Prioritizing Health | Residual Cardiovascular Risk: Beyond Traditional Risk Factors

Comprehensive evaluation of atherosclerotic cardiovascular disease (ASCVD) risk is the foundation of preventive cardiology. Accurate assessment of ASCVD risk facilitates shared decision-making regarding lifestyle interventions, medical therapy and goals of care. While many risk factors for ASCVD are well-established, emerging data have uncovered new opportunities for cardiovascular risk reduction.
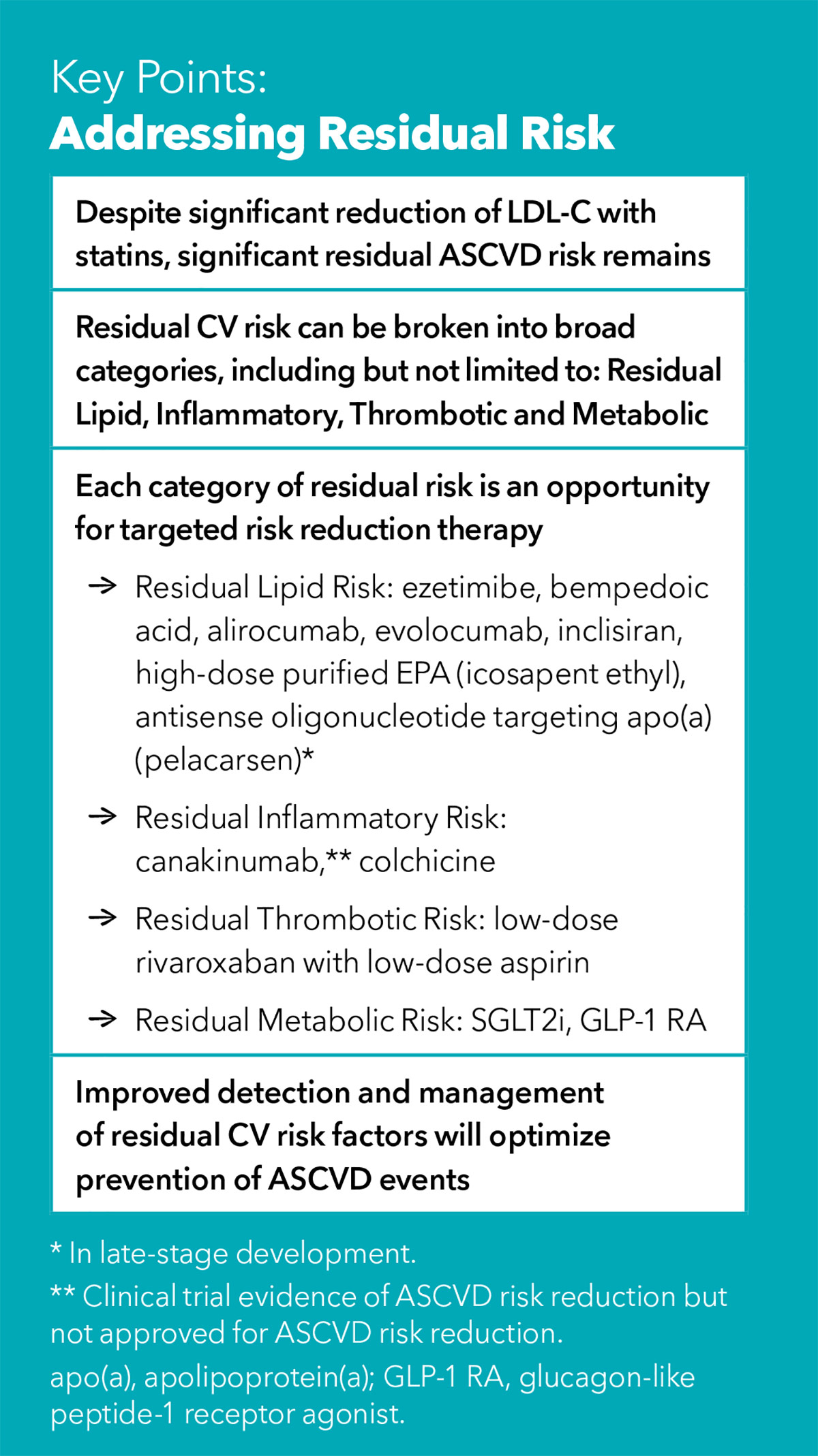
Advances over recent decades have revolutionized ASCVD risk factor management. Antihypertensive therapy and more aggressive treatment goals have led to improved blood pressure control. Tobacco cessation campaigns and interventions have led to significant reductions in tobacco use. The statin story is well known, and these agents are largely considered the most effective foundation of ASCVD prevention. However, the statin mega-trials demonstrated a 30-40% reduction in ASCVD events, leaving most patients still at risk for recurrent events. The advent of additional therapies to lower LDL-C such as ezetimibe and, particularly, PCSK9 inhibitors have transformed lipid management and prevention of ASCVD.
