Peripheral Matters | Primary Effort Thrombosis: A Primer For the General Cardiologist

"I can't bat or swing – my right arm is swollen!"
He was a 19-year-old man, an all-star high school baseball player who presented for evaluation of sudden onset worsening right arm swelling and pain. His symptoms were exacerbated with movements such as throwing a baseball, batting or hyperextension of his right arm. On physical examination, his right upper extremity pulses (radial, ulnar, brachial) were normal.
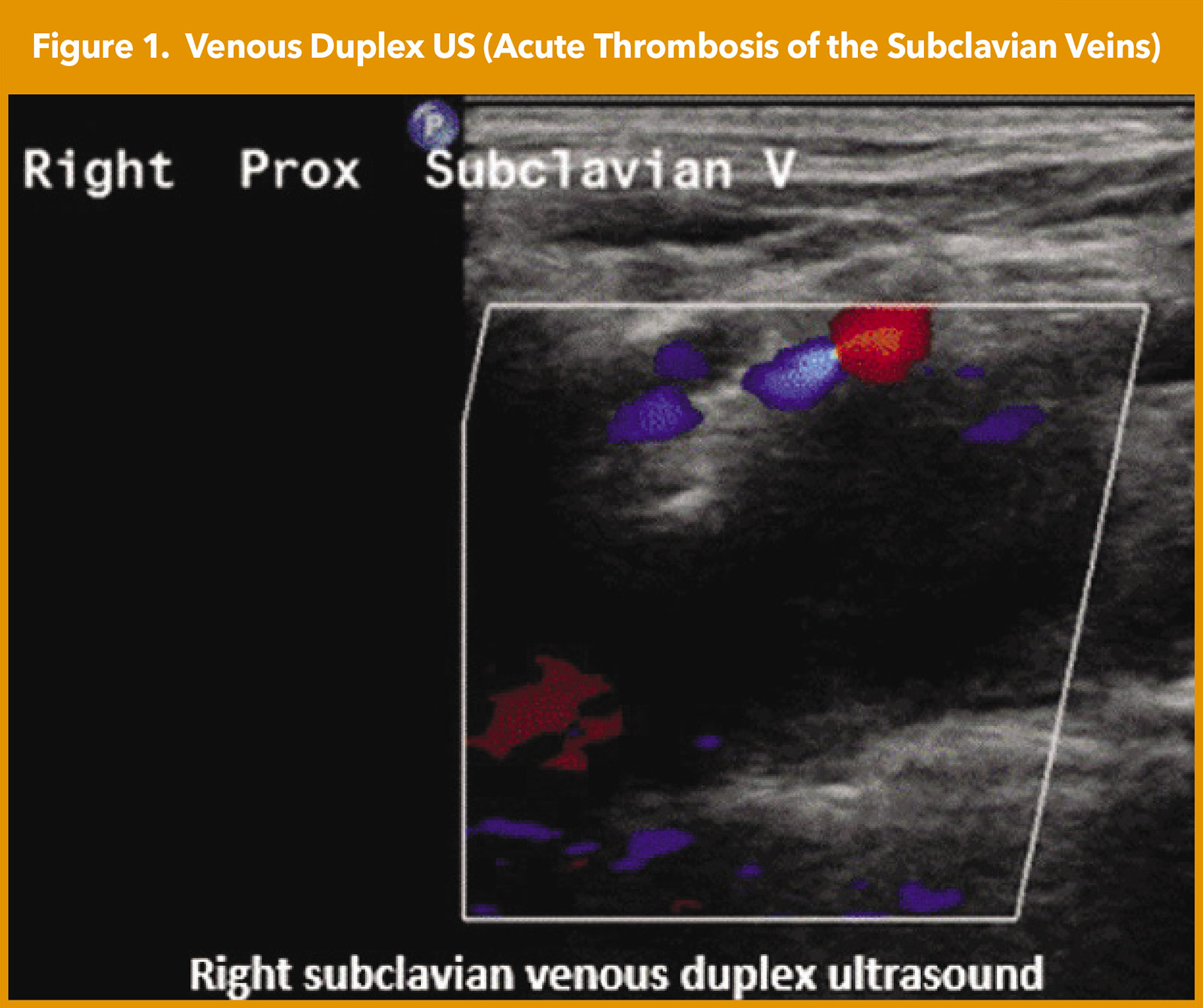
However, his right radial artery pulse was absent with right arm abducted, rotation of his head to the right and extension of his neck. His right upper chest wall revealed prominent superficial veins (Figure 1). His right upper arm circumference was approximately 3.5 cm larger than his left upper arm. Labs revealed an elevated D-dimer of 1,183 mg/L. His hypercoagulability lab panel was unremarkable. Venous duplex US of his right upper extremity revealed an acute thrombosis of the axillary-subclavian vein (Figure 1).
