Focus on EP | COVID-19 and Arrhythmias: Something to Worry About?
As a new attending physician, I spent New Year's Eve weekend covering phone calls for my cardiology group. I expected to address the usual "emergencies": a couple of hospital transfer requests, a handful of urgent consults from inpatient providers, and the smattering of messages from anxious patients who accidentally took too much of a prescribed medication, detected an abnormal blood pressure reading or experienced frightening cardiac symptoms.
I was ill prepared for what actually occurred. In the wake of the Omicron surge and recent holiday celebrations, a significant majority of the phone calls were from frantic patients who had tested positive for COVID-19 and were unsure what to do. Most patients only had mild viral symptoms, but some reported palpitations and chest discomfort. While I was keen on catching potential cases of acute coronary syndrome and heart failure, I was less certain about arrhythmias. Was COVID-19 infection a trigger for heart rhythm conditions and, if so, was the association any different than for other viral respiratory illnesses?
A global survey of cardiac electrophysiologists who cared for patients hospitalized with COVID-19 infection from January 2020 to August 2020 reported a 12.9% incidence of cardiac arrhythmias. The majority of patients who developed arrhythmias did not have a prior history of arrhythmias. Atrial tachyarrhythmias were the most commonly observed rhythm abnormality (atrial fibrillation [AFib] 61.5%, atrial flutter [AFL] 10.4% and supraventricular tachycardia 9.7%), whereas ventricular tachyarrhythmias were the least common observed rhythm abnormality (nonsustained ventricular tachycardia 9.4%, sustained ventricular tachycardia 8.1% and ventricular fibrillation 3.4%). Nearly a quarter of the rhythm abnormalities were due to bradyarrhythmias (sinus bradycardia <40 bpm 12.8%, atrioventricular block 8.6% and pause >3 seconds 1.2%). Notably, the majority of patients with arrhythmias had been treated for COVID-19 with QTc prolonging medications including hydroxychloroquine (57.3%), azithromycin (44.3%) and quinolones (10.2%).1
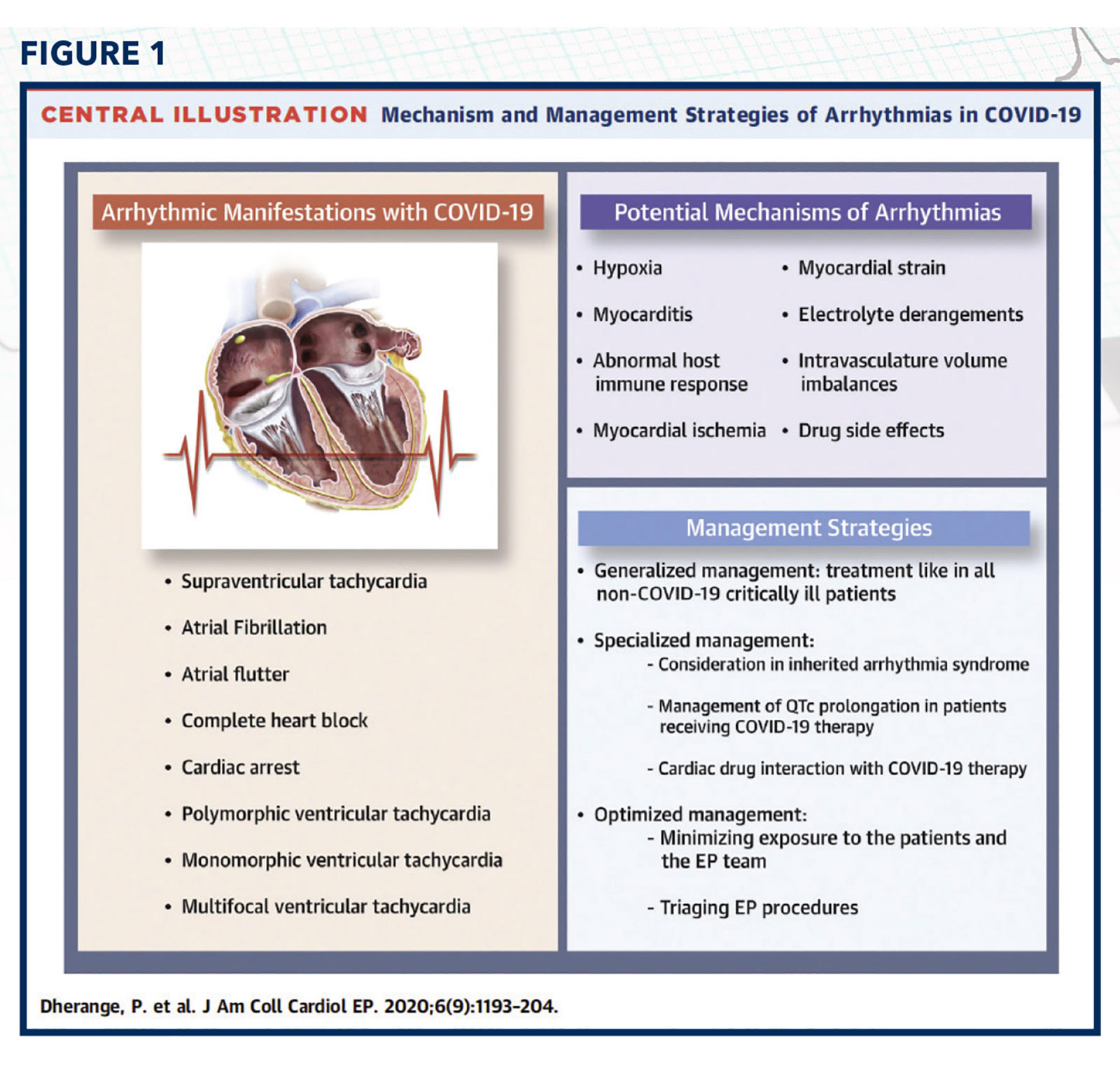
