From the Starting Line | Ushering in a New Decade: Consumer Wearable Devices in the 2020s

One Cardiologist (the Patient), One Wearable: Lifesaving!
It was June of 2019. Naomi, a cardiovascular medicine fellowship program director and associate professor of medicine, had just left the cardiology division's morning conference.
While walking to her office in the medical school, she developed moderate-intensity chest discomfort. She dismissed the chest discomfort, but it persisted.
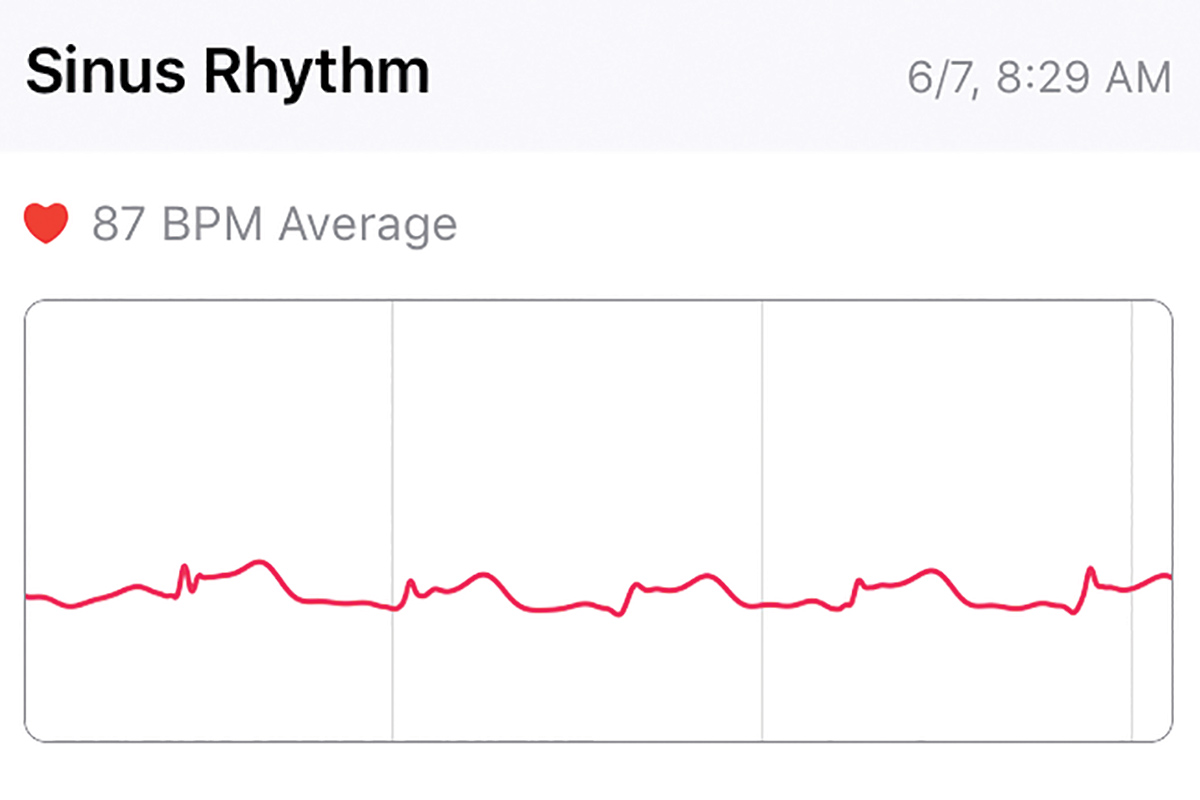
Then she turned to the Apple watch on her wrist, a recent purchase, for an ECG. In utter disbelief, she stared at an ST elevation on the single lead tracing (Figure 1).
Figure 1: Naomi's wearable device showing ST elevation
Scheduled to read inpatient echocardiograms that morning, Naomi surmised the fastest way for a 12-lead ECG was in the echo lab. Ten minutes later, she was holding hers showing an anterolateral ST elevation (Figure 2).
