Prioritizing Health | Journey of the Health and Well-Being Coaching Profession

At 20.1 million deaths in 2021, cardiovascular disease continues to be the leading cause of death worldwide,1 largely driven by modifiable lifestyle-related risk factors like poor diet, smoking and physical inactivity.2,3 Lifestyle improvements play a pivotal role in preventing and managing cardiovascular disease and many other chronic diseases. The health and well-being coaching (HWC) field has evolved over the past decade into a well-respected partnership of coaches and patients focusing on physical, emotional and behavioral health to improve cardiovascular and metabolic health and well-being.4,5
Research has shown that HWC significantly improves engagement in lifestyle interventions, leading to better cardiovascular outcomes. For example, individuals who engage in coaching programs have shown clinically significant improvements in blood pressure,6 cholesterol levels, blood glucose/A1C levels, BMI,7 cardiorespiratory fitness and overall heart health. By fostering high-quality motivation and self-efficacy, health and well-being coaches help patients become more internally motivated and confident in their ability to make meaningful health changes and maintain them over time.4,8-10
Digital HWC programs (human coaching supported with digital tools) are structured, evidence-based and increasingly delivered via telehealth.4,11 These programs begin with the enrollment and risk assessment process using patients' health data from electronic medical records along with laboratory and/or biometric results. This information helps tailor the HWC dose (session length, frequency, time frame). Patients then work with coaches to set personalized health goals and create evidence-based action plans focused on improving cardiovascular disease risk factors like diet, exercise and stress management.
Clinician Takeaways
- Encourage behavior change. Use HWC techniques to help patients find their own motivation and confidence to make heart healthy lifestyle changes.
- Integrate coaching into care. Collaborate with HWCs to design and implement comprehensive care plans for your patients.
- Empower patients. Encourage patients to take an active role in managing their cardiovascular health through evidence-based HWC.
Key Messages For Patients
- Small changes matter. HWC breaks large goals into manageable steps, making it easier to achieve long-term heart health.
- You're not alone. Coaches provide personalized, supportive guidance to help navigate your heart health journey.
- Sustainability is key. Coaches help you learn strategies to maintain heart healthy behaviors in daily life.
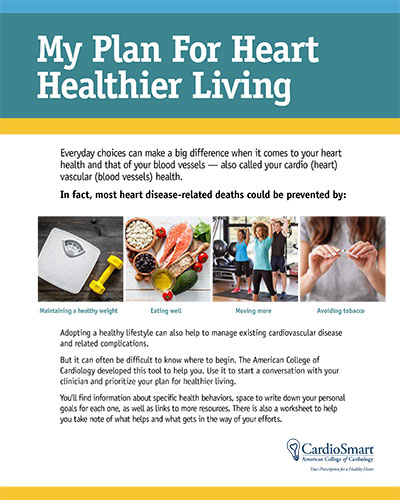
Click here to download this infographic to support patient goals and more.
Coaches, supported by artificial intelligence and digital tools, provide regular check-ins via telehealth and wearables, keeping patients engaged and adjusting plans as needed. At follow-up appointments, coaches track progress, update goals and offer additional support.
Many physician practices and health systems have successfully integrated HWC into cardiovascular care, including with patients recovering from cardiac events reporting positive lifestyle changes. In primary care, HWC improves medication adherence, follow-up visit attendance and overall cardiovascular health, with patients appreciating the personalized support that drives lasting behavior change.11
Developing the Work Force
As a new profession, the HWC field is addressing standardization, professional recognition and reimbursement. By the end of 2023, more than 125 training programs for HWC had been approved by the National Board for Health and Wellness Coaching (NBHWC), a controlled affiliate of the National Board of Medical Examiners (NBME), contributing to a U.S. workforce of more than 10,000 NBHWC-certified coaches.12 With the NBHWC board exam now offered three times a year, HWC has gained added professional credibility and wider acceptance among health care providers.
Coaches complete rigorous training, pass/fail skills assessment and certification processes to earn the National Board Certified Health and Wellness Coach (NBC-HWC) credential, which has become the gold standard in the field.13 As health care systems increasingly recognize the importance of HWC and lifestyle medicine, coaches are being integrated into primary care teams, hospitals and medically-oriented gyms.
A major opportunity for growth in HWC lies in its integration into health care systems and routine clinical care. In 2024, the American College of Lifestyle Medicine became a member of the AMA House of Delegates,14 and 3,000+ U.S. physicians are now board-certified in lifestyle medicine.15
Impacting Patient Care
HWC is key to effective implementation of lifestyle medicine in clinical care, to support patients in engaging in the six pillars of lifestyle medicine to prevent and treat chronic disease. The six pillars include exercise, diet, sleep, stress management, avoiding substance abuse and social connection.15 By collaborating with health care providers such as physicians, PAs, NPs, dietitians and physical therapists, coaches can help patients implement comprehensive care plans that address both medical and lifestyle needs.16
As research continues to show effectiveness, HWC will become more embedded into routine health care via telehealth to reach people in rural or underserved areas. The NBME's rigorous development of health professional exams, including physician licensing exams, and ongoing support for the HWC profession through NBHWC has helped establish its credibility within health care.
