Focus on EP | Atrial Fibrillation: Current Evidence For Management

In the last several years, atrial fibrillation (AFib) management has rapidly evolved from a reactive strategy favoring rate control to a proactive strategy emphasizing sinus rhythm maintenance.
This paradigm shift was catalyzed by several landmark events leading up to this decade. In 2018, the U.S. Food and Drug Administration (FDA) approved the first AFib detection algorithm for the Apple Watch, providing individuals with a popular, wearable consumer device that could easily screen for AFib without the need for a prescription rhythm monitor.
The CABANA trial results in 2019 challenged the AFFIRM trial notion that rhythm control provided no significant benefit over rate control in AFib.1 Lastly, in 2020, the COVID-19 pandemic led to a greater recognition of clinical symptoms overlapping with AFib (shortness of breath, palpitations, chest discomfort, etc.) as well as the understanding that COVID-19 infection could serve as a trigger for AFib.
Against this backdrop of increasing AFib awareness and the desire to improve AFib outcomes, the past two years have witnessed significant research advancements in the areas of remote monitoring, lifestyle modification, and substrate modification with AFib ablation. This month's "Focus on EP" column highlights some of these advances, ranging from the growing role of smart devices to AFib ablation. Look for even more on these topics in future issues of Cardiology in the coming months, including a deeper dive into AFib ablation vs. medical management in terms of practice considerations, payment and more.
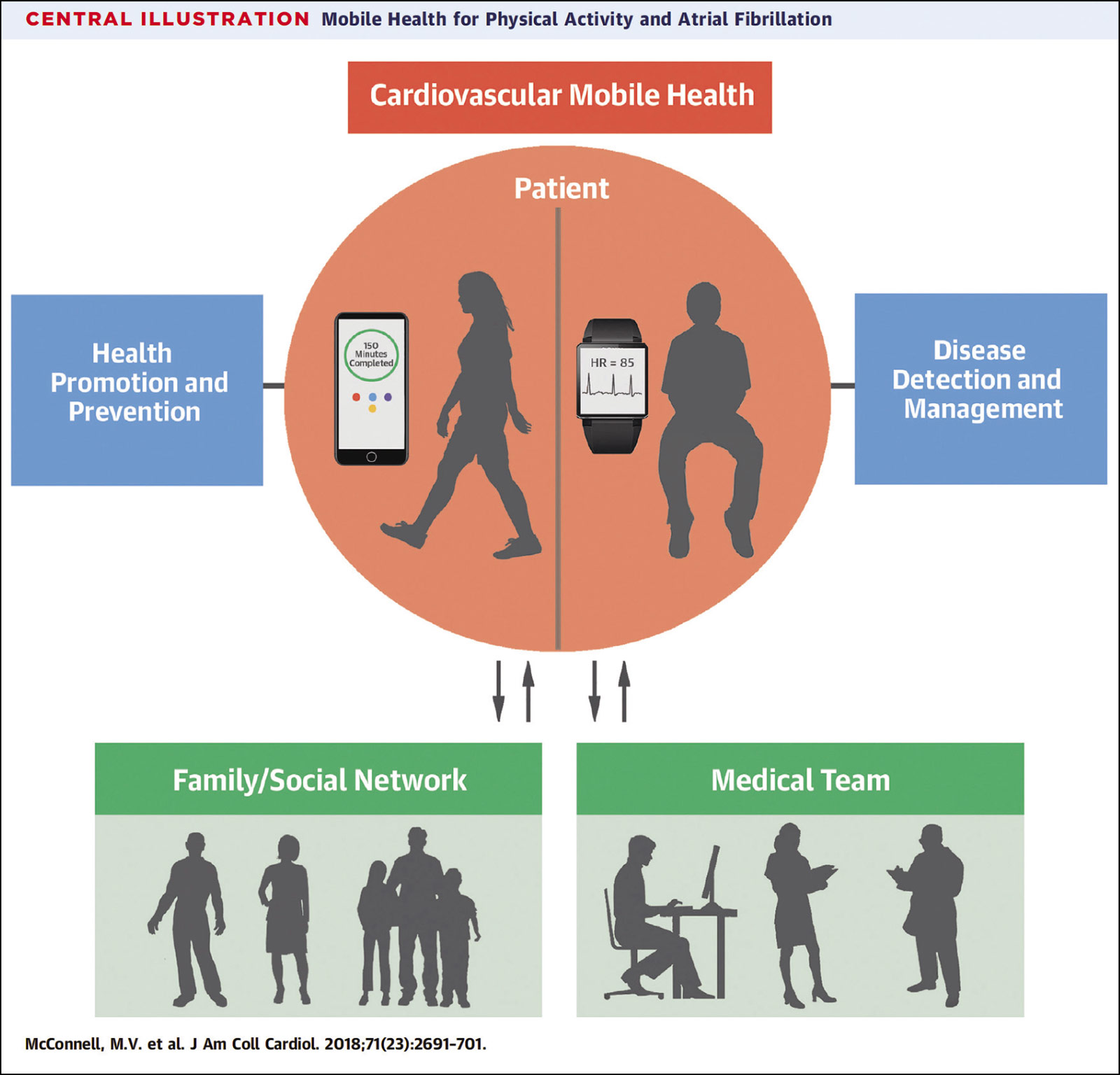
The Growing Role of Smart Devices

With the rise of smart devices, patients are now empowered to diagnose and track their AFib burden with far greater convenience than before. This expanded accessibility has had a profound impact on AFib screening and risk reduction.