Figure 2: Naomi's 12-lead ECG showing acute anterolateral STEMI
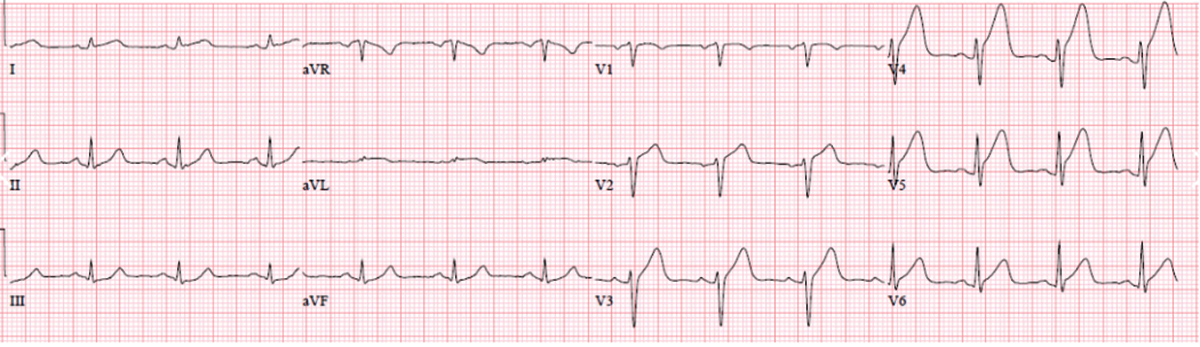
One of her cardiology fellows ran to the cath lab with the ECG. In minutes, an echo probe was on her chest wall and Naomi was staring at a wall motion abnormality in the distribution of the distal left anterior descending artery (LAD).
She contacted her husband, gave permission to the cardiology fellow to access her electronic health record (EHR), and signed the cardiac cath consent form. Twenty minutes later, the cath lab was ready.
Naomi remembers small things: the shock on the cardiology fellows' faces, the apologies of the nurse who prepped her groin for back-up femoral arterial access, and the occasional murmured conversation in the cardiac cath lab.
The coronary angiogram revealed an occluded mid LAD. The etiology of the occlusion wasn't immediately obvious. However, once the occlusion was opened with a stent, the appearance of the vessel just proximal to the stent was suggestive of a dissection or extension of an intramural hematoma.
An overlapping second stent was placed proximally with resultant evidence of proximal extension. An overlapping third stent was placed proximally, and at this point the proximal vessel appeared normal. Her diagnosis was an acute myocardial infarction (MI) secondary to spontaneous coronary artery dissection (SCAD).
[Note: Wearable devices are not approved by the U.S. Food and Drug Administration (FDA) for the diagnosis of acute MI. It's recommended that patients with chest discomfort seek immediate evaluation by health care professionals.]
Definition of Digital Health

The term digital health broadly encompasses the use of digital technologies, such as wearable devices, telemedicine, health information technology and mobile health in health care.1 Mobile Health (mHealth) refers to the use of mobile technologies designed to assist with health care delivery and information dissemination.2,3
These mobile technologies include secure text messaging apps, mobile telemedicine devices, mobile-enabled EHRs, consumer wearable devices such as smart watches, smartphone-based health care apps and mobile-enabled patient portals to access clinical records.
Consumer wearable devices and smartphone-based health care apps have become increasing popular due, in part, to the widespread use of smartphones. A 2019 Pew Research Center survey showed that 81 percent of U.S. adults owned a smartphone,4 and that in 2019, 63 percent of rural America had access to home broadband internet, compared with 35 percent of rural America in the 2007 survey.5
Industry market forecasts reflect the increased consumer interest in wearable devices. One market forecast states that smart wearable device sales will become a $27 billion-plus worldwide market by 2022,6 and another states the wearable device industry revenue will reach $54 billion by 2023.7
Potential Benefits in Cardiovascular Medicine

Remote monitoring and improved access to care. Wearable devices and smartphone-based health care apps cross geographic boundaries and improve patient access to care via remote monitoring and data interpretation. These devices can efficiently connect patients in rural areas with health care services via remote monitoring.
In the 2020s, as artificial intelligence (AI) algorithms and machine learning clinical decision-making support become incorporated into appropriate wearable devices, data may be accurately interpreted and seamlessly transmitted to health care professionals for real-time clinical decision-making.
This may lead to a potential role for appropriate wearable devices in triaging patients to appropriate levels of care, reducing hospital readmissions or emergency room visits, and potentially lead to health care cost saving for patients and the health care system.
Cardiovascular risk factor modification. Wearable devices can enhance self-management of cardiovascular risk factors (blood pressure control, physical activity, dietary/calorie intake and tobacco cessation). At this time, whether this translates into improved cardiovascular outcomes remains to be seen.
Future Perspectives, Potential Barriers to Overcome
Wearable devices have made significant gains in arrhythmia detection and monitoring. However, there are still barriers to overcome in the 2020s before wearable devices can be adopted as standard of care in cardiovascular medicine. Some of these limitations are outlined here.
