Feature | Racial, Ethnic Disparities in CV Care: Focused JACC Series

A new nine-part focus seminar series in the Journal of the American College of Cardiology, looks at how race and ethnicity impact multiple facets of cardiovascular care, including hypertension management, diabetes and obesity, heart failure (HF), atrial fibrillation, quality of care and more.
"This JACC Focus Seminar Series provides narrative assessments of where we are today in nine cardiovascular conditions and shares insights on how we chart the path forward for addressing related health disparities," says George A. Mensah, MD, FACC, and JACC Editor-in-Chief Valentin Fuster, MD, PhD, MACC, in an accompanying introduction article. "A common theme throughout this seminar series is the importance of social determinants of health (SDOH) as a root cause of the observed racial and ethnic disparities. Taking action to pave the way for health equity in cardiology is important."
Throughout the series, the researchers note that implementation of proven strategies such as team-based care and an active fostering of positive partnerships between clinicians and patients are essential for underserved racial and ethnic minority groups. Other themes highlighted throughout the series include access to adequate and timely diagnoses and treatments, increasing diversity in clinical trials, access to proper health insurance coverage and the need for social justice approaches to health care.
Equity-Centered Roadmap For Reducing Disparities, Improving Quality of Care
Recent research suggests that health equity for all racial and ethnic groups will not be achieved without an approach to quality measurement and improvement that acknowledges systemic racism at multiple levels and uses the methods and tools of QI to dismantle systemic racism in health care," according to a review on race, ethnicity and heart disease.
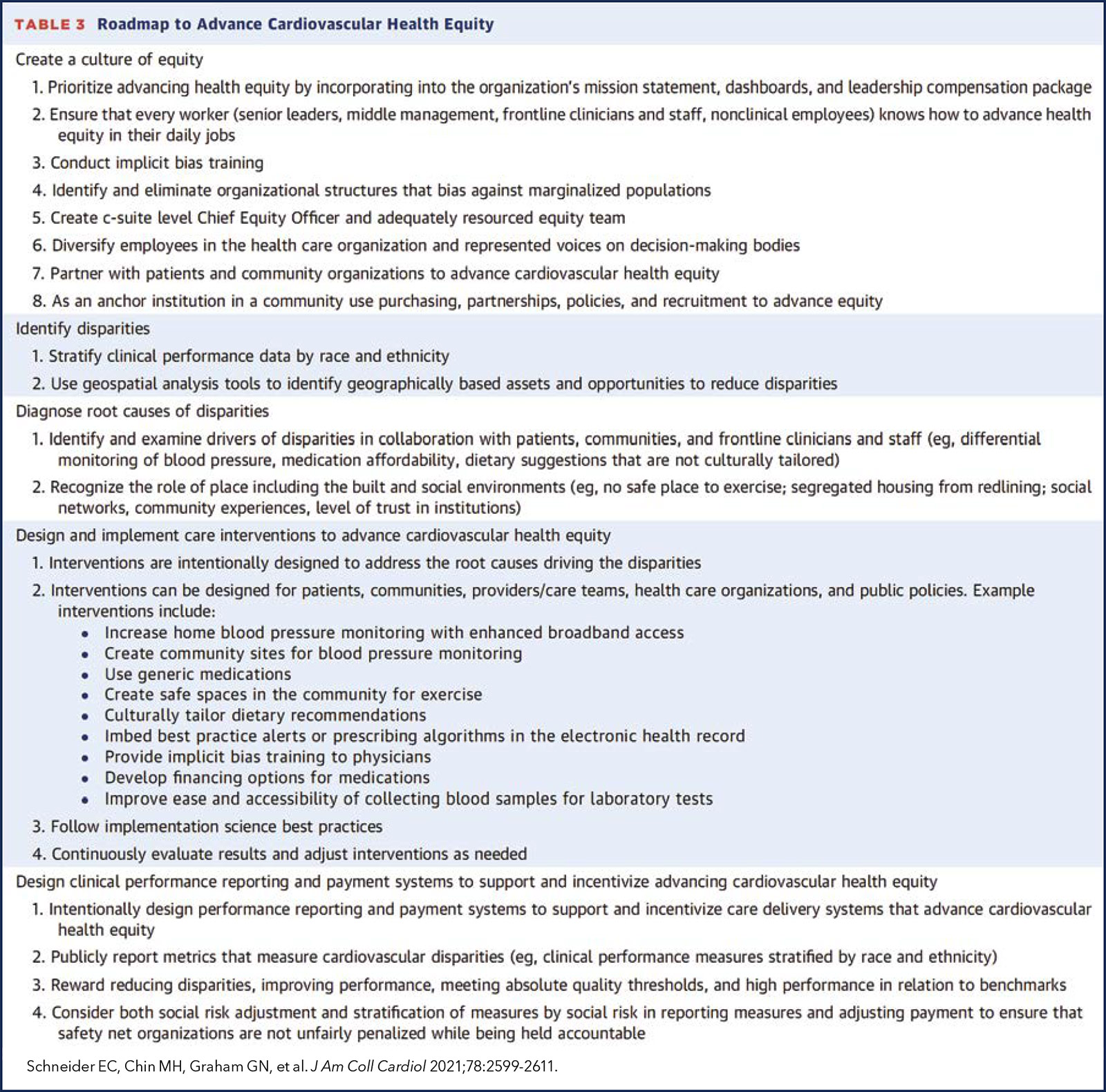
Eric C. Schneider, MD, FACC, Marshall H. Chin, MD, FACC, et al., provide a summary of racial and ethnic disparities in the quality of cardiovascular care and offer an approach for diagnosing and intervening on health equity factors in the form of the "Equity-Centered Quality Improvement Model and Roadmap to Advance Cardiovascular Health."
