Pediatric Cardiology Telehealth in Action: How the Pandemic Shaped the Future of Pediatric Cardiology Care Delivery

With the public health emergency (PHE) of 2020, telehealth utilization has increased exponentially. To serve the needs of vulnerable patients who could not be seen in traditional health care environments, providers and patients quickly embraced existing telehealth technology.
Policy makers and payers did their part to support the stressed health care marketplace by becoming more accommodating with technology requirements and reimbursement. Fortunately, the effectiveness and value of this delivery model has become obvious and continued utilization of telehealth services is positioned to be a positive development in the otherwise gloomy legacy of COVID-19.
Pediatric cardiology was no different. Many programs quickly developed telehealth processes that aligned the right technology and right people to provide virtual care to thousands of children across the U.S. Through the experiences of high-performing pediatric cardiology programs, there are several lessons learned and best practices that provide value as the use of telehealth evolves as part of a comprehensive delivery model, whether a pandemic exists or not. Their experiences provide insights into the use of technology, reimbursement, barriers to telehealth utilization, patient identification, scheduling management and telehealth sustainability at a program level.
Program Demographics
MedAxiom surveyed five pediatric cardiology programs that ranged from 11 to 70 cardiologists. Common clinic types where telehealth services are utilized include general pediatric cardiology, heart failure, adult congenital heart disease, electrophysiology, heart transplant, prevention, and syncope. Additional clinic types