The eBRAVE-AF trial randomized 5,501 AFib-free patients (median age, 65 years; median CHADS-VASc score, 3) to digital screening of AFib using an app on their smartphone or to AFib screening by usual care. At six months of follow-up, patients in the digital screening group were more than twice as likely to be diagnosed with new-onset AFib (necessitating oral anticoagulation initiation), compared with patients in the usual care group (1.33% vs. 0.63%, p=0.01).2
The mobile AFib App (mAFA)-II trial randomized 1,261 patients with AFib to a structured, mAFA-guided management program based on the ABC (Atrial fibrillation Better Care) pathway or to usual care (Figure). At 12 months of follow-up, patients in the mAFA program experienced a nearly 50% reduction in the composite outcome of ischemic stroke/systemic thromboembolism, death and rehospitalization, compared with patients in the usual care group (6.9% vs. 13.6%, p<0.001).3
Although technically not a smart device, the implantable loop recorder (ILR) is the only device to provide continuous but remote rhythm monitoring. The LOOP trial randomized 6,004 AFib-free patients (mean age, 74.7 years; mean CHADS-VASc score, 4) to AFib screening with ILR or with usual care. At a median 64.5 months of follow-up, nearly threefold as many patients were diagnosed with new AFib in the ILR group compared with the usual care group (31.8% vs. 12.2%, p<0.001).
Oral anticoagulation, for AFib episodes lasting six minutes or longer, was initiated more than twice as often in the ILR group compared with the usual care group (29.7% vs. 13.1, p<0.01). However, there was no significant difference in the occurrence of stroke or systemic embolism between the ILR group and the usual care group (4.5% vs. 5.6%, p=0.11).4
Lifestyle Still Matters

There is increasing recognition that AFib episodes can be triggered by suboptimal lifestyle patterns and potentially suppressed by healthy lifestyle behaviors.
The HOLIDAY Monitors study (abstract presented at ACC.21) examined the impact of alcohol consumption on AFib burden in 100 patients with paroxysmal AFib who underwent continuous rhythm monitoring for one month. The results revealed that one glass of wine, beer or equivalent alcoholic beverage, doubled the risk of an AFib episode occurring in the subsequent four-hour period (odds ratio, 2.02; p<0.002). For every 0.1% increase in the blood alcohol concentration in the previous 12 hours, the risk of developing an AFib episode increased by 38% (odds ratio, 1.38; p=0.024).5
The ACTIVE-AF trial (abstract presented at ESC Congress 2021) randomized 120 patients with paroxysmal or persistent AFib and <60 minutes of baseline weekly physical activity to either a structured exercise program consisting of supervised physical activity with gradual escalation to 210 minutes of weekly physical activity or to education-only exercise program that recommended 150 minutes of weekly physical activity.
At 12 months of follow-up, patients in the structured exercise cohort were twice as likely to be free of AFib compared with the control cohort (40% vs. 20%, p=0.018) and experienced an estimated 33% reduction in AFib symptom severity (p=0.041).6
The SLEEP-AF trial randomized 24 patients with paroxysmal or persistent AFib and moderate obstructive sleep apnea (OSA) to continuous positive airway pressure (CPAP) or no therapy. Compliance in the CPAP group was high (69% device usage, mean usage/day 268 minutes). All patients underwent invasive right atrial mapping at baseline and at six months or later.
