Focus on Intervention | Weaning of Mechanical Circulatory Support For Patients With Cardiogenic Shock

Cardiogenic shock remains the most feared and deadly complication of acute myocardial infarction. In patients who develop cardiogenic shock, there remains a >40% mortality. Mechanical circulatory support (MCS) devices are indicated for patients who suffered cardiogenic shock and who have been on two or more inotropic therapies with hemodynamic compromise.
Yet, in certain cases, prolonged MCS might be required, especially in patients with florid cardiogenic shock that requires prolonged support for the heart to recover due to the unintended consequence of continued hemodynamic instability.
The National Cardiogenic Shock Initiative (NCSI) was launched using a standardized protocol to understand the early hemodynamic changes associated with cardiogenic shock and implement MCS as early as possible. The NCSI showed decreased mortality from STEMI complicated with cardiogenic shock through the early and routine use of invasive hemodynamic monitoring and early delivery of MCS, thus limiting device-related complications.
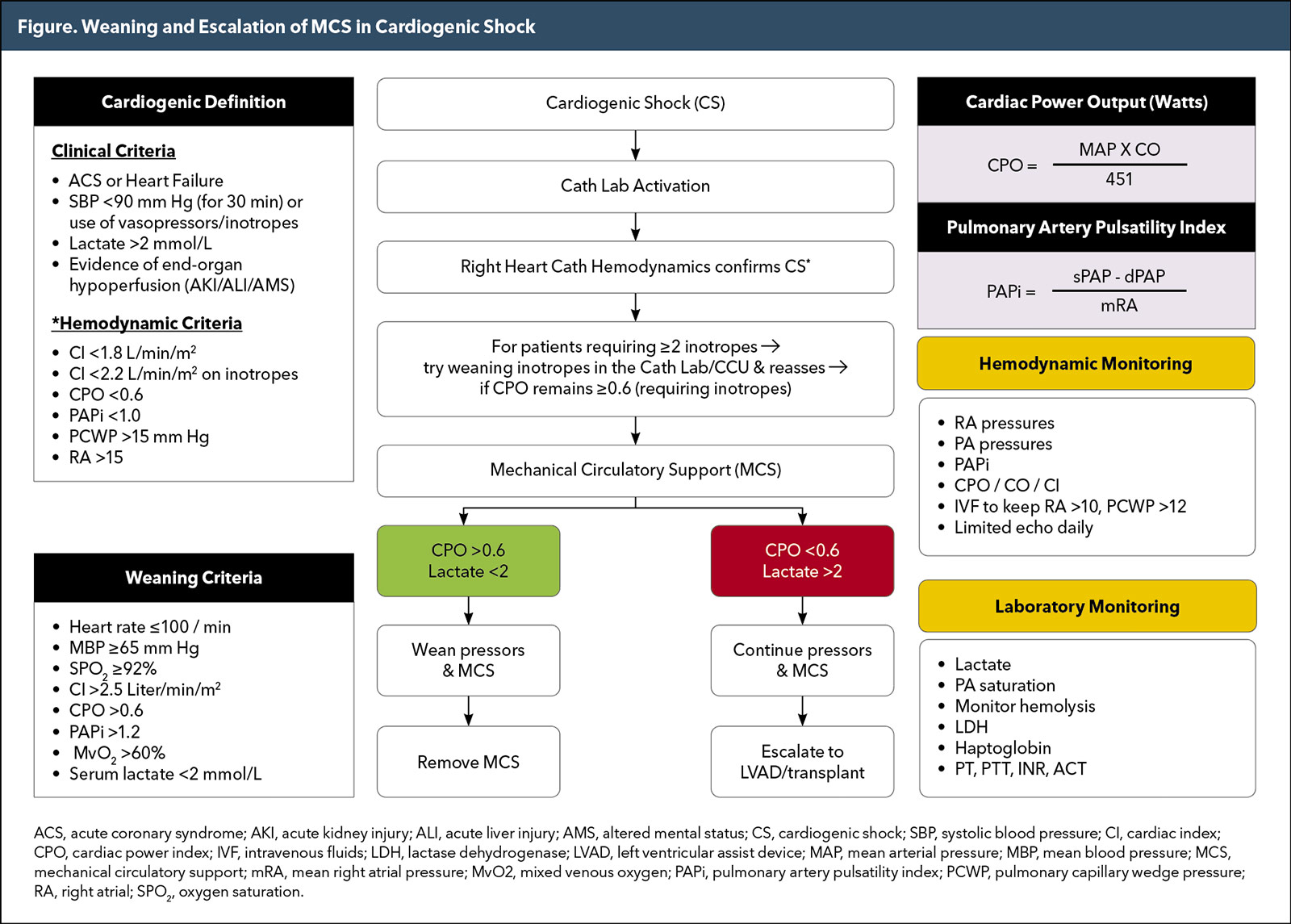
Given the importance of hemodynamic assessment for the patient presenting with cardiogenic shock, invasive hemodynamic monitoring using a pulmonary artery (PA) catheter offers more data on the cardiac output (CO) and cardiac index (CI) compared with the left ventricular (LV) end-diastolic pressure. Indeed, PA catheters have been shown to improve outcomes in patients with cardiogenic shock when inserted early because they provide more hemodynamic evaluation of these patients, as well as guide escalation or weaning of MCS by providing real-time hemodynamic data. Furthermore, the cardiac power output (CPO) [(mean arterial pressure × CO)/451] has been shown to be the strongest hemodynamic correlate of mortality in these patients. Similarly, the pulmonary artery pulsatility index (PAPi) [(PA systolic pressure-PA diastolic pressure)/right atrial pressure] was another strong correlate of mortality in cardiogenic shock patients after LV MCS implantation.
Weaning the patient from MCS is usually at the discretion of the treating physician in the intensive care unit. Several protocols have been developed using multidisciplinary teams that include cardiology, critical care, anesthesia, cardiovascular surgery, pharmacy and nursing staff. Weaning of MCS should be performed in a step-by-step manner during which the level of device support is gradually reduced. There