A review of arrhythmias during COVID-19 revealed that the incidence of arrhythmias was higher in patients who were critically ill: in one case series, 16.5% of ICU patients with COVID-19 experienced atrial tachyarrhythmias.2 The hypothesized mechanisms for arrhythmogenesis included hypoxia resulting from injury to lung tissue, myocarditis, abnormal host immune response, myocardial ischemia, myocardial strain, electrolyte derangements, intravascular volume imbalances and drug side effects.3
The advised treatment strategies for COVID-19-related arrhythmias emphasized medical management during the active infection, minimization of drug-drug interactions, and postponement of nonurgent procedures (cardioversions, device implantations, ablations) until after the infection had resolved (Figure 1).3
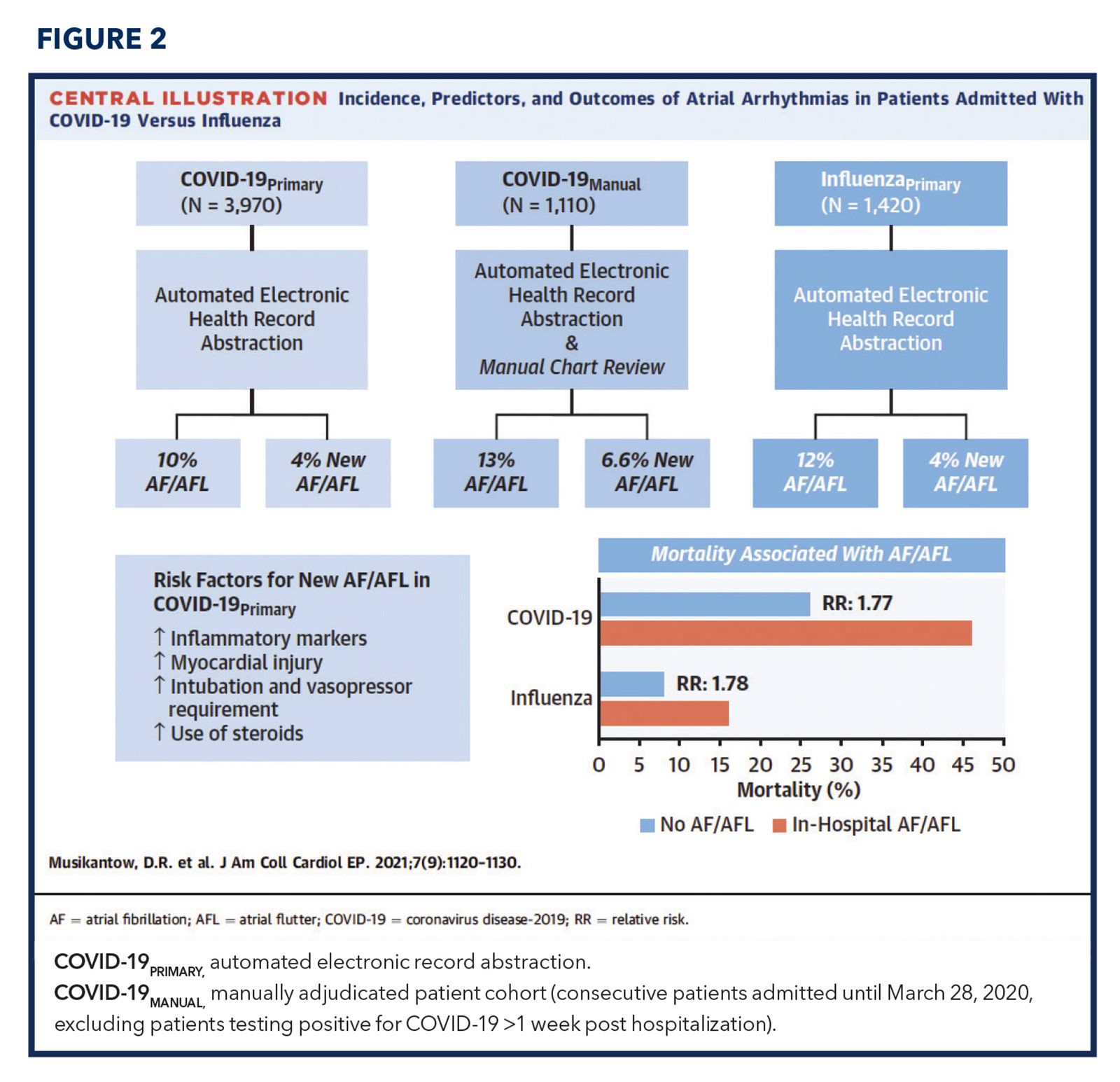
A retrospective multicenter comparison of 3,970 hospitalized patients with COVID-19 infection and 1,420 patients hospitalized patient with influenza infection determined that the incidence of in-hospital AFib/AFL was significantly higher in those with influenza than in those with COVID-19 (12% vs. 10%; p=0.03), but the proportion of influenza patients with a prior history of atrial arrhythmias was also significantly higher than the proportion of COVID-19 patients with a prior history of atrial arrhythmias (14% vs. 9%; p<0.01).4
The rates of new-onset AFib/AFL, however, were similar between the two groups (4% vs. 4%; p=0.93). Interestingly, in both patients with COVID-19 and in patients with influenza infection, new-onset AFib/AFL was correlated with higher degrees of inflammation (peak serum levels of IL-6, C-reactive protein, etc.) and disease severity (need for mechanical ventilation and/or vasopressors), independent of patient baseline characteristics. Based on these results, the study concluded that atrial arrhythmias were not unique to COVID-19 infection but instead a reflection of the systemic inflammatory response to severe viral disease (Figure 2).4
