Cover Story | Secondary Mitral Regurgitation: When to Refer, When to Treat and How to Treat?
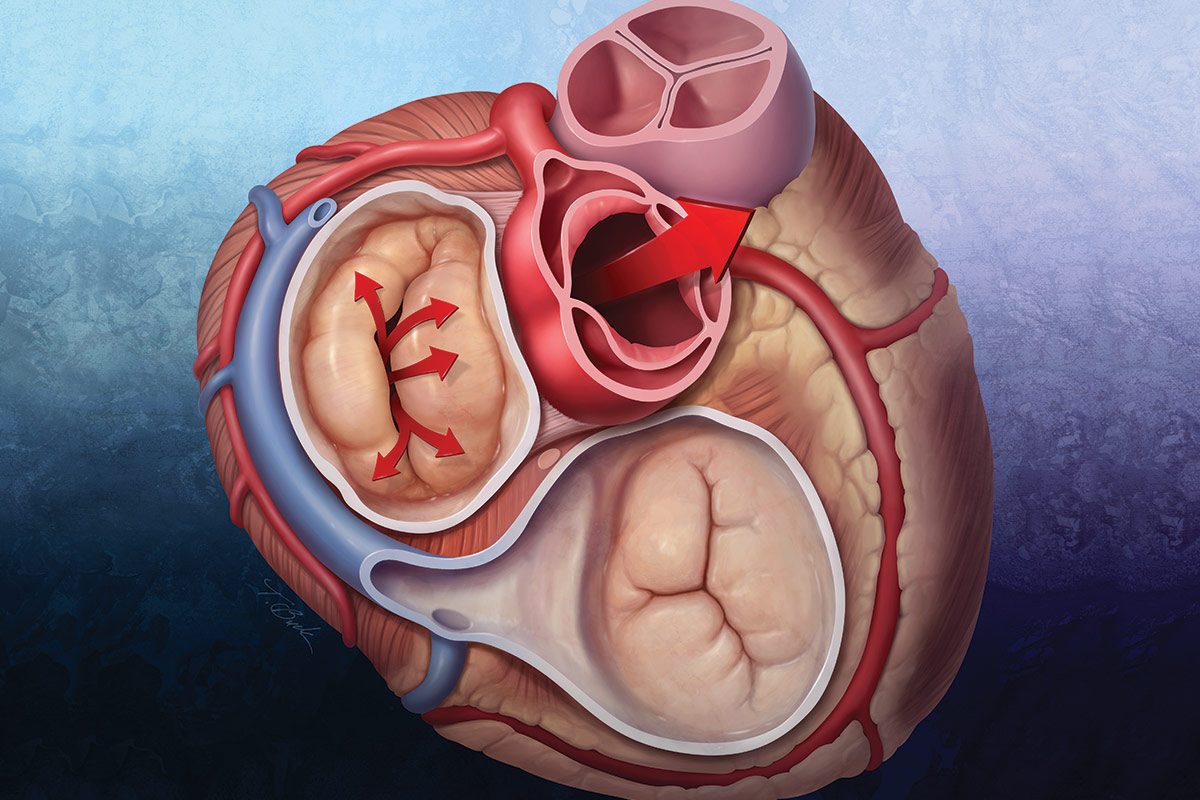
Some degree of mitral regurgitation (MR) is present in about 10% of older patients and in about one-third of patients with heart failure with reduced ejection fraction (HFrEF). It's no small wonder why – it takes proper and coordinated interaction of the annulus, commissures, leaflets, chordae tendineae, papillary muscles, and the left ventricle to ensure valve integrity. Abnormalities in any of these structures can lead to retrograde flow through the mitral valve.
Secondary (functional) MR has at its root cause left ventricular (LV) dysfunction and remodeling (due to ischemic or nonischemic myocardial disease) that adversely impacts leaflet tethering forces. Another etiology is related to enlargement of the mitral annulus secondary to left atrial dilatation in individuals with atrial fibrillation and other cardiomyopathies. Functional MR is differentiated from primary (degenerative) MR, which is a disease of the mitral valve leaflets or elongation or rupture of the subvalvular chords.
"There is a lot of confusion around whether functional MR should be treated and, if so, how and when it should be treated," says Raj R. Makkar, MD, FACC, vice president, Cardiac Intervention and Innovation, at Cedars-Sinai Medical Center in Los Angeles.