noted include aortopathy/Marfan's, pulmonary hypertension and fetal health. Common types of providers who provided services via telehealth include cardiologists, cardiothoracic surgeons, advanced practice providers, behavioral health providers, genetic counselors, dietitians, registered nurses and medical social workers.
Use of Technology
Although the initial PHE waivers allowed for a liberal use of technology to provide telehealth services, many programs had to quickly identify the appropriate platform and implement the functionality into their flow. Like electronic health record systems, some platforms were easier to use than others and the following insights were provided by the programs:
- Three of the five programs utilized Zoom technology and found the usability "easy" to "very easy" for general and provider usability.
- For patient usability, Zoom was ranked "neutral" to "very easy."
- Microsoft Teams was utilized by two programs and found to be "very easy" for general and patient usability and "easy" to "very easy" for provider usability.
- Other platforms used were Cisco Jabber, SBR and Haiku, all with varying usability. SBR ranked the lowest but was also only used by one program.
Patient Experience
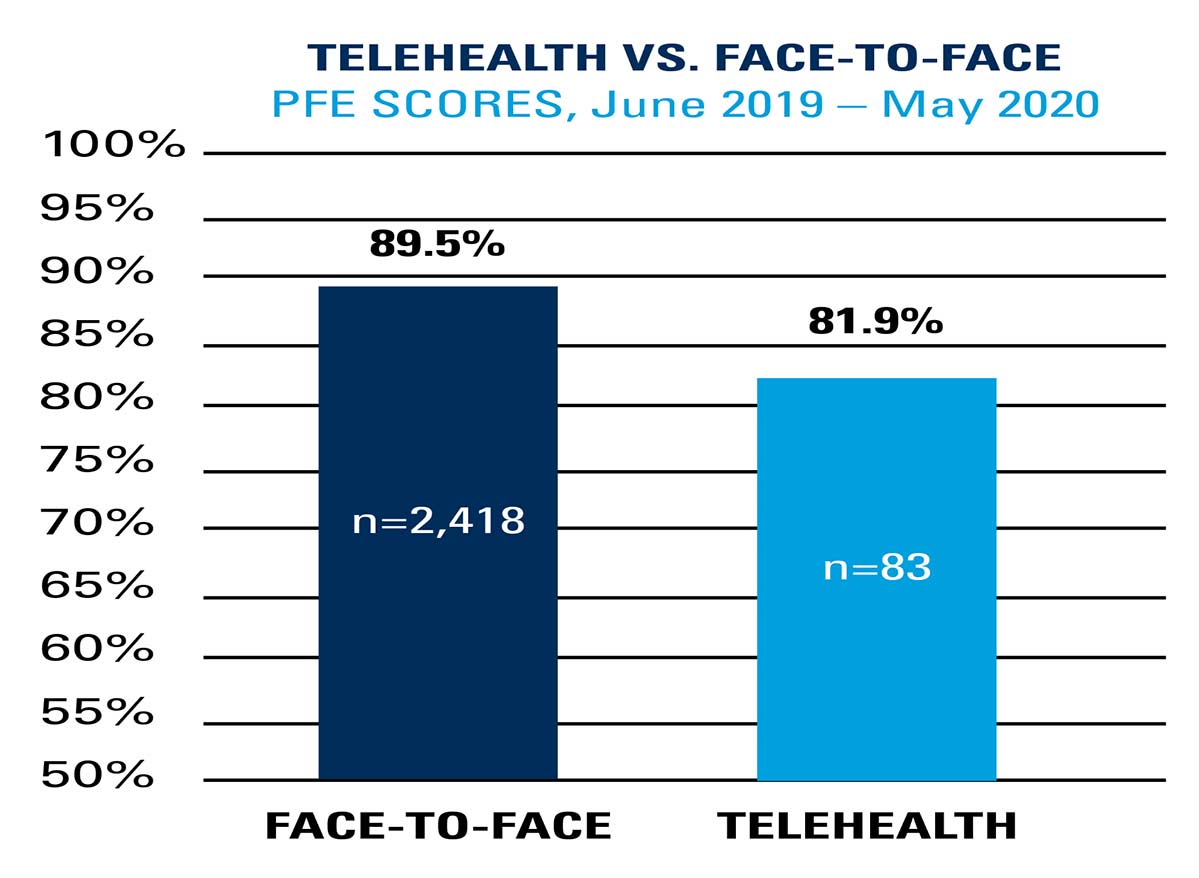
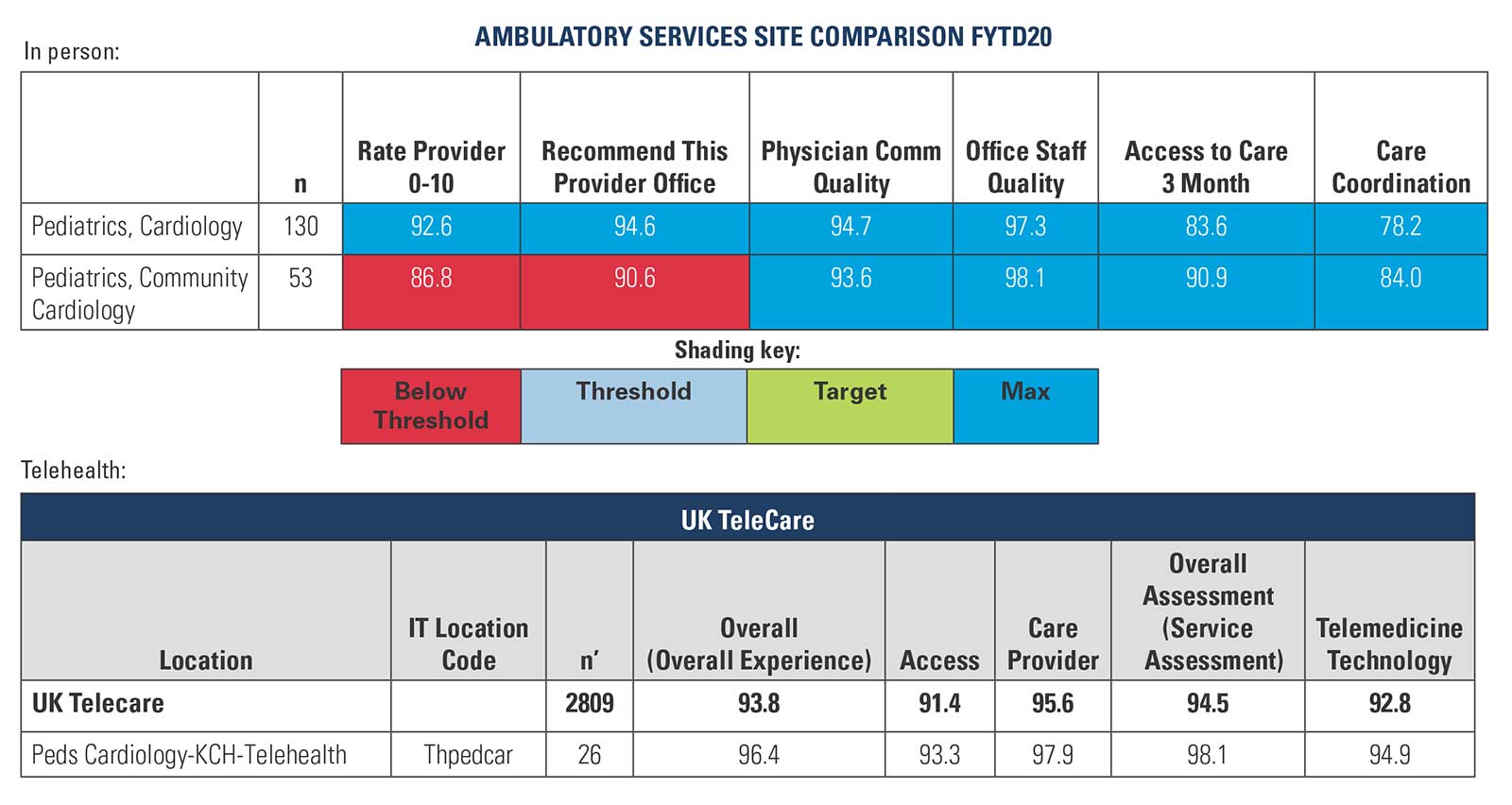
Patient experience is an important outcome of providing telehealth services. The two programs that provided patient satisfaction feedback reported that most patients found these visits highly satisfying. Figure 1 shows good satisfaction for the telehealth services compared with the satisfaction scores of the face-to-face services at Cincinnati Children's Hospital Medical Center. Figure 2 shows a similar trend from Kentucky Children's Hospital, a part of the University of Kentucky.
