Focus on EP | HRS 2025: 5 Takeaways Impacting Practice
Electrophysiology is in the midst of a tremendous paradigm shift driven by new scientific, clinical and operational developments. Heart Rhythm 2025 (HRS 2025) provided a glimpse of these "disruptive advancements," many of which have yet to reach maturity but will be affecting future generations of patients and practitioners. If you missed the meeting, we've got you covered with these key takeaways. You'll want to keep an eye on these!

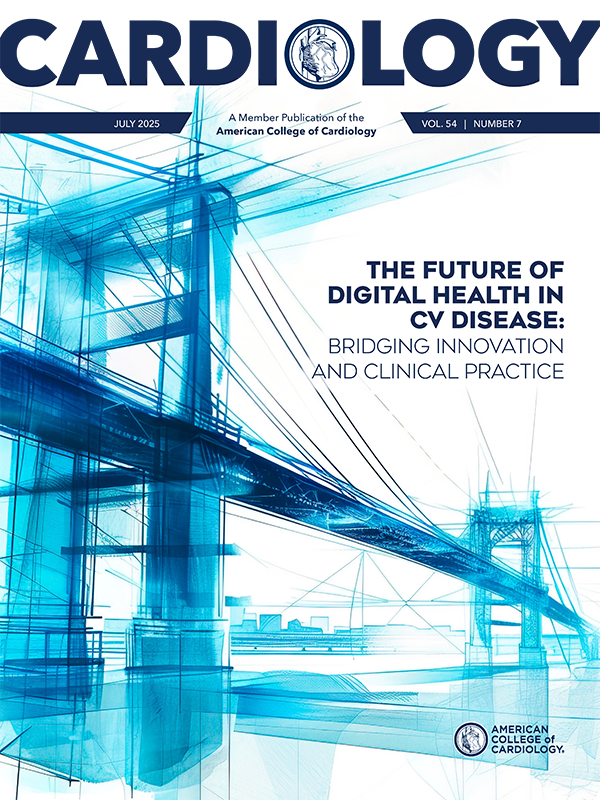
PFA Explosion
For cardiac electrophysiologists (EPs), pulsed field ablation (PFA) is undoubtedly the most disruptive technology in recent memory. The pre-conference PFA Live Case Summit showcased the novel use of existing PFA technologies in atrial fibrillation (AFib) to treat nonpulmonary vein (PV) substrates (e.g., cavotricuspid isthmus and mitral isthmus) as well emerging PFA technologies that further optimize PV isolation and ventricular ablation.
The late-breaking clinical trials (LBCTs) highlighted the successful use of two novel PFA systems in the treatment of paroxysmal AFib: the Globe Pulsed Field system in the PULSAR IDE trial and the OMNYPULSE system in the Omny-IRE trial. Additionally, there was the first novel PFA system (FieldForce) for the treatment ventricular tachycardia (VT).
Of all the PFA systems on display, the FieldForce catheter, which is capable of contact-force sensing and creating a transmural ventricular lesion, impressed me the most.

Not Your Father's Device Implant
Several LBCTs highlighted the benefit of conduction system pacing, leadless pacing and novel ICDs as an alternative to traditional transvenous cardiac implantable electronic devices with pacing leads in the right ventricle (RV) apex and/or coronary sinus.
The I-CLAS multicenter registry six-year results, presented by Pugazhendhi Vijayaraman, MD, FACC, showed that among 2,579 patients with an LVEF <50% who underwent CRT plus left bundle branch area pacing (LBBAP) or biventricular pacing, LBBAP was associated with a significantly lower rate of death or heart failure hospitalizations (20.5% vs. 29.5%, p=0.002) and procedural complications (3.5% vs. 6.5%, p=0.004) as well as a narrower paced QRS (mean 129 vs. 143 ms, p<0.001).
The LEADR LBBAP study, also presented by Vijayaraman, showed that defibrillation threshold testing was successful in all 162 patients indicated for an ICD who underwent implantation of an ICD lead at the LBBAP position using the OmniaSecure lead. No procedure-related major complications were observed.
The first in-human experience of a leadless pacemaker system, called Aveir, implanted at the LBBAP position was presented by Vivek Reddy, MD. Of the 14 patients enrolled, implant was deferred in two patients with unfavorable anatomy on preprocedure imaging and aborted intraprocedurally in two patients due to inadequate implant position. In the 10 patients with successful implantation, intraprocedural pacing, sensing and impedance measurements were within normal range (comparable to transvenous lead measurements) and one-month freedom from serious adverse device events was 87.5%.
In a comparison of transvenous ICD implant against subcutaneous ICD implant in the PRAETORIAN-XL trial, Louise Olde Nordkamp, MD, reported that at eight years there was a significant difference in all device-related complications (8.0% vs. 11.6%, p=0.15). However, those who underwent subcutaneous ICD implant experienced significantly fewer major complications (5.7% vs. 10.2% transvenous, p=0.03) and lead-related complications (2.4% vs. 8.3% transvenous, p<0.001).
The INTEGRA-D trial examined outcomes with a single transvenous device capable of providing ICD and cardiac contractility modulation therapy (Optimizer Integra CCM-D). Niraj Varma, MB, ChB, FACC, reported that among 100 patients with LVEF <40% indicated for ICD but not CRT, defibrillation threshold testing was successful in all cases (94% first shock efficacy) and one-month procedural complication rate was 5% (no deaths).