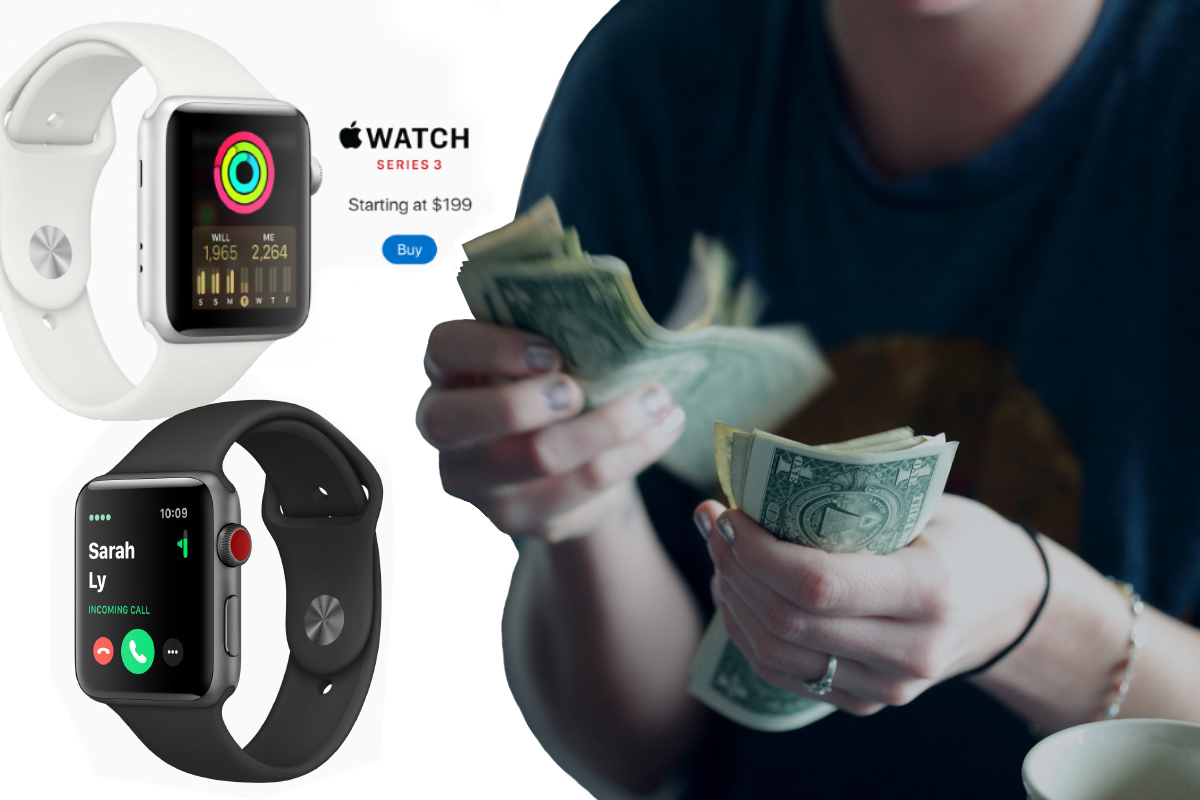
The Digital Divide: Disparities to Access. Often, the population that would benefit the most from so-called home monitoring devices is the same one that is challenged to afford life's basic necessities.
In a 2019 survey, 97 percent of adults with an annual household income greater than $100,000 had a smartphone, 94 percent had a computer, 94 percent had home broadband internet, 70 percent had a tablet, and 64 percent had all four technologies.8
In contrast, 71 percent of adults with an annual household income less than $30,000 had a smartphone, 54 percent had a computer, 56 percent had home broadband internet, 36 percent had a tablet and just 18 percent had all of them.
As we tackle health care disparities in the 2020s, solutions to address this digital divide must be found, especially if wearable devices demonstrate the ability to reduce health care costs and improve cardiovascular outcomes. It is encouraging that while financial cost remains a limiting factor, approximately 80 percent of people who identify as Hispanic or African-American own a smartphone.9
Regulation of Data Collection, Management. Although the FDA provides oversight of mobile medical apps that impact patient safety or transform a mobile device into a regulated medical device such as an ECG machine, cardiovascular professional society input via guidelines and/or consensus statements is needed regarding the collection of clinically actionable data, data management, data monitoring, data analytics with AI and data transmission into the EHR.10

In the 2020s, cardiovascular professional societies may need to develop guidelines or consensus statements to guide the public and health care providers regarding the collection and management of data from wearable devices.
Data Security, Privacy. Currently, the Health Insurance Portability and Accountability Act (HIPAA) does not extend to health information derived from wearable devices. Due to concerns about multiple party access to health data from these wearable devices, data security and patient privacy in wearable devices will need to be appropriately addressed.