While strides have been made in reducing racial and ethnic disparities in cardiovascular disease, these disparities have not been eliminated and "may be increasing again, reversing earlier gains," due to factors like structural racism, according to Schneider, Chin and colleagues. They outline the importance of understanding the complex web of factors contributing to racial and ethnic disparities, including clinical risk factors, genetics and, more importantly, social and economic conditions. They also stress that "current quality and safety improvement programs may be more effective if interventions are designed to address the drivers of inequitable health outcomes both within and outside of health care."
Enter the Roadmap to Advance Cardiovascular Health (Figure). The Roadmap provides "practical guidance to improve the measurement and analysis of quality problems and the implementation of care interventions and policies that reduce racial and ethnic disparities in outcomes," says Schneider, Chin, et al. "Setting explicit organizational goals for equity should reflect emerging understandings of structural racism and engage people from local communities. Policymakers, payers, and accreditors must align financial incentives to reward those who tackle this insidious problem. Change is possible. Seizing the equity initiative today will offer hope to future generations and accelerate further reductions in CVD morbidity and mortality."
Solutions For Increasing Health Equity Among Patients With Diabetes, Obesity
Implementing equity-focused strategies targeted at racial and ethnic minority groups disproportionately burdened by diabetes and obesity are critical to preventing and managing these conditions and decreasing risks of cardiovascular disease and adverse clinical outcomes, according to Prakash Deedwania, MD, FACC, et al.
Obesity and type 2 diabetes are highly prevalent and increasing in the U.S. among racial/ethnic minority groups including African American, Hispanic/Latinx American and Asian American populations. They note "pervasive disparities exist at every level from risk factors through outcomes." For example, they highlight documented disparities in hemoglobin A1c control, lower prescription rates of newer hyperglycemic medications along with greater rates of complications post-bariatric surgery.
Several best practices are outlined to address cardiometabolic disparities within clinical guidelines, as well as recommendations for cross-cutting strategies to advance health equity within these patient populations. Specifically, Deedwania, et al., stress the importance of addressing social needs and SDOH in future guidelines and underscore the importance of providing culturally tailored and linguistically appropriate care. The use of community health care workers "as bridges between their ethnic, cultural, or geographic communities and health care providers" is also encouraged, as are "aggressive measures to enhance participation of underrepresented racial and ethnic minority groups" in all aspects of clinical trials.
"Currently, building trust with patients, effective communication, diversity in medicine and science and patient-centered guideline-based care are cornerstones of improving diabetes and obesity care," the authors write. "Many opportunities exist to improve obesity and diabetes treatment and care for U.S. racial/ethnic minorities by keeping equity as our North Star."
Clinical Review Explores Solutions For Reducing Disparities in Hypertension
Hypertension control remains a persistent clinical problem and public health challenge, especially among certain racial/ethnic minority groups in which the prevalence is high, according to Keith C. Ferdinand MD, FACC, and colleagues. They provide an overview of racial/ethnic disparities in the epidemiology of hypertension and detail the impact of SDOH, racism and bias on the quality of cardiovascular care and outcomes.