is no unified recommendation of vital signs and hemodynamic status for MCS weaning and the assessment and decision should be adjusted for each patient. Weaning or escalation should always be guided by hemodynamic parameters to evaluate not only for ongoing LV dysfunction but also right ventricle dysfunction. These assessments should be made at least twice daily to minimize any delay of escalation or transfer if warranted.
Shock patients often are on inotropic therapy as well as MCS in the early phases. However, while the heart is recovering the need for inotropic agents will decrease and can be weaned off. In general, it is preferred to have the patient on minimal inotropic or pressor agents before considering MCS weaning. Overall and while on full MCS support, the desired parameters at which weaning should be considered are heart rate ≤100 beats per minute and no more than 10-20% of baseline; mean blood pressure should remain ≥65 mm Hg and no less than 10-20 mm Hg of baseline; arterial saturation should remain ≥92% with no signs of respiratory distress; CI >2.5 liter/minute/meter2; CPO >0.6; PAPi >1.2; mixed venous oxygen (MvO2) >60%; serum lactate level <2 mmol/L. Once these parameters are reached, the patient is considered ready for MCS weaning (Figure).
When the patient's vitals, hemodynamic and metabolic parameters continue to be stable, it is recommended that the level of MCS support be decreased slowly while following the hemodynamic and metabolic parameters. At any stage, if serum lactate or hemodynamic parameters are abnormal, it is recommended that the patient return to full support and be re-evaluated in 24-48 hours since this indicates incomplete recovery from cardiogenic shock. In patients who do not meet the above criteria, MCS should continue for 48-72 hours. If there is no evidence of recovery, escalation of support or transfer to a left ventricular assist device or a transplant center is recommended.

This article was authored by M. Chadi Alraies, MD, FACC, medical director of the cardiac catheterization laboratory, cardiac rehabilitation, and interventional cardiology research at Detroit Medical Center, Harper University Hospital, in Michigan.
Clinical Topics: Cardiac Surgery, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Cardiac Surgery and Heart Failure, Acute Heart Failure, Interventions and Imaging, Angiography, Nuclear Imaging
Keywords: ACC Publications, Cardiology Magazine, Heart Failure, Angiography, Cardiac Surgical Procedures, Care Team, Patient Care Team