In the no-therapy group, repeat atrial mapping demonstrated a decline in average bipolar voltage (2.16 vs. 1.94 mV, p=0.07), increase in the proportion of complex points (7.49% vs. 11.93%, p<0.001) and no change in average conduction velocity (0.68 vs. 0.69 m/s, p=0.86).
In the CPAP group, repeat atrial mapping demonstrated no significant change in the average bipolar voltage (2.17 vs. 2.30 mV, p=0.58) and proportion of complex points (9.17% vs. 8.87%, p=0.82) but a significant improvement in average conduction velocity (0.67 vs. 0.86 m/s, p=0.005).7 These results suggest that CPAP use in OSA not only stalls the progression of adverse AFib remodeling but can also lead to reverse remodeling.
AFib Ablation Moves to the Forefront

As a result of several recent landmark trials, there is no longer a question of "if" AFib ablation should be performed but rather "when" and "how" it should be performed. The EAST-AFNET 4 trial randomized 2,789 patients with recent-onset AFib (≤12 months from diagnosis) to either early rhythm control (ERC) or usual care. Of note, 20% of the patients in the ERC group underwent AFib ablation whereas only 7% of the patients in the usual care group underwent AFib ablation.
The investigation was terminated early after a median follow-up of 5.1 years due to efficacy in the ERC group: the composite outcome of cardiovascular death, stoke and hospitalization for heart failure or acute coronary syndrome was significantly reduced in the ERC group compared with the usual care group (3.9% vs. 5.0%, p=0.005). There was no significant difference in the composite safety outcome of stroke, death and serious adverse events between the ERC group and the usual care group (16.6% vs. 16%, p>0.05).8
The EAST-AFNET 4 trial was the first randomized controlled trial to overturn the long-held AFFIRM trial dogma that rhythm control had no clinical benefit compared with rate control. Published simultaneously, the EARLY-AF and STOP-AF trials randomized 303 patients and 203 patients with paroxysmal AFib, respectively, to pulmonary vein isolation (PVI) with cryoballoon or antiarrhythmic drug therapy.
At 12 months of follow-up in the EARLY-AF trial, patients who underwent cryoballoon ablation experienced a significantly lower rate of atrial arrhythmia recurrence, compared with patients who underwent drug therapy (42.9% vs. 67.8%, p<0.001). There was no significant difference in the rate of serious adverse events between groups (3.2% vs. 4.0%, p>0.05).9
At 12 months of follow-up in the STOP-AF trial, patients who underwent cryoballoon ablation were more likely to be free of atrial arrhythmia recurrence, compared with patients who underwent drug therapy (74.6% vs. 45%, p<0.001). There was also no significant difference in the rate of serious adverse events between groups (14% vs. 14%, p>0.05).10 These two trials further solidified the value of PVI, particularly with cryoballoon ablation, to achieve rhythm control in patients with paroxysmal AFib.
Moving beyond PVI, the VENUS, ERASE-AF, and CONVERGE trials explored additional ablation targets beyond the pulmonary veins (PVI+) in patients with persistent AFib. The VENUS trial randomized 350 patients with persistent AFib to PVI or PVI with ethanol infusion of the Vein of Marshall.
At 12 months of follow-up, patients who underwent additional ethanol infusion of the Vein of Marshall experienced a greater freedom from atrial arrhythmias compared with patients who underwent PVI only (49.2% vs. 38%, p=0.04).11
The ERASE-AF trial randomized 342 patients with persistent AFib to PVI or PVI with additional isolation of five discrete left atrial wall segments (posterior, inferior, septal, lateral and anterior) based on the presence of low-voltage myocardium. At 12 months of follow-up, patients who underwent additional wall isolation experienced less atrial arrhythmia recurrence compared with patients who only underwent PVI ablation (35% vs. 50%, p=0.006).12
The CONVERGE trial randomized 153 patients with persistent AFib to endocardial PVI with a left atrial roof line or to endocardial PVI with endocardial and epicardial posterior wall isolation (via a surgical pericardial access system).