When should patients with functional MR be referred to a Comprehensive Valve Center? How far will medical therapy take you? Why does it make sense to fix the valve when really the left ventricle is the problem? When is transcatheter edge-to-edge repair (TEER) a better option?
The field has an up-to-date guideline, published in December 2020, but guidelines can be cumbersome for the non-subspecialist, particularly when recent data have been conflicting (think, COAPT and MITRA-FR). This month Cardiology spoke with four experts in the field – two cardiothoracic surgeons and two interventionalists – to provide some texture and commentary around the guidelines and answer some of these common clinical questions.
Short summary: Collaboration is key. It takes a village of cardiology professionals to diagnose and treat a disease that has minimal or subtle signs and symptoms in the beginning (like fatigue); starts in the ventricle (or the atria) but impacts the valve; and has both pharmacological therapies and advanced interventions that work to differing degrees in different patients.
Medical Treatment of Functional MR
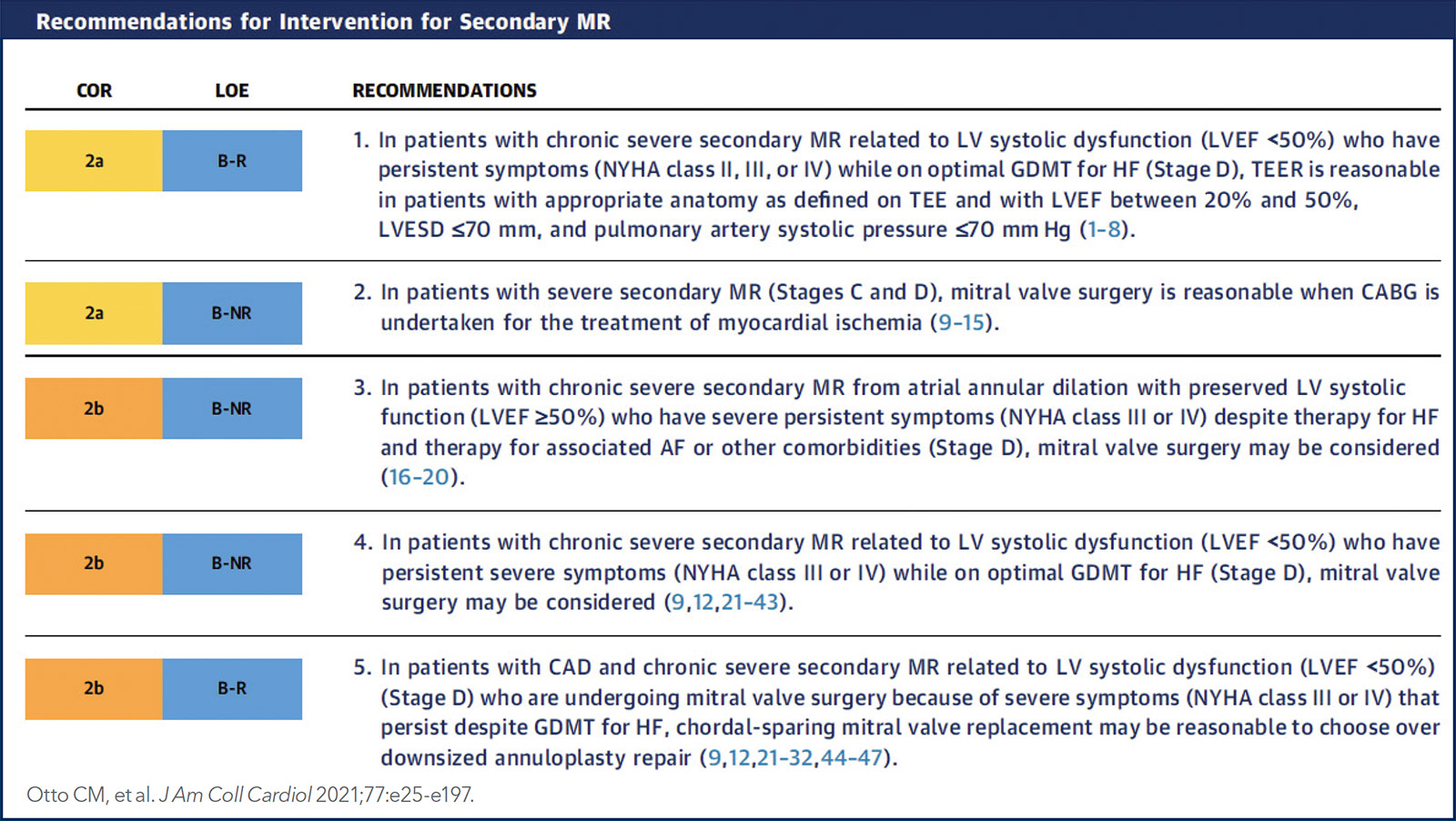
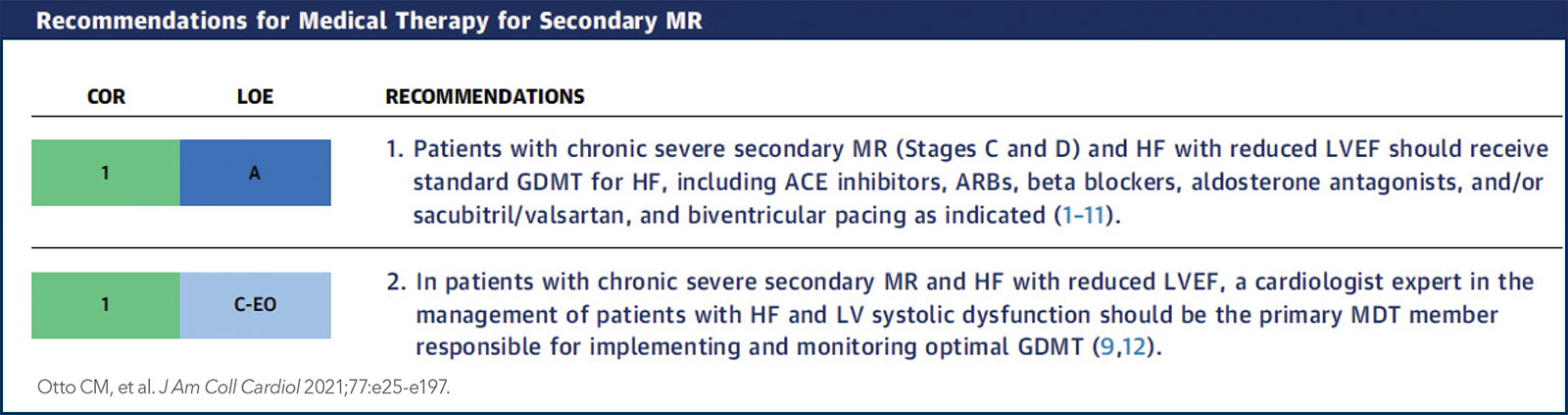
According to the current ACC/American Heart Association (AHA) guideline on valvular heart disease, individuals with chronic severe functional MR (stage C or D, meaning asymptomatic severe or symptomatic severe disease) should first be treated with guideline-directed medical therapy (GDMT) supervised by a HF specialist.1 Because chronic severe functional MR usually develops as a result of LV systolic dysfunction, standard GDMT for HF forms the mainstay of therapy. This includes diuretics, beta-blockers, ACE inhibitors or ARBs, and aldosterone antagonists.