Based on the clinical presentation, what is your diagnosis and next step?
- Lymphatic obstruction, further testing needed
- Superior vena cava syndrome, refer for catheter-directed thrombolysis (CDT)
- Effort thrombosis, refer for CDT
- Unclear diagnosis, further diagnostic testing needed
Definition, Epidemiology and Pathophysiology
Thoracic outlet syndrome (TOS) refers to compression of structures coursing between the thoracic outlet and the axilla.1 There are three types of TOS: neurogenic (95%), venous (4%) or arterial (1%).2 Three types of venous TOS exist: primary "effort thrombosis," secondary subclavian vein thrombosis and intermittent/positional obstruction. Here the focus is primary effort thrombosis also known as Paget-Schroetter Syndrome (PSS).
PSS refers to compression and thrombosis of the axillary-subclavian vein from chronic, repetitive upper extremity exercise/activity. PSS usually occurs due to mechanical compression of the subclavian vein by structures in the thoracic outlet. It is relatively rare and accounts for 1-4% of all venous thromboembolism.3 Although TOS is generally more common in women with a female:male ratio of 4:1, PSS most commonly affects men in their early 30s, with a male:female ratio of 2.1:1.1
Athletes in sports such as weightlifting, volleyball, javelin throwing, swimming or baseball, or workers who perform repetitive overhead arm activity are most commonly at risk for PSS. It is thought to be triggered by repetitive strenuous interaction between the upper extremity venous system and the thoracic outlet structures. The axillary vein becomes the subclavian vein as it moves over the first rib and goes under the clavicle. The subclavian vein passes through the thoracic outlet to reach the internal jugular vein.
Repetitive upper extremity activity leads to hypertrophy of the anterior scalene and subclavius muscles and/or costoclavicular ligament hypertrophy which compresses the vein within the thoracic outlet.4 Chronic vein compression (with arm abduction) consequently leads to venous endothelial cell damage, inflammation, venous stasis, venous hypertension and eventual thrombosis of the axillary-subclavian vein.
Clinical Presentation and Diagnosis
Diagnosis is usually validated by history and physical examination and confirmed with noninvasive imaging. Symptoms usually present within 24 hours of the trigger physical activity. Usually, the dominant upper extremity is affected. Symptoms include upper extremity swelling/heaviness, upper extremity pain, chest pain, and engorged superficial and collateral veins may be seen across the shoulder, chest or neck.2
Occasionally, the thrombosed vein can be palpated in the axilla. Duplex US is the imaging modality of choice, with >80% sensitivity and specificity.5 If duplex US is inconclusive, other imaging tests can be performed such as contrast venography, and CT or MR venography. D-dimer levels may be elevated. Routine thrombophilia workup and routine malignancy screening are not typically recommended in most cases.
Management of PSS
The goals of therapy are to relieve symptoms and prevent complications and obviate recurrence. Thrombus burden reduction to reestablish vessel patency and thoracic outlet decompression are the two main principles of the available treatment strategies. Supportive care with warm compresses, upper extremity elevation and analgesia help to relieve symptoms. Therapeutic anticoagulation should be initiated expeditiously following definitive diagnosis.
Endovascular therapy (pharmacologic CDT or mechanical thrombectomy) should be considered for venous recanalization.6 The goal of endovascular therapy is to facilitate elimination/reduction of the thrombus burden, minimize endothelial cell injury and reestablish venous flow.7
Venous stenting is not recommended as studies have shown stenting of a nondecompressed costoclavicular junction is associated with stent deformation, stent fracture and rethrombosis. However, not all institutions may have endovascular capabilities to perform CDT before surgical decompression.8
The definitive therapy is surgical decompression of the thoracic outlet obstruction.9-11 Studies have shown that surgical decompression prevents recurrence/rethrombosis of the axillary-subclavian vein.10 Consequently, patients should be referred for surgical decompression whether or not endovascular therapy is technically successful.
