From the Member Sections | Right Sizing Compensation Models For Cardiovascular Imagers

The field of cardiovascular imaging plays a pivotal role in cardiovascular medicine and is widely recognized as an essential and growing subspecialty within cardiology. Given this importance and growth, the ACC's Imaging Member Section is leading multiple education and advocacy initiatives, one of the biggest of which involves the creation and implementation of compensation models.
As imaging services provided by cardiologists continue to grow, health care systems must recognize payment models that will value and appropriately reward the contribution made by imagers, keeping in mind there is no one-size-fits-all model. Not only does the scope of work of imagers vary widely by the type of imaging tests performed and interpreted, but different practice settings may require different approaches.
Below we describe the pros and cons of different compensation models and suggest various considerations for a path forward.
RVU-Based Compensation
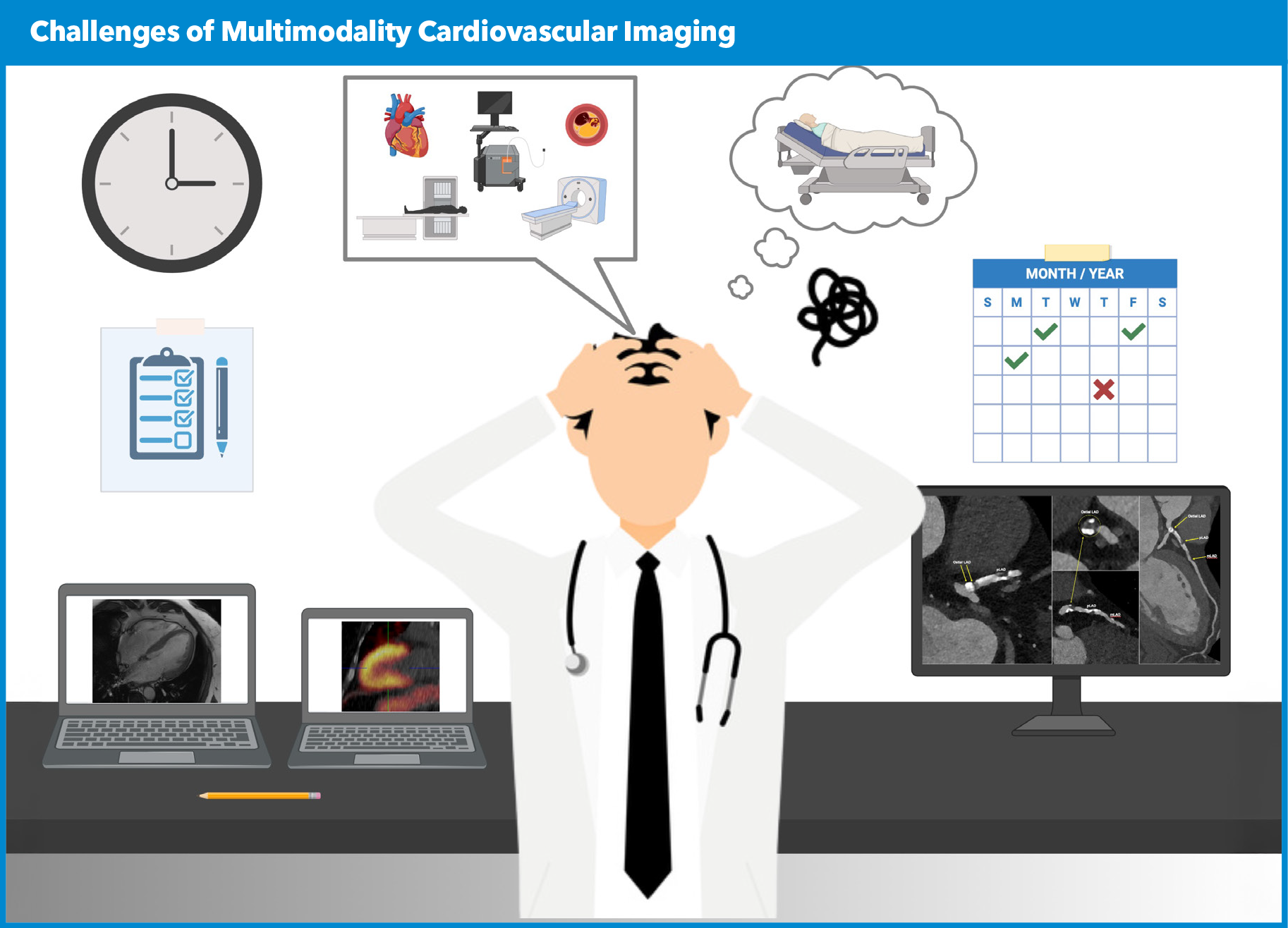
In this model, pay is tied to the number of work Relative Value Units (wRVUs) generated. This system rewards volume and efficiency but underrecognizes nonbillable tasks (e.g., reviewing prior images for comparison, reviewing images with clinical teams, teaching).
RVU-based models may reward readers who are fast, especially if they are involved in tests that can be read more quickly, such as transthoracic echocardiograms, and if there is a high volume of normal exams. However, such models do not work well for those who are involved in performing more complex exams, such as structural heart disease cases, or who are involved with modalities that require more time, such as cardiac CT or MRI.