Raj R. Makkar, MD, FACC
This is in contrast to primary MR, where the benefits of medical therapy with respect to valve function and clinical outcomes are less well established. Significant reductions in functional MR also occur with cardiac resynchronization therapy (CRT) and this option should be tried, if appropriate, before any advanced intervention is considered.
In a patient with functional MR related to LV systolic dysfunction and persistent severe symptoms despite optimized GDMT (and CRT, if appropriate), the guidelines say TEER is a "reasonable" option in those with appropriate anatomy and hemodynamics. Surgery may also improve symptoms in some patients with severe functional MR, with mitral valve replacement preferred over repair. The decision to go with one option over the other is the purview of the Heart Valve Team.
When to Refer to a Heart Team
According to the 2020 ACC/AHA Guideline, patients with severe valvular heart disease should be evaluated by a Multidisciplinary Heart Valve Team when intervention is considered.1 According to the experts interviewed here, earlier is better than later.
"When a patient is diagnosed with even moderate MR, they need to be seen by a Heart Team at a valve center. This isn't because the general cardiologist or heart failure specialist isn't capable of taking care of the patient. Rather, it's because we need to see these patients early to ensure all treatment options stay open and we intervene at the most optimal time," says Kendra J. Grubb, MD, MHA, FACC, surgical director of the Emory University Structural Heart and Valve Center.