Pinpoint the Target Substrate
Given the inherent variation in cardiac anatomy among patients, an ongoing challenge in conduction system pacing and high-risk ablation procedures is localizing the site where the delivered therapy would be most effective. The benefit of advanced cardiac imaging for improving procedural efficacy was the focus of several LBCTs.
In a study presented by Shunmuga Sundaram Ponnusamy, MD, cardiac CT was used in 264 patients who underwent LBBAP to characterize the RV lead tip position related to the origin of the LBB and the LV endocardium. Greater improvements in LVEF were seen in patients with shorter distances from the lead tip to the LBB (0.25% LVEF increase for each additional 1 mm proximity, p<0.01) as well as from the lead tip to the LV endocardium (0.63% LVEF increase for each additional 1mm proximity, p=0.01).
In the MADURAI LBBP study, presented by Ponnusamy, cardiac MRI was used to characterize LV scar burden in 225 patients with nonischemic cardiomyopathy and an LVEF <35% who underwent either LBB pacing (LBBP) for scar burden <10% or LBBP + ICD for scar burden ≥10%. Over the 30-month mean follow-up, the primary composite endpoint of death, heart failure hospitalization or VT/ventricular fibrillation (VF) significantly lower in those with a scar burden <10% compared to ≥10% (6.9% vs. 26.1%, p<0.001). The authors concluded that cost-effective CRT may be safely provided by preprocedure cMRI characterization in patients with nonischemic cardiomyopathy and LVEF <35% undergoing CRT.
The InEurHeart trial, presented by Frederic Sacher, MD, randomized 113 patients with prior myocardial infarction and clinically significant VT to either CT-guided VT ablation or conventional VT ablation (without imaging guidance). CT guidance included the use of artificial intelligence software that created 3D models of the heart and identified arrhythmogenic targets for ablation. In the per protocol analysis, CT-guided VT ablation had a mean procedure duration that was significantly less than conventional VT ablation (107.1 vs. 148.8 minutes, p<0.001) but one-year freedom from VT was not significantly different between groups (80.4% vs. 66%, p=NS).