Data Overload and Clinician Impact. Extensive adoption of wearable devices creates large amounts of data, which can lead to an excessive clinician burden if not appropriately managed. As we focus on improving work-life integration and reducing clinician burnout in the 2020s, societal guidelines regarding management of clinically actionable data from wearable devices is important.
AI algorithms and machine learning for data interpretation and clinical decision-making can alleviate this problem – and there is progress in this field. In November 2019, the FDA granted 510(k) clearance to Ultromics for its AI-powered echocardiography image analysis system EchoGo Core.2
EchoGo Core is designed to assist clinicians with quantification and reporting of cardiovascular function on echocardiogram, as well as calculation of strain.
What If?

Naomi wonders what would have happened if she had been at home rather than at work. Would she have sought medical attention for her chest discomfort, which was not particularly severe? Would she have convinced herself that her discomfort was noncardiac if she had not owned the Apple Watch? If her MI had been in a different territory, would she have been falsely reassured by the absence of ST elevation on the ECG tracing?
We will never know the answers to these questions. However, the fact is that the life of a 49-year-old female cardiologist may have been saved thanks to information from a wearable device. Just four weeks later, she was in Iceland (photo).
The Decade Ahead: Digital Clinical Practice?
The evolution of wearable devices, their potential role in reshaping clinical practice, and their effect on cardiovascular outcomes will be exciting topics to follow in this new decade.
It's possible that AI-based algorithms will have the capacity to interpret critical findings on wearable devices and trigger emergency services automatically or be transmitted securely for immediate over-read by an appropriate health care professional.
With the advent of augmented reality, mixed reality and virtual reality technologies, digital clinical practice may become a specialty that serves as an initial health care contact service, referring patients to traditional health care facilities only when necessary.
Naomi F. Botkin, MD, FACC, expresses her gratitude to the physicians, nurses and technologists who cared for her during her hospitalization. While they are too numerous to list, she would like to give special thanks to Daniel Z. Fisher, MD, PHD, FACC; Barinder "Ricky" Hansra, MD; and Ramprakash Devadoss, MD, who were responsible for her rapid revascularization.
References
- US Food and Drug Administration. Digital health. July 2019. Available here. Accessed Dec. 19, 2019.
- World Health Organization. mHealth: New horizons for health through mobile technologies: second global survey on eHealth. 2011. Available here. Accessed Dec. 15, 2019.
- Steinhubl SR, Muse ED, Topol EJ. The emerging field of mobile health. Sci Transl Med 2015;7:283rv3.
- Pew Research Center. Demographics of mobile device ownership and adoption in the United States. 2019. Available here. Accessed Dec. 15, 2019.
- Perrin A. Digital gap between rural and nonrural America persists. Pew Research Center, 2019. Available here. Accessed Dec. 15, 2019.
- Lamkin P. Smart Wearables Market to Double by 2020: $27 billion industry forecast. Available here. Accessed Dec. 15, 2019.
- Barkho G. The wearable tech industry is expected to hit $ 54 billion by 2023. Available here. Accessed Dec. 15, 2019.
- Anderson M, Kumar M. Digital divide persists even as lower-income Americans make gains in tech adoption. Pew Research Center, 2019. Available here. Accessed Dec. 15, 2019.
- Perrin A, Turner E. Smartphones help blacks, Hispanics bridge some – but not all – digital gaps with whites. Pew Research Center, 2019. Available here. Accessed Dec. 15, 2019.
- Singh JP. Connecting life with devices. JACC Clin Electrophysiol 2018:422-3.
Clinical Topics: Cardiac Surgery, Congenital Heart Disease and Pediatric Cardiology, Diabetes and Cardiometabolic Disease, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Prevention, Cardiac Surgery and CHD and Pediatrics, Congenital Heart Disease, CHD and Pediatrics and Imaging, CHD and Pediatrics and Interventions, CHD and Pediatrics and Prevention, CHD and Pediatrics and Quality Improvement, Interventions and Imaging, Interventions and Structural Heart Disease, Angiography, Nuclear Imaging, Exercise
Keywords: ACC Publications, Cardiology Magazine, Algorithms, Angiography, Coronary Angiography, Artificial Intelligence, Consent Forms, Coronary Vessel Anomalies, Electrocardiography, Electronic Health Records, Fellowships and Scholarships, Health Services Accessibility, Hematoma, Inpatients, Internet, Mobile Applications, Medical Informatics, Privacy, Medical Records, Schools, Medical, Myocardial Infarction, Stents, Telemedicine, Text Messaging, Thoracic Wall, United States Food and Drug Administration, Vascular Diseases, Walking
< Back to Listings