Perspective | Optimizing ACC's Strategic Vision: Integrating Behavioral Medicine to Achieve Comprehensive CV Care
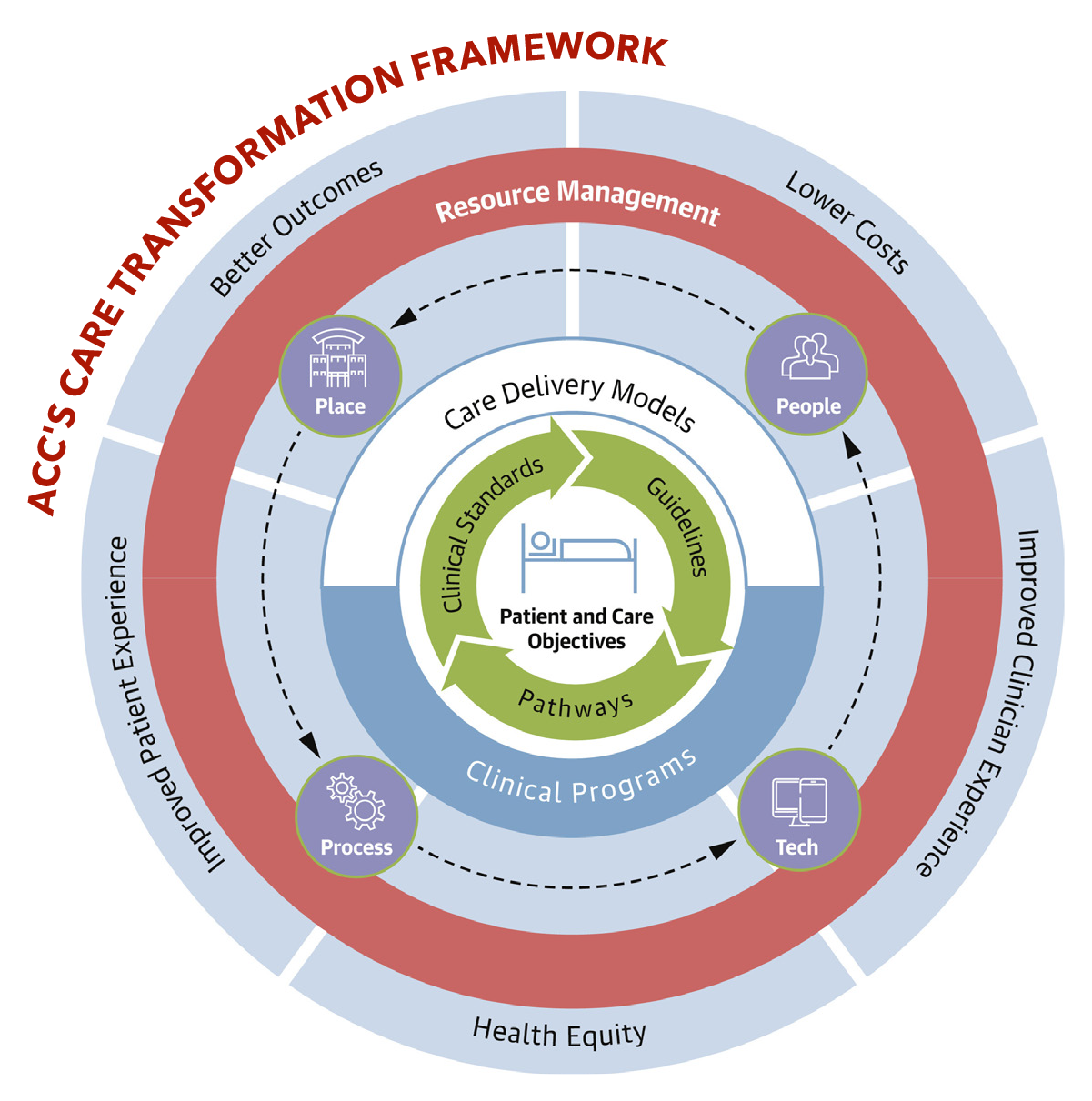
The ACC's reimagined framework for cardiovascular care delivery and implementation is a commendable and timely effort to build a more patient-centered, equitable and efficient system of care.1 Incorporating social determinants of health, team-based care, broad physical delivery mechanisms and technology is an excellent advance that lays a strong foundation. However, to fully realize its potential, the framework must also thoughtfully address behavioral and psychosocial health.2
Incorporating Behavioral and Psychosocial Health
Cardiovascular outcomes are shaped by behavioral and psychosocial factors, such as smoking, physical inactivity, poor diet and sleep, depression, anxiety and stress. These factors drive cardiovascular risk and prognosis, treatment adherence and health care utilization.3 Building on the recognition of social determinants and drivers of health, the framework can be enhanced by incorporating strategies to assess and mitigate behavioral and psychosocial concerns.4
Integrating Cardiac Psychologists Into Care Teams
Cardiac psychologists are specialists who are trained to address the behavioral and psychosocial drivers of cardiovascular health and disease, and manage psychological distress (e.g., depression and anxiety). Integrating cardiac psychologists into care teams improves patient adherence, outcomes and satisfaction, while reducing provider burden.5-7 This integration could also yield cost savings.8
Utilizing Centralized, Remote Behavioral Health Models
Given the current shortage of cardiac psychologists, centralized and remote behavioral health models offer an effective and scalable solution. To illustrate, the CODIACS trial showed that centralized depression care delivered to remotely to patients after an acute coronary syndrome improved depression, reduced cardiac events and was cost-neutral, even with the addition of the depression care.9 Centralized, remote care models can amplify cardiac psychologists' impact by complementing their in-person services, broadening their reach and enhancing access to, and convenience of, high-quality care.