I am confident of two certainties in my near future: COVID-19 infections will not be going away, and neither will my weekend coverage assignments. The next time a patient with a new COVID-19 infection frantically calls with suspicious arrhythmia symptoms, I will be more prepared with my response. "Yes, you may have experienced an abnormal heart rhythm due to your COVID-19 infection, but you could have developed this with any other viral illness as well."

This article was authored by Edward Chu, MD, (@Ed_Chu_MD), an electrophysiology attending physician in Miami, FL.
References
- Coromilas EJ, Kochav S, Goldenthal I, et al. Worldwide survey of COVID-19-associated arrhythmias. Circ Arrhythm Electrophysiol 2021;14:e009458.
- Colon CM, Barrios JG, Chiles JW, et al. Atrial arrhythmias in COVID-19 patients. JACC Clin Electrophysiol 2020;6:1189-90.
- Dherange P, Lang J, Qian P, et al. Arrhythmias and COVID-19: A review. JACC Clin Electrophysiol 2020;6:1193-1204.
- Musikantow DR, Turagam MK, Sartori S, et al. Atrial fibrillation in patients hospitalized with COVID-19: Incidence, predictors, outcomes, and comparison to influenza. JACC Clin Electrophysiol 2021;7:1120-30.
Clinical Topics: Acute Coronary Syndromes, Arrhythmias and Clinical EP, COVID-19 Hub, Diabetes and Cardiometabolic Disease, Heart Failure and Cardiomyopathies, ACS and Cardiac Biomarkers, Implantable Devices, EP Basic Science, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Novel Agents, Statins, Acute Heart Failure, Heart Failure and Cardiac Biomarkers
Keywords: ACC Publications, Cardiology Magazine, Atrial Fibrillation, Azithromycin, Bradycardia, C-Reactive Protein, Hydroxychloroquine, Interleukin-6, Atrial Flutter, Electric Countershock, Incidence, Acute Coronary Syndrome, Atrioventricular Block, Blood Pressure, COVID-19, Critical Illness, Emergencies, Holidays, Influenza, Human, Inpatients, Myocarditis, Reading, Respiration, Artificial, Retrospective Studies, Ventricular Fibrillation, Tachycardia, Ventricular, Intensive Care Units, Systemic Inflammatory Response Syndrome, Tachycardia, Supraventricular, Drug Interactions, Drug-Related Side Effects and Adverse Reactions, Severity of Illness Index, Immunity, Heart Failure, Inflammation, Electrolytes, Cardiology, Physicians, Quinolones, Hospitals, Pharmaceutical Preparations, Lung
< Back to Listings