Single-center studies indicate that treatment with thrombolysis and surgical decompression leads to favorable outcomes in >80% of patients. Surgical decompression usually involves resection of the first rib and constricting fibrous tissue and release of scalene muscle compression. The exact surgical approach is usually tailored to the anatomic abnormality present.
The exact timing for the surgical decompression is controversial. Limited data suggest that early surgical intervention within 14 days of diagnosis is associated with improved clinical outcomes including freedom from reocclusion and reintervention.12,13 In addition, the duration of anticoagulation therapy is controversial.
The 2021 CHEST anticoagulation guideline recommends anticoagulation for three months in patients with acute upper extremity deep vein thrombosis and no contraindications.14 It is not unreasonable to do a tailored approach using postoperative venogram to guide the duration of anticoagulation: if it shows patent veins and no further intervention is indicated, anticoagulation can be discontinued. If the postoperative venogram shows persistent stenosis or rethrombosis, recommend continuing anticoagulation, and consider repeat endovascular interventions with venogram +/- venoplasty.6
There are limited data regarding the benefit of long-term anticoagulation for patients with persistent venous occlusion.10 Also data are limited on posttreatment recurrence rates but it is inferred to be low. Compression of the contralateral vein has been reported, with varying incidence rates, ranging up to 60-70%.
Case Wrap-Up
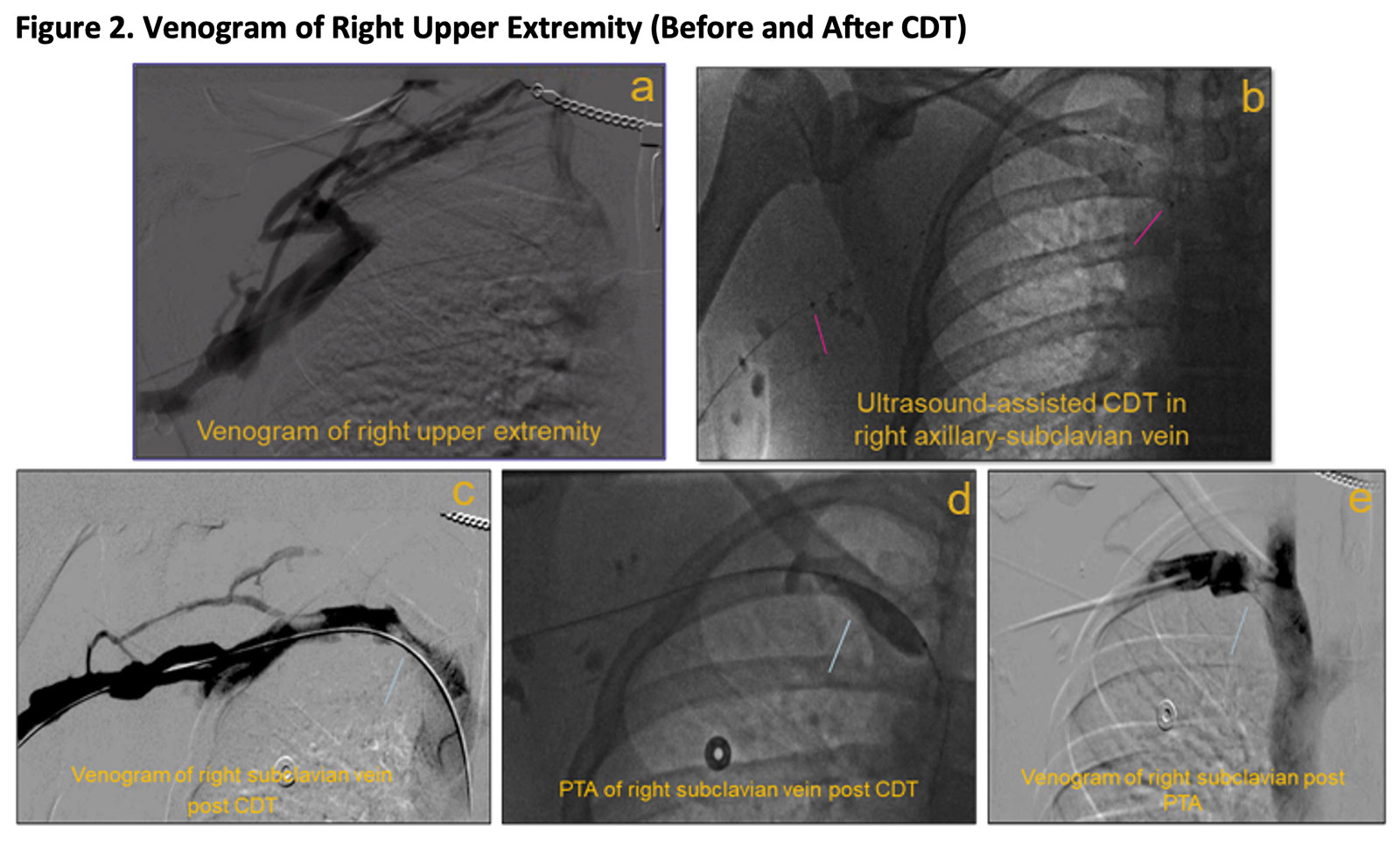
Therapeutic anticoagulation was initiated for our patient. He underwent US-assisted CDT in the interventional vascular suite (Figure 2). A re-look venogram performed several hours later revealed minimal residual thrombus, but improved flow in the right axillary-subclavian vein. Balloon angioplasty was performed of the axillary-subclavian veins with resolution of the thrombus.
