable of doing structural procedures in about a 100-mile radius. I also knew the health system had at least half a million patients in its catchment area and there was a very low penetration of valvular heart disease therapies. Many of our patients drive up to two hours, even from other states, including western West Virginia and southern Ohio, as well as southeastern Kentucky.
I also studied the neighboring programs to better understand their catchment areas and services offered. I wanted to ensure that I would partner with these programs to help all patients in the area – not waste time competing with them.
Step 3: Understand your patient population
When I heard of the paucity of tertiary care centers over such a broad swath of land, I recognized the need for a strong structural program in the area to improve access to care. However, one thing I did not recognize was the lack of connectivity overall in Appalachia. This is one of the areas that's being referred to when politicians and policy makers talk about improving broadband access. (See the cover story for more on digital equity.) When I first moved here in 2019, I was shocked to see how many people still use flip phones and don't have access to the internet. Now I totally understand when I ask a patient for their phone number and learn they do not have a phone. Notably, this lack of access to basic health information makes patient education very difficult.
I have relied heavily on resources on ACC's CardioSmart.org website and YouTube videos to help my patients understand their valvular heart disease process as well as the options available for treatment. I have also devised different analogies and diagrams to explain these concepts to patients. Many are familiar with farming or engine mechanics, so we try to use those examples when explaining the pathophysiology of mitral regurgitation, for instance. Shared decision-making is my personal mantra. I do my best to ensure patients and their families have all the information they need to make a well-informed decision between medical therapy, surgery and percutaneous therapy.
Step 4: Understand the internal politics
Relationships within the home institution are the main reason structural programs are either incredibly successful or fail to grow. These relationships include how cardiologists interact with each other and the cardiac surgeons. What do the cardiac surgeons think of the field of structural heart disease? Are they supportive or skeptical? Are the cardiologists more aggressive with early diagnosis and referral or do they tend to refer patients later in the disease process? Are there any opportunities for education on ACC/AHA guidelines? Relationships between physicians and hospital administration is equally vital. How accessible are the administrators? Do they meet regularly with physicians?
Step 5: Get to know your industry partners
Industry can be vital in your quest to grow your program. Device manufacturers have additional resources at their disposal, both monetary and educational, to help you grow as a clinician and a leader. They can connect you with other leaders in the field from around the country and can also support educational events locally to raise awareness about structural heart disease. They have a wealth of resources to help educate your patients and referring providers.
However, try not to be biased. If you trained with a particular device but there is more than one option on the market, consider ensuring your program has access to both products. This can help protect your program in case of a supply chain issue, but also demonstrates you are willing to grow and that your top concern is offering the best care with the latest devices. And you want to model good behavior for the rest of your program – selecting one particular device every time without taking into account individual patient characteristics can potentially send the wrong message to your colleagues.
Step 6: Align your vision with your organization's vision
You may be the smartest person in the room and the best proceduralist in the country, but if your organization's administration is not supportive of starting a particular procedure, it's unlikely you'll get to do it (at least at that facility). Whether you work at one hospital or several around town, take a moment to make sure your goals are consistent with those of the health care system(s) at which you practice. No alignment = no achievements.
On the flip side, with good alignment, the possibilities are endless. In business, I believe that creating opportunities for win-win-win-win situations is the key to success. Patients win, providers win, health care systems win, industry wins. Maximize these opportunities and growth will ensue.

This article was authored by Sandeep Krishnan, MD, RPVI, FACC, an interventional and structural cardiologist and director of Structural Heart Disease at the King's Daughters Medical Center in Ashland, KY.
Do you have a topic or question to be addressed in this series? Tweet the author @SKrishnanMD or email him at xsandeepx@gmail.com. Thank you.
References
- Marquis-Gravel G, Stebbins A, Kosinski AS, et al., Geographic access to transcatheter aortic valve replacement centers in the united states: insights from the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry. JAMA Cardiol 2020;5:1006-10.
- Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health 2013;38:976-93.
Clinical Topics: Cardiac Surgery, Cardiovascular Care Team, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Valvular Heart Disease, Cardiac Surgery and VHD, Interventions and Imaging, Interventions and Structural Heart Disease, Echocardiography/Ultrasound, Mitral Regurgitation
Keywords: ACC Publications, Cardiology Magazine, Administrative Personnel, Agriculture, Anesthesia, General, Arkansas, Atrial Appendage, Cardiologists, Cardiology, Conscious Sedation, Decision Making, Shared, Early Diagnosis, Echocardiography, Transesophageal, Electronic Mail, Fathers, Fellowships and Scholarships, Goals, Health Services Accessibility, Heart Valve Prosthesis, Heart Valves, Hospital Administration, Hospital Administrators, Hospitals, Community, Internet, Kentucky, Leadership, Learning, Mentors, Mitral Valve Insufficiency, Motivation, Myocardial Infarction, Nuclear Family, Ohio, Operating Rooms, Peer Group, Population Density, Private Practice, Radius, Referral and Consultation, Stents, Surgeons, Technology, Tertiary Care Centers, Transcatheter Aortic Valve Replacement
< Back to Listings