Even the delineation of degenerative or functional MR isn't so simple, she says. In many cases, the MR starts as degenerative and moves to a mixed etiology. The degenerative process often starts in the valve but progresses to become more functional, at which point the patient becomes more symptomatic.
"If you ignore degenerative or primary MR long enough, it becomes functional," says Grubb. "But waiting for a patient with a prolapsing leaflet to develop more severe secondary pathology, reduced ejection fraction and symptoms before advancing them up the care ladder can be dangerous."
For some, a surgical valve consult can seem counterintuitive in a patient with a completely normal looking valve, particularly as there aren't good data to say that surgical valve repair or replacement improves survival in patients with functional MR, adds Grubb, stressing this doesn't mean the patient will be going for surgery immediately.

Kendra J. Grubb, MD, MHA, FACC
"We know it's progressive and we know the patients will end up with worsening HF. As this happens and their ventricle deteriorates, they may move from a patient with treatment options to a 'no option' patient and we've missed the opportunity to help."
Adds Makkar, "Only 50% of patients, at best, with functional MR are ever sent for advanced therapies or interventions. They're being cared for medically, waiting for symptoms to get worse, which essentially means we're waiting for the ventricle to start to fail. When that happens, it's really too late."
To Intervene or Not to Intervene?
Before a discussion of whether a patient is best served by transcatheter or surgical mitral valve intervention, Makkar suggests, there needs to be more consensus on whether to treat functional MR invasively at all. Some, he says, are reluctant to treat the valve directly when the issue stems from the ventricle. It's akin to replacing the tires on a car that has a bent frame.
"It's important for clinicians to understand that it's the regurgitation itself that is so important here – it hampers medical management but it also leads to further LV dilatation, which leads to more regurgitation – a vicious cycle. We know from the COAPT trial that TEER reduces rehospitalization and mortality. So it's really a shame to not offer this treatment to patients for whom it is indicated," Makkar says.
COAPT patients who underwent TEER had lower mortality at thee years (42.8% vs. 55.5% for GDMT alone; HR, 0.67; p=0.001) and sustained three-year improvements in MR severity, quality-of-life measures and functional capacity.2 Even among the 58 patients assigned to GDMT alone who crossed over to TEER in the trial, the subsequent composite rate of mortality or HF hospitalization was reduced compared with those who continued on GDMT alone (adjusted HR, 0.43; p=0.006).
"The COAPT trial took a long time to enroll because of the fastidious requirements around GDMT, but with that trial, we have clear data – now with three years of follow-up – that TEER plus GDMT is better than GDMT alone for the treatment of functional MR," says Makkar.
Makkar notes there have been some big changes in GDMT for HF since COAPT, namely sacubitril/valsartan and the SGLT2 inhibitors: "two amazing additions to GDMT that HF specialists now have in their armamentarium," he says.
"I think these drugs may be dampening enthusiasm for TEER a bit. But what I've seen in my practice, and I've heard this from HF specialists too, is that sometimes a TEER procedure can actually help optimize medical therapy, because it can help to address the hypotension that patients develop with GDMT. Implanting a MitraClip in these patients often fixes the issue of hypotension and allows being more aggressive with medical therapy," says Makkar.
Isida Byku, MD, FACC, from Emory University, calls it "pre-habing" patients so they qualify for a TEER procedure, and "re-habing" them after the procedure by adjusting their GDMT to capture the best possible outcomes (see sidebar).
Transcatheter or Surgical Repair?
Surgeons and interventional cardiologists readily agree there are some patients for whom a surgical mitral valve repair is the best option and others for whom TEER is most appropriate, says Vinod H. Thourani, MD, FACC, chief of cardiovascular surgery at Piedmont Heart Institute in Atlanta and the surgical director of the Marcus Valve Center of Excellence.
"For patients who have severe ischemic secondary MR and LV dysfunction who need coronary artery bypass grafting, there is no argument that they should undergo mitral valve surgery at the same time. We have data to support this," says Thourani.
"On the flip side, patients considered at high to prohibitive risk for surgery should go for TEER, assuming they meet the criteria." He also notes that patients with an ejection fraction <30% are unlikely to be surgical candidates.
For those in between, it's in the patient's best interest to be seen by a Heart Valve Team to determine the best course of action, he adds. The Heart Valve Team should, at a minimum, include a cardiac surgeon well versed in mitral valve surgeries, an interventional cardiologist adept in TEER, a HF specialist and an imaging specialist, says Thourani.