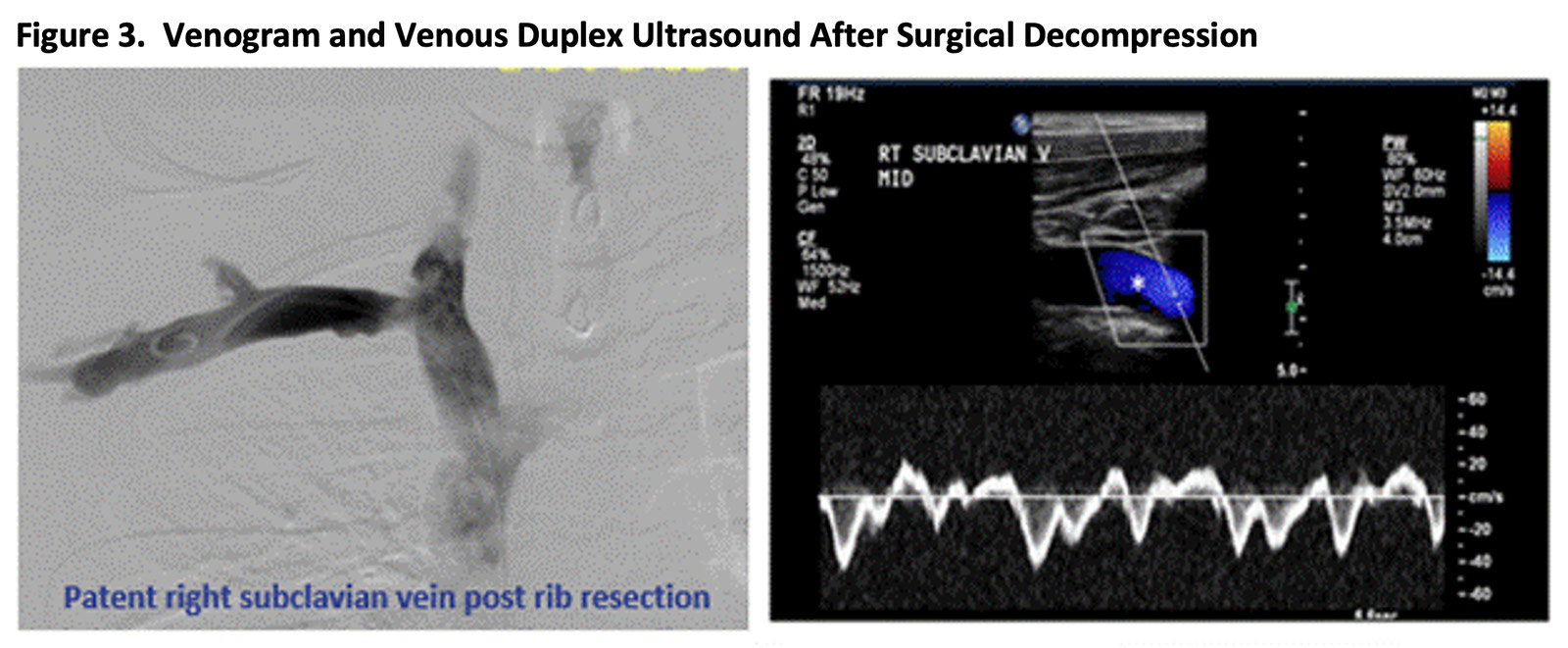
Therapeutic anticoagulation was resumed, and he was subsequently referred for definitive surgical TOS decompression. Duplex US and venogram performed one month later confirmed patent right axillary-subclavian vein and no residual thrombosis. Patient clinically fared very well with resolution of arm swelling and discomfort (Figure 3).