The authors note that "racial/ethnic disparities in hypertension prevalence are well documented, especially among Black adults who are disproportionately affected and have one of the highest rates of hypertension globally." They also highlight the higher burden of CAD, heart failure, stroke, peripheral arterial disease, chronic renal disease, dementia and other complications linked to hypertension faced by certain racial/ethnic minority groups. Stark disparities in maternal outcomes, particularly among Black women, as well as COVID-19 morbidity and mortality, are also called out in the review.
Ferdinand and colleagues stress the need for "urgent action" to improve existing suboptimal hypertension control rates, including the routine consideration of SDOH in clinical assessments. They also highlight the importance of team-based care, strengthening community-based interventions and outreach and utilizing self-measured BP and telemedicine. Incorporating racial/ethnic differences in clinical guideline recommendations and the development and support for national programs targeted towards hypertension control are other approaches that need to be considered.
"We must ensure the existing disparities in clinical care are not worsened and there are continued efforts to promote equitable health care access for all," they write.
Race and Ethnicity Considerations in Patients With CAD, Stroke
Greater representation of racial and ethnic subgroups in population data and clinical trials, as well as "improved culturally congruent and competent communication about risk factors and symptoms," are needed when it comes to reducing disparities in the management and treatment of coronary artery disease (CAD) and stroke, according to a review authored by Michelle A. Albert, MD, MPH, FACC, et al.
Albert and colleagues highlight known differences across racial/ethnic populations in traditional cardiovascular risk factors like hypertension and diabetes, and call attention to the impacts of SDOH and structural racism within and outside of health care systems. However, they stress that underrepresentation of racial and ethnic minority patients and primary principal investigators in clinical trials make it difficult to have a complete and comprehensive understanding of health care disparities in CAD and stroke.
Potential strategies to improve health equity they highlight include implementation of implicit bias training and provider culturally competent and congruent engagement and training; equitable health insurance coverage; use of equitable clinical financial algorithm modeling that prioritizes SDOH; standardization of clinical care protocols that address equity concerns; increasing the percentage of main principal investigators from racial/ethnic minority groups as well as patient diversity in clinical trials; and collaborative community-centric implementation research.
"Identification of strategic opportunities to address the social and structural factors responsible for racial and ethnic disparities is imperative to achieving equitable outcomes for patients with CAD and stroke," says Albert, et al.
Race, Ethnicity Should Take Center Stage in VHD Research
Despite recognition of valvular heart disease (VHD) as a major global public health problem and marked disparities in access to diagnosis and treatment across racial and ethnic groups, "considerations of race and ethnicity have not taken center stage in VHD research," according to the paper authored by Catherine M. Otto, MD, FACC, et al.
"The past decade has seen major breakthroughs in the diagnosis and treatment of [VHD]," they write. "… However, there is mounting evidence that inequitable access to health care has systematically prevented racial and ethnic minorities from fully benefiting from these advancements."
Otto and colleagues offer a review of the differences in the etiology, diagnosis and treatment of VHD within the context of race, ethnicity and health care disparities. They also propose ideas for future research that address barriers to diagnosis and treatment among various racial and ethnic minority groups. Among their three main ideas:
- High-quality studies using representative samples of the population … to assess prevalence calcific valve disease across racial and ethnic groups";
- identifying approaches guarantee equitable access to echocardiography;
- incorporation implementation science methods into VHD research systematically identify overcome barriers medical treatment surgical transcatheter therapies among minorities.
"The current unacceptably low rates of surgical and transcatheter interventions among racial and ethnic minorities should be a call to action to put health care disparities at the forefront of VHD research and care," the authors write.
Social Interventions Needed to Improve Care, Outcomes in HCM, DCM
There is an urgent need for biomedical and social interventions to address the significant racial- and ethnicity-based disparities in clinical presentation, management and outcome of hypertrophic cardiomyopathy (HCM) and dilated cardiomyopathy (DCM), respectively, according to two separate review articles authored by Ntobeko A.B. Ntusi, MBCHB, DPHIL, MD, and Karen Sliwa, MD, PhD, FACC.
When it comes to HCM, Black patients are more likely to present with heart failure but are less commonly referred for symptom management, sudden cardiac death stratification, surgical septal myectomy, or for ICDs, all interventions that increase survival, note Ntusi and Sliwa. Additionally, Black patients with HCM have lower survival rates following hospital discharge for out-of-hospital cardiac arrest. Also of note, bystander-initiated CPR is less common when it comes to Black patients compared with White patients.