Yet, the number of ASCVD events remain high.1 This suggests residual risk factors are contributing significantly to the evolution and progression of ASCVD. Here is a survey of some of the key drivers of residual ASCVD risk.
Residual Inflammatory Risk
Deep Dive Into Lifestyle Medicine at ACC.22
Don't miss the two-part Lifestyle Medicine Intensive taking place on Saturday, April 2 as part of ACC.22. Led by Co-Chairs Lynne Braun, PhD, CNP and Amit Khera, MD, MSc, FACC, the intensive will feature 10 presentations designed to move beyond theory to practice. In addition, Session 1 will feature the not-to-miss Bishop Keynote with Dariush Mozaffarian, MD, FACC, on the topic of Common Ground: What do Heart Healthy Diets Have in Common?
Other topics include:
- Carnivores and Herbivores: Is Peaceful Coexistence Possible?
- Bringing Nutrition into the Conversation: Practical Tools
- Moving the Seemingly Immovable: Healthier Hospital Dietary Offerings
- Technology in Motion: Incorporating Stress Testing and Wearables
- Teams and Tools for an Office-Based Exercise Prescription
- Beyond Your Limit: The Science of Stress
- Unique Perspectives: Psychosocial Stress in Diverse Populations
- Bringing Psychological Health into the Conversation
More information on location and times is available at ACCScientificSession.org. The session will also be live streamed on the Interdisciplinary Education channel as part of the virtual ACC.22 experience.
Systemic inflammation has a well-established relationship with development of atherosclerosis and subsequent ASCVD events. The relationship between measures of inflammation and ASCVD, high-sensitivity C-reactive protein (hsCRP) and interleukin (IL)-1β and IL-6, has been considered in multiple studies. Recent clinical trials have gone beyond association to demonstrate that targeting inflammation facilitates ASCVD risk reduction.
Canakinumab, a direct IL-1β inhibitor, reduced major adverse cardiovascular events in individuals with prior myocardial infarction (MI) and hsCRP >2 mg/L vs. placebo.2 It may also reduce heart failure hospitalizations in patients with a previous MI.3,4 This benefit comes at the cost of increased neutropenia and death secondary to sepsis.3 Low-dose colchicine, another anti-inflammatory drug, improved cardiovascular outcomes in several trials,5-8 and may even prove to be practical, cost-effective preventive measure in the future.
Residual Thrombotic Risk
As ASCVD events are atherothrombotic, thrombotic risk has been an intense area of research. Antiplatelet therapy for secondary prevention following development of cardiovascular disease has become the standard of care. However, the role of routine anticoagulation use has been less studied.
The findings from two trials have made a case for low-dose anticoagulation for secondary prevention.9,10 Both trials showed that adding low-dose rivaroxaban to aspirin for secondary prevention led to improvement in cardiovascular outcomes, but at the cost of increased bleeding risk. These data suggest a role for anticoagulation as an adjunct to aspirin secondary prevention in patients with low bleeding risk, particularly in those with polyvascular disease (where ASCVD risk is highest).
Residual Metabolic Risk
Statins and PCSK9 inhibitors have transformed lipid management. Beyond LDL-C, other atherogenic lipoproteins appear to be an important source of residual ASCVD risk. Additionally, two newer diabetes medications show promising ASCVD risk reduction.
Triglycerides
The association between plasma triglyceride concentrations and ASCVD are well known. Until recently, there was no evidence that targeting triglycerides with specific triglyceride-lowering drugs improved cardiovascular outcomes. Most recently, the use of high-dose, purified eicosapentaenoic acid (EPA) in patients with elevated triglycerides (135-500 mg/dL) on statin therapy and either ASCVD or diabetes reduced ASCVD events.11 Interestingly the benefit of high-dose EPA was not related to baseline or attained triglyceride levels.
Lipoprotein(a)
Lipoprotein a (Lp[a]) is an LDL-like particle with an additional glycoprotein (apolipoprotein(a)) bound to its apolipoprotein B-100 moiety. Besides its lipid cargo, Lp(a) particles also serve as a repository for plasma oxidized phospholipids and share structural homology with plasminogen. As a result, Lp(a) exerts pro-atherosclerotic, anti-fibrinolytic and pro-inflammatory properties. The observational and genetic epidemiology demonstrate a close relationship between Lp(a) with ASCVD and calcific aortic stenosis. A novel antisense oligonucleotide targeting apolipoprotein(a) mRNA is safe and lowers plasma Lp(a) concentration by approximately 80%.12 It is currently being investigated in a large cardiovascular outcomes trial.
Diabetes
Diabetes is a well-known risk factor for ASCVD. Until recently, medications used to treat diabetes improved hyperglycemia but did not specifically improve cardiovascular outcomes. There are now two distinct classes of diabetes medications, sodium-glucose transporter 2 inhibitors (SGLT2i) as well as glucagon-like peptide 1 agonists, that demonstrate impacts on a range of cardiovascular outcomes and mortality.13–18 Moreover, the SGLT2i demonstrate benefit for management of heart failure with reduced ejection fraction independent of diabetes status.13 The recent developments in diabetes therapies have been remarkable and are poised to transform the prevention of cardiovascular disease.