At 12 months of follow-up, patients who underwent additional endocardial and epicardial posterior wall isolation experienced greater freedom from atrial arrhythmias compared with patients who only underwent PVI ablation with roof line (67.7% vs. 50%, p=0.013).13 In all three trials, there was no significant difference in adverse events between the control and experimental groups.
The Future of AFib Management

Although these studies have advanced the field of AFib, it is unclear whether any will leave any lasting impression. New smart devices and detection algorithms emerge each year, leaving older iterations obsolete. Poor lifestyle habits can be hard to change, and hardly any of the recent recommendations (consume less alcohol, improve sleep quality and exercise more) are novel.
Even current ablation technologies are at risk of being replaced if pulsed field ablation, which only recently earned a CE Mark in Europe and has yet to achieve FDA approval in the U.S., proves to be as effective and safe as it is rumored to be.
Despite the uncertainty, it is certainly an exciting time in AFib management.

This article was authored by Edward Chu, MD, FACC, (@Ed_Chu_MD), an electrophysiology attending physician in Miami, FL.
References
- Packer DL, Mark DB, Robb RA, et al; CABANA Investigators. Effect of catheter ablation vs antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation: The CABANA randomized clinical trial. JAMA 2019;321:1261-74.
- Rizas KD, Freyer L, Sappler N, et al. Smartphone-based screening for atrial fibrillation: a pragmatic randomized clinical trial. Nat Med 2022;28:1823-30.
- Guo Y, Lane DA, Chen Y, et al; mAF-App II Trial investigators. Regular bleeding risk assessment associated with reduction in bleeding outcomes: The mAFA-II randomized trial. Am J Med 2020;133:1195-1202.e2.
- Svendsen JH, Diederichsen SZ, Højberg S, et al. Implantable loop recorder detection of atrial fibrillation to prevent stroke (The LOOP Study): A randomised controlled trial. Lancet 2021;23:398:1507-16.
- HOLIDAY Monitors: Alcohol Consumption Significantly Increases Risk of AFib Episode. ACC.21 News Story. May 12, 2019. Available here.
- ACTIVE-AF: A randomised controlled trial of exercise training in AF patients. ESC Congress 2021. Available here.
- Nalliah CJ, Wong GR, Lee G, et al. Impact of CPAP on the atrial fibrillation substrate in obstructive sleep apnea: The SLEEP-AF study. JACC Clin Electrophysiol 2022;8:869-77.
- Kirchhof P, Camm AJ, Goette A, et al; EAST-AFNET 4 Trial Investigators. Early rhythm-control therapy in patients with atrial fibrillation. N Engl J Med 2020;383:1305-16.
- Andrade JG, Wells GA, Deyell MW, et al; EARLY-AF Investigators. Cryoablation or drug therapy for initial treatment of atrial fibrillation. N Engl J Med 2021;384:305-15.
- Wazni OM, Dandamudi G, Sood N, et al; STOP AF First Trial Investigators. Cryoballoon ablation as initial therapy for atrial fibrillation. N Engl J Med 2021;384:316-24.
- Valderrábano M, Peterson LE, Swarup V, et al. Effect of catheter ablation with vein of marshall ethanol infusion vs catheter ablation alone on persistent atrial fibrillation: The VENUS randomized clinical trial. JAMA 2020;324:1620-8.
- Huo Y, Gaspar T, Schönbauer R, et al. Low-voltage myocardium-guided ablation trial of persistent atrial fibrillation. NEJM Evidence Published Oct. 19, 2022;1(11). Available here.
- DeLurgio DB, Crossen KJ, Gill J, et al. Hybrid convergent procedure for the treatment of persistent and long-standing persistent atrial fibrillation: Results of CONVERGE clinical trial. Circ Arrhythm Electrophysiol 2020;13:e009288.
Clinical Topics: Acute Coronary Syndromes, Anticoagulation Management, Arrhythmias and Clinical EP, COVID-19 Hub, Diabetes and Cardiometabolic Disease, Heart Failure and Cardiomyopathies, Prevention, Anticoagulation Management and ACS, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Acute Heart Failure, Exercise, Sleep Apnea
Keywords: ACC Publications, Cardiology Magazine, Arrhythmias, Cardiac, COVID-19, Wearable Electronic Devices, Acute Coronary Syndrome, Heart Failure, Anticoagulants, Exercise, Sleep Apnea, Central
< Back to Listings