Leveraging Digital Health Technologies
Digital health technologies (e.g., internet interventions, telehealth, remote monitoring, digital cognitive behavioral therapy and artificial intelligence-based platforms10,11) are both appealing and practical. For patients, these tools are convenient, time efficient and accessible. For providers and health care systems, these tools can support personalized interventions and minimize personnel, training and space requirements. Ultimately, these innovations could scale care delivery, advance precision behavioral medicine and potentially drive down costs.
Broadening Outcome Metrics
Comprehensive cardiovascular care evaluation should extend beyond traditional metrics to include behavioral and psychosocial risk and prognostic factors, quality of life, patient and caregiver satisfaction, and economic outcomes. This broader lens will provide a holistic assessment of care effectiveness and promote alignment among the priorities of patients, providers and the health care system.
Moving Forward
The ACC's new framework for cardiovascular care delivery represents significant progress toward modernizing cardiovascular care. For optimal effectiveness and efficiency, it must incorporate behavioral and psychosocial health, integrate cardiac psychologists, utilize centralized care models, leverage digital health and broaden outcome metrics. This effort requires building organizational support for integrated care models, growing the cardiac psychologist workforce, and addressing reimbursement issues. Ideally the ACC should evaluate the cost-effectiveness of their new framework vs. a framework incorporating the enhancements proposed here. Exemplars for overcoming these barriers are available to serve as roadmaps.12-15
Holistic cardiovascular care aligns with the American Medical Association's Behavioral Health Integration Collaborative,16 and is essential to the ACC's Mission to transform cardiovascular care and improve heart health.
This article was authored by Allison E. Gaffey, PhD, Section of Cardiovascular Medicine, Yale School of Medicine, and the VA Connecticut Healthcare System, New Haven, CT; Jesse C. Stewart, PhD, Department of Psychology, Indiana University Indianapolis, Indianapolis, IN; Alyssa M. Vela, PhD, Division of Cardiac Surgery, Northwestern University Feinberg School of Medicine, Chicago, IL; Josefin Särnholm, PhD, Division of Cardiac Surgery, Northwestern University Feinberg School of Medicine, Chicago, Department of Clinical Neuroscience, Karolinska Institute, Stockholm, Sweden and Center for Behavioral and Cardiovascular Health, Columbia University Medical Center, New York; and Matthew M. Burg, PhD, Department of Anesthesiology, Yale School of Medicine.
References
- Bhatt AB, Biesbrock GK, Biga C. Best practices for transforming cardiovascular care delivery and implementation: a modern framework. J Am Coll Cardiol 2025;85:1580-2.
- Burg MM, Stewart JC, Gaffey AE, et al. Behavioral medicine can tackle cardiovascular disease risk and burden: a call for new priorities. Policy Insights from the Behavioral and Brain Sciences 2025:23727322241306071.
- Levine GN, Cohen BE, Commodore-Mensah Y, et al. Psychological health, well-being, and the mind-heart-body connection: a scientific statement from the American Heart Association. Circulation 2021;143:e763-e783.
- Biga C, Wilson BH. Realizing our vision: ACC's next 5-year strategic plan. J Am Coll Cardiol 2024;83:1489-91.
- Ladapo JA, Davidson KW, Moise N, et al. Economic outcomes of depression screening after acute coronary syndromes: The CODIACS-QoL randomized clinical trial. General Hospital Psychiatry 2021;71:47-54.
- Skúladóttir H SJ, Wallén H, Ólafsdóttir E, et al. Physiological and psychological factors in symptomatic atrial fibrillation: Cost-effectiveness of online cognitive behavioral therapy for symptomatic paroxysmal atrial fibrillation. Karolinska Institutet; 2024.
- Holdgaard A, Eckhardt-Hansen C, Lassen CF, et al. Cognitive-behavioural therapy reduces psychological distress in younger patients with cardiac disease: a randomized trial. Eur Heart J 2023;44:986-96.
- Dorling G, Fountaine T, McKenna S, Suresh B. The evidence for integrated care. McKinsey and Company. 2015;
- Kronish IM, Moise N, Cheung YK, et al. Effect of depression screening after acute coronary syndromes on quality of life: the CODIACS-QoL randomized clinical trial. JAMA Intern Med 2020;180:45-53.
- Särnholm J, Skuladottir H, Rück C, et al. Cognitive behavioral therapy improves quality of life in patients with symptomatic paroxysmal atrial fibrillation. J Am Coll Cardiol 2023;82:46-56.
- Rollman BL, Muldoon MF, Magnani JW. Four "E" s to speed adoption of mHealth and promote cardiovascular behavioral medicine. Health Psychology 2022;41:765.
- Gaffey AE, Harris KM, Mena-Hurtado C, Sinha R, Jacoby DL, Smolderen KG, et al. The Yale roadmap for health psychology and integrated cardiovascular care. Health Psychology 2022;41:779.
- Vela AM, Carroll AJ. Cardiac psychology: Psychosocial and behavioral assessment and treatment for cardiovascular conditions. J Health Service Psychology 2023;49:21-32.
- Sall KE, Griffith AM, Midgette EP, et al. Cardiac psychology training in a rural health care setting: East Carolina Heart Institute. Health Psychology 2022;41:803.
- Smolderen KG, Gillaspy S, Evers AW, et al. The role of the clinical psychologist in the care of adults with cardiovascular disease. JACC Advances 2024;3:100910.
- American Medical Association. Behavioral Health Integration (BHI) Collaborative. Available here.
Clinical Topics: Cardiovascular Care Team
Keywords: Cardiology Magazine, ACC Publications, Behavioral Medicine, Social Determinants of Health, Cognitive Behavioral Therapy, Digital Technology, Psychological Distress