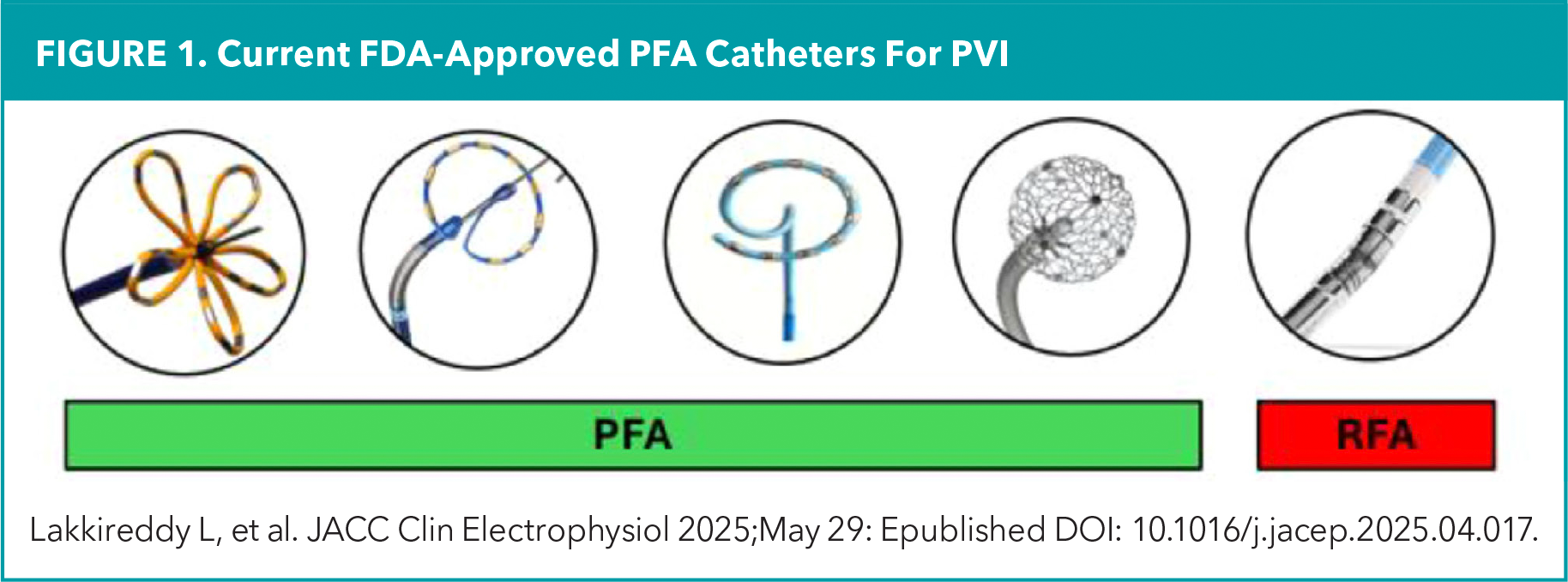
Novel Ablation Indications For Puzzling Conditions
Ablation is emerging as a treatment strategy for arrhythmias arising from genetic and autonomic etiologies, which historically have lacked an identifiable ablation target. Two LBCTs demonstrated the safety and efficacy of radiofrequency ablation in the treatment of Brugada syndrome, functional bradycardia and vasovagal syncope.
BRAVE, the first randomized controlled trial to evaluate the safety and efficacy of catheter ablation in the prevention of VF in 52 patients with symptomatic Brugada syndrome and ICDs, presented by Koonlawee Nademanee, MD, FACC, found a decrease in VF events with catheter ablation vs. medical management (20% vs. 52%, p=0.02) at three years. Furthermore, 83% of patients were VF-free after a single ablation procedure and 90% were VF-free after a repeat ablation procedure. The only complication was a hemopericardium. Due to the superiority of catheter ablation in the interim analysis period, the trial was terminated early.
The first U.S. multicenter registry on the feasibility, safety and efficacy of cardioneuroablation provided insights on the compassionate use of functional bradycardia and/or vasovagal syncope refractory to medical management and behavioral modification. Roderick Tung, MD, reported that in 205 patients (210 procedures), endocardial ablation was performed at anatomical sites of typical ganglionated plexi in the right and left atrium. At 14 months, 78% of patients remained free of syncope recurrence with a median reduction in syncopal episodes from seven before the reduction to one afterwards. Complications occurred in 4.7% of cases with a major adverse event rate of 1.4% (two hemopericardium and one death).

PEs, ASCs and Advocacy
Disruptive forces affecting the profession were the subject of discussions and debates during the Business of EP forum. Private equity employment has become an attractive model for younger and older EPs, who are interested in long-term equity partnership or a retirement parachute, respectively. Ambulatory surgical centers (ASCs) are on the brink of receiving approval for atrial fibrillation ablations, which seems like the natural progression for a procedure that has evolved into a same-day discharge encounter. Heart Rhythm Advocates has been established, a committee dedicated to addressing broader politics and policies, such as decreasing procedural reimbursements, that threaten the practice of EP.

This article was authored by Edward Chu, MD, FACC (@Ed_Chu_MD), an electrophysiology attending physician in Miami, FL.
Clinical Topics: Arrhythmias and Clinical EP, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias
Keywords: Cardiology Magazine, ACC Publications, Wearable Electronic Devices, Ablation, ACC Advocacy, Arrhythmias, Cardiac