While CPT Category III codes for health and well-being coaching services were introduced in 2020 and are provisionally added to the Medicare Telehealth Services List starting in 2024, they are not widely reimbursed yet. The Centers for Medicare and Medicaid Services has requested published evidence of clinical benefit in medical practices using the CPT codes in order to earn permanent approval.17,18
The professionalization of the HWC field is paving the way for its future success in health care adoption and reimbursement. HWC is poised to reduce cardiovascular disease burden and improve individual and public health outcomes. Through research, certification and health system integration, it's becoming an integral part of cardiovascular care, empowering patients to make lasting lifestyle changes and achieve long-term success. Coaches will play a vital role in preventing and treating cardiovascular disease in collaboration with cardiologists, aligned by lifestyle and cardiovascular guidelines.
This article was authored by Priyansh Shah, MD, Jacobi/Albert Einstein College of Medicine and World Youth Heart Federation, in New York City; Margaret Moore, MBA, NBC-HWC, Wellcoaches Corporation, Boston, MA; and Neil F. Gordon, MD, PhD, MPH, FACC, INTERVENT International, Savannah, GA.
Learn about and join ACC's Prevention of Cardiovascular Disease Section.
References
- Lindstrom M, DeCleene N, Dorsey H. Global Burden of Cardiovascular Diseases and Risks Collaboration, 1990-2021. J Am Coll Cardiol. 2022;80(25):2372-2425.
- Lavie CJ, Ozemek C, Carbone S, et al. Sedentary Behavior, Exercise, and Cardiovascular Health. Circ Res. 2019;124(5):799-815.
- Vaduganathan M, Mensah GA, Turco JV, et al. The Global Burden of Cardiovascular Diseases and Risk: A Compass for Future Health. J Am Coll Cardiol. 2022;80(25):2361-2371.
- Gordon NF, Salmon RD, Wright BS, et al. Clinical Effectiveness of Lifestyle Health Coaching. Am J Lifestyle Med. 2016;11(2):153-166.
- Sforzo GA, Gordon NF, Peeke PM, Moore M. Health and Well-Being Coaching Adjuvant to GLP-1 Induced Weight Loss. Am J Lifestyle Med. 2024;Nov 19:15598276241302273.
- Nguyen-Huynh MN, Young JD, Ovbiagele B, et al. Effect of Lifestyle Coaching or Enhanced Pharmacotherapy on Blood Pressure Control Among Black Adults With Persistent Uncontrolled Hypertension: A Cluster Randomized Clinical Trial. JAMA Netw Open. 2022;5(5):e2212397.
- Katzmarzyk PT, Martin CK, Newton RL, et al. Weight Loss in Underserved Patients _ A Cluster-Randomized Trial. N Engl J Med. 2020;383(10):909-918.
- Gerber BS, Biggers A, Tilton JJ, et al. Mobile Health Intervention in Patients With Type 2 Diabetes. JAMA Netw Open. 2023;6(9):e2333629-e2333629.
- Krishnamurthi R, Vandal AC, Barker‐Collo S, et al. Health and Wellness Coaching for 5-Year Projected Cardiovascular Health. Neurol Clin Pract. 2024;14(1):e200220.
- Gordon NF. Clinical Effectiveness of Lifestyle Management Programs: Importance of the Class Effect Paradox. Curr Treat Options Cardiovascr Med. 2013;15(6):675-680.
- Maddison R, Rawstorn JC, Stewart RAH, et al. Effects and Costs of Real-Time Cardiac Telerehabilitation: Randomised Controlled Non-Inferiority Trial. Heart. 2019;105(2):122-129.
- National Board for Health and Wellness Coaching. NBC-HWC Online Portal. Available here.
- National Board for Health and Wellness Coaching. Find A Continuing Education Course. Available here.
- Shroyer B. A Major Milestone: ACLM Inducted into the American Medical Association House of Delegates. American College of Lifestyle Medicine. Published June 20, 2024. Accessed January 23, 2025. Available here.
- American College of Lifestyle Medicine. Fact Sheet. Available here.
- Paz E, Pargaonkar VS, Roach BJ, et al. Comprehensive Cardiovascular Risk Factor Control With a Mobile Health Cardiovascular Risk Self‐Management Program. J Am Heart Assoc. 2024;13(10):e033328.
- Bryant CX, Lundman J, Moore M. Lessons Learned from the Wellness Coaching Profession. ACSM Health Fitness Journal. 2024;28(5):6-9. doi:https://doi.org/10.1249/fit.0000000000000985
- Abu Dabrh AM, Reddy K, Beech BM, Moore M. Health & Wellness Coaching Services: Making the Case for Reimbursement. Am J Lifestyle Med. 2024;July 19:5598276241266784.
Clinical Topics: Cardiovascular Care Team, Prevention, Sports and Exercise Cardiology, Diet, Smoking
Keywords: Cardiology Magazine, ACC Publications, Mentoring, Life Style, Cardiorespiratory Fitness, Smoking, Diet