Telehealth Reimbursement
There was significant support by health care policy makers and insurers to provide reimbursement for telehealth services. During the PHE many of the services were valued as equal to face-to-face visits, which was an unprecedented shift in reimbursement. All five programs noted that they billed E/M services for the telehealth services that included both video and audio options. Three of the five programs billed telephone services for telehealth services that involved only audio options. One common challenge noted from the industry is a decrease in the level of visits billed when transitioned to telehealth compared with the same visit provided face-to-face. Four of the five programs did not notice a difference, while one program did notice a difference with an estimated 10% impact compared to traditional care. As health policy makers and insurers continue to evaluate telehealth service payment, a continued support for these services is crucial for their sustainability.
Barriers to Telehealth Utilization
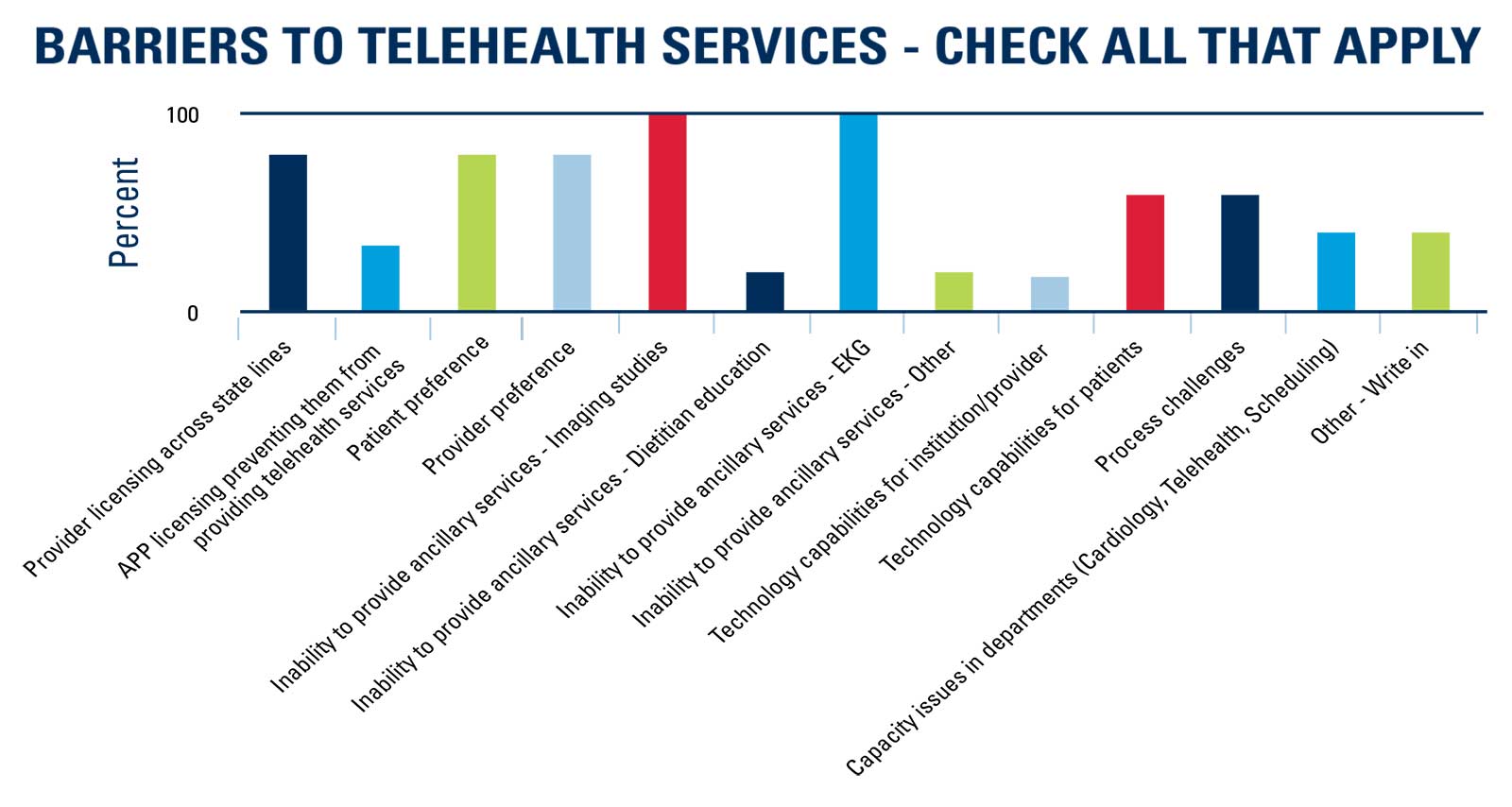
It is important to understand the many barriers to telehealth utilization to develop solutions. Every program surveyed noted that the inability to provide imaging and ECG studies along with the telehealth visit was problematic. In pediatric cardiology, a common practice is to provide diagnostic testing such as echocardiograms, ECGs, rhythm monitoring, exercise stress testing and cardiac magnetic resonance imaging which are often coupled with the visit. The need to de-couple provided a challenge. Several programs noted that they developed diagnostic testing-only clinics or provided patients with the option of obtaining testing in other locations. Others postponed the imaging studies to another time after the appropriate triage of the patient's history and symptoms.
Additional common barriers noted by most programs surveyed were provider licensing across states, patient preference, provider preference, technology capabilities of the patients and process challenges (Figure 3).
Patient Prioritization/Stratification
Certainly, telehealth services will not meet the need of every patient that needs to be seen by a pediatric cardiologist. All five programs noted that they developed a prioritization plan with the most common strategy described as a physician-specific approach where the physicians review the schedule to direct which patients could be provided a telehealth visit. Some programs included other members of the care team as part of the triage process including advanced practice providers and registered nurses.
Telehealth Sustainability