"We've found at Piedmont Heart Institute that having the surgeon and cardiologist assess the patient together in our mitral valve clinic – reviewing their current treatment, risk category and anatomy together – is what leads us to have optimal outcomes."
Different from patients with primary MR or who are under consideration for TAVR, prior to considering an advanced therapy, patients with functional MR should be assessed by a qualified HF specialist to make sure their GDMT is optimized.
"We have great outcomes after mitral valve surgery for primary, degenerative MR because the ventricle is normal and we fix the valve. So, you've put a new tire on a good car. These days in top valve centers this will likely mean a minimally invasive robotic surgical repair. But with functional MR, there is a larger discussion needed to understand the risks and benefits, and determine the best possible treatment," says Grubb.
The TEER Landscape: Devices, Data
Abbott's MitraClip has had a long run at the top of the transcatheter mitral valve implantation heap. The device, which replicates the Alfieri stitch operation and is usually performed with adjunctive ring annuloplasty, was first implanted in 2003 in a 55-year-old woman from Caracas, Venezuela. It obtained CE marking in Europe in 2008, was approved by the U.S. Food and Drug Administration in 2013, and now has been used in well over 100,000 patients.
Its closest competitor, the PASCAL system from Edwards Lifesciences, is likely to come to market within the next 12 to 18 months pending the results of the CLASP IID randomized trial which compared the MitraClip to the PASCAL device in primary MR. The CLASP IIF trial comparing the PASCAL device with MitraClip is still enrolling patients. There are also some mitral valve replacement options in development and coming within a year or two, like the Tendyne transcapical mitral valve replacement device (Abbott).
Two relatively recent developments are expected to gradually lead to more use of TEER: a January 2021 National Coverage Determination from the Centers for Medicare and Medicaid Services that includes TEER for secondary MR and the new 2020 ACC/AHA valvular heart disease guideline that upgraded the recommendation for TEER to Class 2a in both primary and secondary MR.1
Vinod H. Thourani, MD, FACC
Gone are the dark and confusing days after the presentations of the COAPT and MITRA-FR trials when many wondered if TEER's days were numbered.
As a quick reminder, the COAPT trial was first presented in September 2018 and showed marked clinical benefit in terms of survival, hospitalization, symptoms and quality of life from TEER plus medical therapy vs. medical therapy alone in patients with HF and secondary MR and persistent symptoms despite optimization of GDMT.3
In contrast, in the MITRA-FR trial, which had been presented one month earlier, TEER failed to show benefit over medical therapy.4 A closer look revealed that MITRA-FR enrolled patients with a greater degree of LV enlargement and less severe MR (mean effective regurgitant orifice area 0.31 cm2 vs. 0.41 cm2 for COAPT). Both trials used the MitraClip.
The enrollment criteria for COAPT – LVEF between 20% and 50%, LV end systolic diameter ≤70 mm Hg and persistent symptoms (NYHA class II, III or IV HF) while on optimal GDMT – are the current standard selection criteria for TEER for functional MR.
The next-generation MitraClip G4 system is now approved in the U.S. for commercial use. The new MitraClip device overcomes limitations found in earlier iterations, comes in four different sizes, and incorporates the ability to continuously monitor left atrial pressure for real-time hemodynamic monitoring during the procedure. In a small study, use of the MitraClip G4 was associated with excellent reduction in MR to ≤2+ in 96.6% of patients at 30 days.5
Collaboration and Teamwork
In the end, the experts are requesting collaboration. "I think it's fair to say the medical and surgical management of functional MR is a very complex and dynamic process that requires specialists in surgical and transcatheter valve procedures, imaging and heart failure, along with general cardiologists who we count on to diagnose the disease and help to manage the GDMT on a daily basis. It's a complex valve and a complex disease, but our ability to manage it has improved dramatically in recent years," says Thourani.
Beyond COAPT: Finessing Patient Selection
As an early career interventionalist at Emory University Hospital, Isida Byku, MD, FACC, is interested in how patient selection and risk assessment for TEER will evolve over the next several years.
"We have a subanalysis from COAPT along with other reviews that have shown us that the existence of moderate-to-severe right ventricular (RV) dysfunction and moderate-to-severe tricuspid regurgitation (TR) portend a poor prognosis in any patient treated with mitral valve therapy," says Byku. There are questions we haven't yet worked out: How do we differentiate TR? Is it a marker of RV or a sign of temporary volume pressure overload of the RV in the presence of significant MR? How do we best intervene?