Question Recap: Based on the clinical presentation, your diagnosis and next step?
The correct answer is effort thrombosis and refer for CDT.

This article was authored by Nkechi Ijioma, MD, FACC, a vascular intervention fellow at Massachusetts General Hospital (MGH) in Boston, MA. She acknowledges and appreciates the expert content review by Eric A. Secemsky, MD, FACC, Beth Israel Deaconess Medical Center, Boston MA; Jose Emilio Exaire, MD, FACC, Baylor Scott & White Health, Temple TX; and Robert Schainfeld, DO, at MGH.
References
- Zucker EJ, Ganguli S, Ghoshhajra BB, et al. Imaging of venous compression syndromes. Cardiovasc Diagn Ther 2016;6:519-32.
- Hangge P, Rotellini-Coltvet L, Deipolyi AR, et al. Paget-Schroetter syndrome: treatment of venous thrombosis and outcomes. Cardiovasc Diagn Ther 2017;7(Suppl 3):S285-S290.
- Illig KA, Doyle AJ. A comprehensive review of Paget-Schroetter syndrome. J Vasc Surg 2010;51:1538-47.
- Moore R, Wei Lum Y. Venous thoracic outlet syndrome. Vasc Med 2015;20:182-9.
- Mall NA, Van Thiel GS, Heard WM, et al. Paget-schroetter syndrome: a review of effort thrombosis of the upper extremity from a sports medicine perspective. Sports Health 2013;5:353-6.
- Archie M, Rigberg D. Vascular TOS-creating a protocol and sticking to it. Diagnostics (Basel) 2017;7(2):34.
- Jubran JH, Towbin RB, Towbin A, et al. Paget-Schroetter syndrome. Applied Radiology 2021;50:56E-56H.
- Guzzo JL, Chang K, Demos J, et al. Preoperative thrombolysis and venoplasty affords no benefit in patency following first rib resection and scalenectomy for subacute and chronic subclavian vein thrombosis. J Vasc Surg 2010;52:658-62.
- Vazquez FJ, Paulin P, Poodts D, Gandara E. Preferred management of primary deep arm vein thrombosis. Eur J Vasc Endovasc Surg 2017;53:744-51.
- Urschel HC Jr., Patel HN. Surgery remains the most effective treatment for Paget-Schroetter syndrome: 50 years' experience. Ann Thorac Surg 2008;86:254-60.
- Urschel HC Jr., Razzuk MA. Neurovascular compression in the thoracic outlet: changing management over 50 years. Ann Surg 1998;228:609-17.
- Samoila G, Twine CP, Williams IM. The infraclavicular approach for Paget-Schroetter syndrome. Ann R Coll Surg Engl 2018;100:83-91.
- de Kleijn RJ C M F, Schropp L, Westerink J, et al. Timing of thoracic outlet decompression after thrombolysis for primary upper extremity deep venous thrombosis: A systematic review. Ann Vasc Surg 2020;66:654-61.
- Stevens SM, Woller SC, Baumann Kreuziger L, et al. Antithrombotic therapy for VTE disease: Second update of the CHEST guideline and expert panel report. Chest 2021;160:e545-e608.
Clinical Topics: Cardiac Surgery, Diabetes and Cardiometabolic Disease, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Prevention, Pulmonary Hypertension and Venous Thromboembolism, Sports and Exercise Cardiology, Vascular Medicine, Cardiac Surgery and Heart Failure, Pulmonary Hypertension, Interventions and Imaging, Interventions and Vascular Medicine, Hypertension, Sports and Exercise and Imaging
Keywords: ACC Publications, Cardiology Magazine, Aneurysm, Hypertension, Pulmonary, Diagnostic Imaging, Cardiac Surgical Procedures, Sports
< Back to Listings