Racial segregation, lack of neighborhood walkability, racism or bias among health care workers, lack of dedicated patient education and clinical programs, limited trust in health care workers and poor linkages between health systems and communities are among the factors associated with these disparities in care related to HCM. Other SDOH like education, religious beliefs and economic status also have an impact.
Sliwa and Ntusi stress the need for targeted, multipronged and multisectoral interventions to help improve equity in care. In particular, they note the importance of enhanced patient education and greater understanding of the "drivers of race- and ethnicity-based disparities in [HCM] ... in terms of the impact on the individual, community, institution, and national realities." They also urge the use of implementation science to "support durable adoption of evidence-based interventions in Black patients and communities" that "go beyond enhancing linkages between health care systems and the communities and reduce the impact of [SDOH] on ethnicity-based disparities in [HCM] and other forms of cardiovascular disease."
Like HCM, DCM outcomes and survival rates are worse in Black patients compared with White patients. "DCM in Black patients is underrecognized and underreferred for effective therapies, a consequence of a complex interplay of social and socioeconomic factors," write Sliwa and Ntusi. They recommend the creation of multifaceted strategies to manage SDOH and urge the exploration of policy changes to expand patient access to equitable care, and provision of insurance, education and housing. They also underscore the "urgent need to prioritize a social justice approach to health care and the pursuit of health equity to eliminate race and other disparities in the management of cardiovascular disease."
Race, Ethnicity and Heart Disease: Atrial Fibrillation
"The unique importance of race and ethnicity in determining [atrial fibrillation (AFib)] risk and outcomes must be recognized and should provoke continued research," according to findings in the paper authored by Sumeet S. Chugh, MD, FACC, et al. AFib affects at least 60 million people worldwide, accounting for a substantial number of deaths and significant health care costs. Available studies suggest disparities in both treatment and outcomes between White individuals and persons of other races and ethnicities, yet the reasons for these differences and the potential impacts on outcomes are unclear due to the limited number of studies available.
Chugh and colleagues offer several research initiatives to better define and understand the association(s) between race and ethnicity and AFib, including a call for studies that "will gather accurate race-based epidemiological data and evaluate social determinants and genetic factors in the context of multiple races and ethnicities." They also suggest that "more diverse global registries like GARFIELD-AF may help to elucidate the causes of under treatment, and to assess the effect of aggressive management of the most influential comorbidities."
Other suggestions include a "renewed emphasis on structural and social determinants of health that contribute to AFib" as a means of developing a complete and accurate picture of AFib burden in the U.S. and globally. Use of uniform AFib definitions and standardized reporting methods across all settings are also encouraged. Additionally, the authors note the importance of focused efforts to enroll and standardize reporting of individuals from underrepresented racial and ethnic groups in clinical trials to advance the evidence base for AFib management.
"A renewed and intensive focus on investigating the implications of race and ethnicity on risk, prevention, management, and outcomes of AFib is necessary for the provision of equitable care," they write.
Clinical Topics: Arrhythmias and Clinical EP, Cardiovascular Care Team, COVID-19 Hub, Heart Failure and Cardiomyopathies, Noninvasive Imaging, Prevention, Valvular Heart Disease, Atherosclerotic Disease (CAD/PAD), Atrial Fibrillation/Supraventricular Arrhythmias, Acute Heart Failure, Echocardiography/Ultrasound, Hypertension, Sleep Apnea
Keywords: ACC Publications, Cardiology Magazine, African Americans, Asian Americans, Atrial Fibrillation, Bariatric Surgery, Cardiology, Cardiovascular Diseases, Communication, Community Health Services, Coronary Artery Disease, COVID-19, Cultural Competency, Dementia, Diabetes Mellitus, Diabetes Mellitus, Type 2, Echocardiography, Ethnic Groups, Glycated Hemoglobin A, Health Care Costs, Health Equity, Health Personnel, Health Services Accessibility, Healthcare Disparities, Heart Disease Risk Factors, Heart Failure, Heart Valve Diseases, Hypertension, Implementation Science, Insurance Coverage, Minority Groups, Morbidity, Motivation, Obesity, Organizational Objectives, Outcome Assessment, Health Care, Patient-Centered Care, Peripheral Arterial Disease, Policy, Prescriptions, Prevalence, Public Health, Quality Improvement, Quality of Health Care, Racism, Reference Standards, Registries, Renal Insufficiency, Chronic, Reward, Risk Factors, Social Determinants of Health, Social Justice, Social Responsibility, Stroke, Telemedicine, Treatment Outcome, Trust
< Back to Listings