These are important questions, she adds, because up to 30% of patients have concomitant MR and TR – both LV and RV dysfunction. Like severe MR, severe TR decreases survival and quality of life and progression of TR is common, particularly in patients undergoing mitral valve surgery.
Clinical outcomes with isolated tricuspid surgery are poor, but outcomes after combined mitral surgery plus tricuspid annuloplasty are promising, as shown in the CTSN trial presented by Gammie, et al., at the AHA Scientific Sessions in 2021.

Isida Byku, MD, FACC
She thinks solutions will come from working closely with HF specialists to tease out best medical therapies and how GDMT might be used to "pre-hab" a patient to make them suitable for TEER, but also to "post-hab" them after TEER to optimize outcomes.
Also, rather than relying just on echocardiography, which is notoriously inaccurate in assessing RV function, but also perhaps using continuous hemodynamic monitoring in these patients.
"Can we optimize things using some of these new HF medications and continuous monitoring where we can see some reversibility in the degree of TR and in the degree of RV dysfunction? And bring down the RV pressure such that maybe we make a patient who walked into the office a non-COAPT patient as close to being a COAPT patient as possible?"
COAPT excluded patients with tricuspid valve disease requiring surgery and those with severe pulmonary hypertension and moderate-to-severe RV dysfunction. Less than 1% of the COAPT patients had moderate or greater TR.
"Most of the patients who walk through our door are not suitable for COAPT," says Byku. But if we can flip them to being COAPT-like and offer them the clinical benefits of TEER, she says, the potential is huge. But this requires good teamwork before, during and after the procedure between HF specialists and the surgical and transcatheter interventionalists.
This article was authored by Debra L. Beck, MSc.
References
- Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2021;77:e25-e197.
- Mack MJ, Lindenfeld J, Abraham WT, et al. 3-Year outcomes of transcatheter mitral valve repair in patients with heart failure. J Am Coll Cardiol 2021;77:1029-40.
- Stone GW, Lindenfeld J, Abraham WT, et al. Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med 2018;379:2307-18.
- Obadia JF, Messika-Zeitoun D, Leurent G, et al. Percutaneous repair or medical treatment for secondary mitral regurgitation. N Engl J Med 2018;379:2297-306.
- Chakravarty T, Makar M, Patel D, et al. Transcatheter edge-to-edge mitral valve repair with the MitraClip G4 System. JACC Cardiovasc Interv 2020;13:2402-14.
Clinical Topics: Arrhythmias and Clinical EP, Cardiac Surgery, Cardiovascular Care Team, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Valvular Heart Disease, Implantable Devices, Aortic Surgery, Cardiac Surgery and Arrhythmias, Cardiac Surgery and Heart Failure, Cardiac Surgery and VHD, Novel Agents, Acute Heart Failure, Interventions and Imaging, Interventions and Structural Heart Disease, Echocardiography/Ultrasound, Mitral Regurgitation
Keywords: ACC Publications, Cardiology Magazine, Angiotensin Receptor Antagonists, Angiotensin-Converting Enzyme Inhibitors, Aortic Valve, Atrial Pressure, Cardiac Resynchronization Therapy, Cardiologists, Cardiology, Cardiomyopathies, Centers for Medicare and Medicaid Services, U.S., Chordae Tendineae, Consensus, Coronary Artery Bypass, Dilatation, Echocardiography, Europe, Fatigue, Follow-Up Studies, Heart Failure, Heart Valve Diseases, Heart Ventricles, Hemodynamic Monitoring, Hospitalization, Hospitals, Hypotension, Los Angeles, Medicare, Midazolam, Middle Aged, Mineralocorticoid Receptor Antagonists, Mitral Valve, Mitral Valve Insufficiency, Noncommunicable Diseases, Papillary Muscles, Patient Selection, Pharmaceutical Preparations, Prognosis, Quality of Life, Risk Assessment, Robotic Surgical Procedures, Shame, Sodium-Glucose Transporter 2 Inhibitors, Stroke Volume, Surgeons, Surgical Instruments, Transcatheter Aortic Valve Replacement, Tricuspid Valve Insufficiency, United States Food and Drug Administration, Universities, Valsartan, Venezuela, Ventricular Dysfunction, Right
< Back to Listings