Structural echo is particularly problematic in an RVU-based model because of the time involved and the paucity of associated RVUs. Indeed, anecdotes from institutions that are heavily RVU-based suggest imagers will prioritize reading normal cases from shared reading lists, while avoiding the more complex and timely cases.
In RVU-based models, interpreting echo and nuclear cardiology studies is often better compensated, while performing complex cardiac CT and cardiac MR exams may be less attractive. Some groups have solved this issue by applying "shadow" wRVUs or Time Value Units (TVUs) that allow for increased payment for these more complex imaging studies.
Pooled RVU Model
All RVUs generated by imagers within a practice are combined, and compensation is distributed proportionally based on each imager's time commitment to imaging activities. It should be noted that pooled RVU models may involve all cardiovascular subspecialties. Using a pooled compensation model requires the Group to meet the Group Practice of Medicine rules – which may seem complex but offers a solution.
TVU-Based Compensation
Each activity is assigned a TVU based on the estimated time or institutional priority (e.g., one day of imaging = X TVUs or 1 minute = 1 TVU). Setting up this model may require time motion studies to ensure accurate capture of the median time per CPT code.
Alternatively, this model can be based on a plan for strategic growth that allows for payment according to time spent on growth initiatives. Under such a system it may be useful to define how many imaging studies constitute a day of work. For example, a day of cardiac CT may consist of 20 studies whereas a day of echocardiography may consist of 35 studies, or a day of structural imaging (two or three cases) would equate to eight hours. The concept is that compensation is based on the time spent performing imaging, rather than on RVUs.
Limitations of TVUs include their lack of standardization and the potential subjectivity of assigning time or value to tasks. One must also consider that payment will be by wRVUs, thus care is needed to avoid a large delta between payment and compensation.
Strengths of a TVU-based approach is that it will appropriately value imagers who are involved in complex cases (e.g., structural heart disease interventions) or who perform and interpret tests that are more complex.
Salary-Based Model
This model features a fixed salary depending on workload. Such models are more common in academic centers and provide stability, but with less incentive for productivity. Of note, it may undervalue high-volume imagers. At the same time, if it is structured with transparency and it appropriately values nonbillable activities, such as teaching and research, it can promote equity and a culture of team work (i.e., we're all in this together and divide and conquer to get the work done).
Salary-Based + Incentive Model
In this model, there is a salary plus a bonus for exceeding RVU thresholds or meeting other metrics. Incentives may be based on exceeding wRVU thresholds or on measures of quality, such as report completion and turnaround time, or for teaching, leadership or research contributions.
The Path Forward
While current payment models remain heavily focused on RVUs, we believe the path forward could be based on TVU- or salary-based models, with incentives that align with the values and mission of an organization. Such models may better reward high performance clinical work and collaboration, while promoting equity across different imaging subspecialties.
We urge clinical service line leaders to replace RVU models with models that capture the full value of the contributions made by cardiovascular imagers. An important limitation in applying RVUs to measuring imaging productivity is that these units are based on surveys conducted in different time periods and by different groups of responders for different modalities.
The scenarios that are used to calculate these units are often outdated and do not represent complex cases or the extra time that imagers may use to ensure proper patient preparation, review prior test results or communicate with other members of the heart team.
Another important issue with RVU-based measures is that imagers don't "control" their clinical volume, as it depends more on referrals. Even if volumes were a metric that could be influenced, it is important to ensure that payment systems do not have any unintended consequences and that testing remains limited to those who have appropriate indications.
When structuring payment models for imagers, it is important to recognize that imaging generates significant revenue for hospitals (from technical fees) and creates value for other hospital services including electrophysiology, interventional cardiology, congenital heart disease, cardiac surgery and heart failure. Accordingly, it may be appropriate to allocate support from alternative revenue streams such as the hospital or catheterization laboratory.
Payment models should also align with institutional priorities. For example, paying for expanded imaging services during off hours (e.g., weekends and evenings) may help reduce hospital and emergency department length of stay. In turn, multimodality imagers have a responsibility to ensure that more expensive and less available imaging services remain limited to those who stand to benefit the most.
Advanced imagers can also help reduce unnecessary testing and create patient-centered algorithms on how to evaluate different conditions. Appropriate use documents and resources from the ACC can help in this regard. In sum, advanced imagers can serve as effective leaders and help ensure appropriate resource utilization in the inpatient and outpatient settings.
In summary, the growth of multimodality imaging has transformed cardiovascular medicine, offering powerful tools for diagnosis, risk stratification and treatment planning. As the field advances, it is essential not only to invest in appropriate training and education of advanced imagers, but also to establish a compelling business case that supports fair and sustainable compensation for this increasingly important subspecialty. In parallel, imagers must continue to demonstrate their value by guiding appropriate test selection and ensuring that imaging results are effectively integrated into clinical decision-making to improve patient outcomes.
Clinical Topics: Noninvasive Imaging, Computed Tomography, Magnetic Resonance Imaging, Nuclear Imaging
Keywords: Cardiology Magazine, ACC Publications, Magnetic Resonance Imaging, Tomography, X-Ray Computed, Compensation and Redress