Although all programs had reopened to near capacity at the time of the survey, all five programs were still utilizing telehealth services and had plans for long-term utilization. While most programs had dropped their overall percentage of telehealth visits to below 20%, this is a higher utilization rate than prior to COVID-19 for all programs. Four of the five programs described telehealth services being embedded in their long-term delivery model strategy. However, this is not without challenges. All programs noted a challenge with managing both face-to-face and telehealth visits in the same clinic day and several noted that patient flow was difficult to manage in this hybrid model. On the other hand, three of the programs said they had challenges managing social distancing for the face-to-face visits, which supports telehealth services as a solution for some patients.
Several of the challenges to telehealth are centered around the process. Four of the five programs noted a challenge with patient communication and reschedule management as they transitioned face-to-face visits to telehealth. The process for setting up a telehealth visit due to the added technology has been challenging. Varying methods have been noted but the underlying theme was to standardize the workflow, such as calling the patient to assure appropriate contact information, providing education on the technology and scheduling time. Several programs utilized a registered nurse to begin the visits and manage the consent requirements followed by the provider visit. This process allowed the provider to maintain the typical role and utilize the registered nurse to manage the traditional rooming process only in a virtual format.
Conclusion
The pandemic of 2020 has been tragic and unprecedented, and it is far from over. However, there have been multiple learnings that, if utilized well, will improve the way health care is delivered into the future. Utilization of telehealth services is one of those key learnings. The programs surveyed noted that telehealth was an invaluable tool to provide patient care during the pandemic and most programs plan to include telehealth services as part of their delivery model well into the future.
Programs are figuring out ways to manage through the challenges including ancillary services and diagnostic testing requirements, patient engagement and technology usability. Health care policy and insurers continue to support telehealth services even after the pandemic with several options included in the proposed reimbursement rules for 2021. Pediatric cardiology has embraced expanding health care delivery options and these key learnings will provide valuable insights into how best to maximize telehealth utilization for the future.
Explore this article and other publications at MedAxiom.com/Publications.
Clinical Topics: Cardiovascular Care Team, COVID-19 Hub
Keywords: ACC Publications, Cardiology Magazine, COVID-19, Pandemics, Public Health, Patient Satisfaction, Patient Preference, Counseling, Insurance Carriers, Patient Participation, Workflow, Personal Satisfaction, Social Work, Nutritionists, Triage
< Back to Listings