Preventive cardiology is clearly in a renaissance. We now have a much greater understanding of residual risk factors and have the tools to target many of them. Diagnosis and management of key residual cardiovascular risk factors are crucial for optimizing prevention of ASCVD.


This article was authored by Trevor Caldarera, MD, internal medicine resident, and This article was authored by Trevor Caldarera, MD, internal medicine resident, and Michael D. Shapiro, DO, MCR, FACC, (@DrMichaelShapir), Fred M. Parrish Professor of Cardiology and Molecular Medicine, both at Wake Forest University, in North Carolina., (@DrMichaelShapir), Fred M. Parrish Professor of Cardiology and Molecular Medicine, both at Wake Forest University, in North Carolina.
References
- Sabatine MS, Giugliano RP, Keech AC, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med 2017;376:1713-22.
- Ridker PM, Everett BM, Thuren T, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med 2017;377:1119-31.
- Ridker PM, Everett BM, Thuren T, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med 2017;377:1119-31.
- Everett BM, Cornel JH, Lainscak M, et al. Anti-Inflammatory therapy with canakinumab for the prevention of hospitalization for heart failure. Circulation 2019;139:1289-99.
- Nidorf SM, Fiolet ATL, Mosterd A, et al. Colchicine in patients with chronic coronary disease. N Engl J Med 2020;383:1838-47.
- Tong DC, Quinn S, Nasis A, et al. Colchicine in patients with acute coronary syndrome. Circulation 2020;142:1890-1900.
- Mewton N, Roubille F, Bresson D, et al. Effect of colchicine on myocardial injury in acute myocardial infarction. Circulation 2021;144:859-69.
- Tardif JC, Kouz S, Waters DD, et al. Efficacy and safety of low-dose colchicine after myocardial infarction. N Engl J Med 2019;381:2497-2505.
- Eikelboom JW, Connolly SJ, Bosch J, et al. Rivaroxaban with or without Aspirin in Stable Cardiovascular Disease. N Engl J Med 2017;377:1319-1330.
- Mega JL, Braunwald E, Wiviott SD, et al. Rivaroxaban in patients with a recent acute coronary syndrome. N Engl J Med 2012;366:9-19.
- Bhatt DL, Steg PG, Miller M, et al. Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. N Engl J Med 2019;380:11-22.
- Tsimikas S, Karwatowska-Prokopczuk E, Gouni-Berthold I, et al. Lipoprotein(a) reduction in persons with cardiovascular disease. N Engl J Med 2020;382:244-55.
- McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med 2019;381:1995-2008.
- Packer M, Anker SD, Butler J, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med 2020;383:1413-24.
- Anker SD, Butler J, Filippatos G, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med 2021;385:1451-61.
- Wagdy K, Nagy S. EMPEROR-Preserved: SGLT2 inhibitors breakthrough in the management of heart failure with preserved ejection fraction. Glob Cardiol Sci Pract 2021;2021(3):e202117.
- Marso SP, Bain SC, Consoli A, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 2016;375:1834-44.
- Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2016;375:311-22.
Clinical Topics: Anticoagulation Management, Arrhythmias and Clinical EP, Cardiovascular Care Team, Diabetes and Cardiometabolic Disease, Dyslipidemia, Heart Failure and Cardiomyopathies, Prevention, Valvular Heart Disease, Advanced Lipid Testing, Hypertriglyceridemia, Lipid Metabolism, Nonstatins, Novel Agents, Statins, Acute Heart Failure, Heart Failure and Cardiac Biomarkers, Diet, Stress
Keywords: ACC Publications, Cardiology Magazine, ACC22, ACC Annual Scientific Session, Hydroxymethylglutaryl-CoA Reductase Inhibitors, C-Reactive Protein, Cholesterol, LDL, PCSK9 protein, human, Proprotein Convertase 9, Cardiovascular Diseases, Apolipoprotein B-100, Eicosapentaenoic Acid, Glucagon-Like Peptide-1 Receptor, Interleukin-6, Platelet Aggregation Inhibitors, Rivaroxaban, Sodium-Glucose Transporter 2 Inhibitors, Secondary Prevention, Cost-Benefit Analysis, Diet, Healthy, Herbivory, Molecular Epidemiology, Molecular Medicine, North Carolina, Standard of Care, Stroke Volume, Tobacco Use Cessation, Universities, Risk Factors, Atherosclerosis, Ezetimibe, Lipoprotein(a), Aspirin, Triglycerides, Oligonucleotides, Antisense, Heart Disease Risk Factors, Glucagon-Like Peptide 1, Myocardial Infarction, Stress, Psychological, Hospitalization, Anticoagulants, Aortic Valve Stenosis, Hyperglycemia, Risk Reduction Behavior, Patient Care Planning, Heart Failure, Inflammation, Phospholipids, Prescriptions, Tobacco Use, Cardiology, Colchicine, Technology, Diabetes Mellitus, Hospitals, Wearable Electronic Devices, Forests, Sepsis, Apolipoproteins A, Interleukin-1
< Back to Listings